A beautiful, attractive smile is very important for communication in the modern world. When meeting, it is customary to smile, at least out of politeness, and in moments of joy we involuntarily laugh with our mouths open.
Unfortunately, various pathologies can lead to a noticeable change in the color of one of the central teeth. This significantly reduces the aesthetic perception of the entire smile as a whole. Even one tooth of a different shade involuntarily attracts attention.
Tooth discoloration is a pathological change in color in the area of enamel, dentin, or both. There are two types – external and internal.
External discoloration
The reason is a pigmented plaque that forms on the roughness of the enamel, in microscopic cracks or anatomical cavities. Discoloration of teeth in this case is a consequence of consuming coloring products (tea, coffee, red wine, soda, etc.), smoking, and a reduced level of hygiene. Professional teeth cleaning at the dentist with mandatory enamel polishing, teaching the patient the rules of personal hygiene, and limiting the intake of coloring products will help get rid of it. In some cases, it is possible to use abrasive preparations.
Internal discoloration of teeth
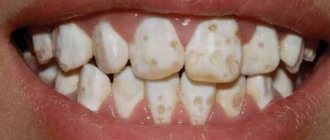
In this case, the color change occurs at a deeper level in the enamel or dentin of the tooth. Whitish erosive spots form on the teeth, which can turn yellow and black over time.
The cause of dental discoloration in this case is the penetration of certain substances into the body. In particular, the increased content of fluoride in drinking water (fluorosis) and the use of tetracycline antibiotics affect it. Violation of mineral and protein metabolism causes enamel hypoplasia - its absence or insufficient development. Age-related changes in the body also lead to thinning of the enamel and, in combination with external factors, yellowing and darkening can develop.
We list the local causes of discoloration:
- “dead tooth” or depulpation (nerve removal). Over time, the tooth becomes darker, grayer, yellower than vital,
- previous root canal treatment using the resorcinol-formalin method. Over time, the crown turns pinkish-brown,
- trauma during the growth of the dental system with the penetration of blood into the mineralization zone,
- Improperly performed orthodontic treatment can damage the ligamentous apparatus (periodontium) of the tooth, resulting in trophic disturbances and loss of vitality.
Internal color changes. Systemic causes.
Genetic defects:
Alkaptonuria is a hereditary disease caused by loss of functions of homogentisic acid oxidase and characterized by a disorder of tyrosine metabolism and excretion of large amounts of homogentisic acid in the urine. Often, patients with alkaptonuria develop pigmentation of the sclera and auricles, which is associated with the deposition of deposits of homogentisic acid in them. The intensity of such deposits may vary. These changes usually do not bother patients, but are one of the signs of this disease that have important diagnostic significance.
In the oral cavity, a bluish discoloration of the crowns of the teeth is observed on 1/2 crowns. There is increased dentin density with a yellow-brown change in the cervical half of the teeth.
Congenital erythropoietic porphyria develops with the birth of a child or in the first year of his life. Sometimes the initial signs of the disease can appear at the age of 3-4 years and older. The disease occurs equally in men and women. Red urine is the initial sign of the disease. Characterized by overdeveloped hair (hypertrichosis, thick eyebrows, long eyelashes), pinkish-brown staining of teeth (erythrodontia) due to the deposition of porphyrins in the enamel and dentin. When examined under ultraviolet rays, teeth give off a bright purple-red glow.
Congenital is a group of hereditary enzymopathies characterized by impaired bilirubin metabolism and manifested by persistent or intermittent jaundice in the absence of pronounced changes in the structure and function of the liver, obvious signs of hemolysis and cholestasis. An increased content of bilirubin in the blood leads to its accumulation and subsequent decay in the tissues of temporary teeth (mainly dentin), causing them to stain in various colors - yellow, greenish-blue, brown. Bilirubin can also influence histogenesis, leading to the development of systemic hypoplasia of primary teeth. The absence of hypoplasia with discolored crowns of primary teeth, which developed as a result of hemolytic jaundice, can be explained by the low titer of antibodies in the mother’s body and the treatment of the newborn with fractional blood transfusions. Over time, the intensity of tooth coloring gradually decreases, which is especially noticeable on the front teeth.
Amelogenesis imperfecta is a severe hereditary disorder of enamel formation, in which the structure and mineralization of both temporary and permanent teeth are disrupted, which leads to discoloration and partial or complete loss of tooth enamel, while dentin remains unchanged.
Amelogenesis imperfecta is divided into 4 main types:
• hypoplastic, • hypomaturational, • hypocalcified, • hypomaturation-hypoplastic with taurodontism.
Treatment of dental discoloration
Aesthetic dentistry has various methods of treating discoloration:
intracanal bleaching – will help restore the light shade of a pulpless tooth,- in-office teeth whitening – brightens and evens out the color of enamel by several orders of magnitude,
- home teeth whitening with trays - can be done at home, but under medical supervision,
- installing veneers on teeth in the smile area will help eliminate discoloration due to internal causes of the body,
- installing a crown made of pressed ceramics completely imitates a living tooth in a row and will hide any defect.
Changes in the color of teeth, or discoloration (the term was introduced into Russian literature by M. I. Groshikov), is one of the reasons for the violation of the aesthetics of a smile. According to ICD-C, the following conditions can lead to discoloration of teeth.
Changes in the color of teeth, or discoloration (the term was introduced into Russian literature by M. I. Groshikov), is one of the reasons for the violation of the aesthetics of a smile. According to ICD-C, the following conditions can lead to discoloration of teeth.
K00.8 Other disorders of dental development K00.80 Change in the color of teeth during formation due to incompatibility of blood groups K00.81 Change in color of teeth due to a congenital defect of the biliary system K00.82 Change in color of teeth during formation due to porphyria K00.83 Change in color of teeth during the process formation due to the use of tetracycline K00.88 Other specified disorders of dental development K03.6 Deposits (growths) on teeth K03.60 Pigmented plaque K03.61 Due to the habit of using tobacco K03.62 Due to the habit of chewing betel K03.63 Other extensive soft deposits white deposits GOAT .64 Supragingival tartar K03.65 Subgingival tartar K03.66 Dental plaque K03.68 Other specified deposits on teeth K03.69 Unspecified deposits on teeth K03.7 Changes in the color of hard tissues of teeth after eruption K03.70 Caused by the presence of metals and metal compounds K03.71 Caused by pulp bleeding K03.72 Caused by the habit of chewing betel K03.78 Other specified color changes K03.79 Unspecified color change
To choose a method for correcting discoloration, it is necessary to correctly determine the cause of its occurrence and assess whether the change in tooth color is permanent or temporary.
Temporary changes in tooth color include discolorations caused by smoking, exposure to food pigments, and mouthwashes. Temporary discoloration of teeth is also caused by the fungus Lichen dentalis and a number of production factors. Temporary discoloration of teeth manifests itself in the form of plaque of various colors and is corrected when plaque is removed by the dentist.
Permanent discoloration of teeth can be congenital or acquired. Permanent congenital discoloration includes “tetracycline teeth,” hypoplasia, fluorosis, discoloration due to incompatibility of blood groups, the presence of a congenital defect of the biliary system, and porphyria.
Permanent acquired color changes include the following types of staining. 1. Vital staining: • age-related changes in tooth color; • staining of tooth tissues filled with amalgam. 2. Devital staining: • due to tooth trauma (hemorrhage into the pulp); • after filling the tooth canal with coloring pastes containing thymol, formalin, iodoform, etc.; • due to the presence in the canal of fragments of metal instruments or pins with signs of corrosion.
Methods for correcting discoloration are determined by the reasons for the change in tooth color. 1. Whitening of living teeth. 2. Whitening of non-vital teeth. 3. Microabrasion. 4. Combined method, when bleaching is used as an auxiliary procedure before making veneers.
How to treat discoloration at home
You can try to remove pigmented yellow and brown plaque with tooth powder or baking soda. The main thing here is not to overdo it and not damage the enamel layer. Highly abrasive pastes must be used very carefully - paste with charcoal can erase the enamel or leave scratches on it. It is recommended to use such toothpastes no more than 2-3 times a week.
There are ways to combat discoloration online using lemon juice and hydrogen peroxide. Most likely, such methods will not harm the teeth, but the effect will be insignificant.
More effective methods are based on a high concentration of hydrogen peroxide or urea. These are various sticks, strips, mouth guards with gel of dubious production from the mass market. These medications often cause tooth pain and sensitivity. These methods are not suitable for treating internal discolorations; you should visit a dental clinic and consult a dentist.
Tooth pigmentation - symptoms and treatment
A doctor can make a diagnosis of “teeth pigmentation” by collecting all the necessary data after a survey and examination. If necessary, additional studies are performed.
In modern medicine, there are not many methods for diagnosing tooth pigmentation, so choosing the right one is not difficult. These include:
- visual inspection of clinical manifestations;
- radiography - allows you to evaluate the internal structure of the tooth and identify deviations;
- computed tomography (CT) is a fairly modern research method that is beneficial for both the doctor and the patient (the doctor receives a higher quality image, and the patient receives approximately 90% less radiation); allows you to study the image in 3D format and monitor the dynamics of treatment;
- microscopy - magnifies the area under consideration approximately 25 times, makes it possible to study the structure of the enamel and the extent of the lesion;
- rheodentography - allows you to determine the functional abilities of the pulp, as well as assess the depth of the lesion;
- electroodontodiagnosis is a method of studying the condition of the pulp and periodontium (soft tissues surrounding the root of the tooth) using a dosed electric current that affects the nerve without damaging the tissue membrane of the pulp [8][9].
As a rule, to diagnose ordinary pigmentation, it is enough only to collect complaints, an anamnesis (history of the disease) and a visual examination. Doctors resort to more serious studies, such as CT scanning and a microscope, in case of deeper lesions of the dental cavity and periodontium.
To choose the right treatment method, it is very important to establish a correct diagnosis and not confuse a pigment spot with caries. The latter, unlike dark pigmentation, has a cavity bottom that is not only dark, but also loose.
Superficial caries must also be differentiated from a whole group of non-carious tooth lesions, such as enamel hypoplasia, fluorosis, wedge-shaped defect, erosion and necrosis of hard dental tissues.
With caries, the spot is most often a single one. It is localized in the grooves on the chewing surface or one of the contact surfaces (between the teeth), less often on the neck of the tooth. With hypoplasia and fluorosis, the spots are multiple and localized in places atypical for caries: areas of the labial (cheek) and lingual surface of the tooth crowns.
Spots with hypoplasia are usually white with clear boundaries and have a smooth and shiny surface. They are located at the same level of the crowns of several symmetrically located teeth.