Tooth abrasion ( Abrasio dentium) is understood as the loss of hard dental tissues (enamel, dentin, root cement) under mechanical influences. In this case, a distinction is made between physiological and pathological (increased) tooth abrasion .
Physiological abrasion is observed after teething and is a continuous process due to constant contact of the surfaces of the teeth (mainly when chewing food; on average, 1-1.5 thousand contacts per day). The loss of hard tissue is insignificant (0.03-0.04 mm per year), although in old age it may already be noticeable, and there are no pain symptoms.
Pathological tooth abrasion is characterized by excessively intense (increased) and too early loss of hard dental tissues, and can be observed on one tooth, or, more often, on a group of teeth, up to all teeth ( generalized tooth abrasion ). This form of non-carious dental damage is quite common (statistically, it is more or less pronounced in 12% of people) and requires mandatory treatment to prevent loss of dental tissue and subsequent complications.
Signs of increased tooth wear
In the early stages, a symptom is the appearance of increased sensitivity of the teeth, especially to temperature changes. Later, pain is felt due to chemical (for example, vinegar, citric acid) or mechanical (for example, brushing teeth) irritation.
Symptoms of pathological abrasion of teeth can be observed in the horizontal or (much less frequently, and in combination, for example, with symptoms of erosion, wedge-shaped defects) vertical direction, as well as in a combination of these directions.
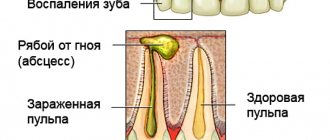
The pathology affects both enamel and dentin, but after the enamel is erased, the process proceeds more intensely, because dentin tissue is softer. As a result, sharp, traumatic enamel edges are formed along the edges of the teeth, and the teeth are shortened. There may be external signs of changes in the lower part of the face (for example, folds in the corners of the mouth), injuries to the temporomandibular joint and tongue, and even hearing impairment.
Causes
A wedge-shaped defect is considered as an independent disease only in domestic dentistry. Abroad, there is a detailed classification of non-carious pathologies depending on the form, origin and clinical picture. Due to the fact that there are several reasons for the development of pathology, the following types of wedge-shaped dental defects are distinguished.
Wedge-shaped defect of abfraction nature
Develops due to malocclusion and pathological closure of the upper and lower jaws. As a result of this process, increased stress occurs on the root region, which leads to the formation of a characteristic cavity. Some researchers consider the parafunction of the tongue (excessively strong pressure on the inner surface of the dentition) to be the main cause of the abfraction defect.
The defect may appear due to bruxism.
Abrasive
The defect in this case develops due to exposure of the teeth to abrasive materials. These include various whitening agents and tartar pastes, as well as brushes with stiff bristles. Often the problem occurs due to improper brushing of the teeth, especially when using horizontal brush movements during the procedure.
Erosive
This type of pathology occurs due to the effects of chemicals on the teeth. As a rule, these are medium-strength acids that are found in many foods (fruits, vegetables, juices and wine drinks). Often, a wedge-shaped defect of this nature is diagnosed in patients with chronic gastritis or ulcers, since gastric juice regularly enters the oral cavity. People working in hazardous industries are also at risk.
It is not recommended to brush your teeth within an hour after consuming highly acidic drinks or foods. This can lead to leaching of calcium from the surface layer of enamel.
Classification of tooth abrasion (pathological)
There are a number of generally accepted classifications of pathological tooth abrasion , which have been and are used by dentists at different times.
| Classifying factors | Clinical manifestations |
| Clinical and anatomical | Three degrees of abrasion (incisal edges and tubercles of the crown parts of teeth to a small extent; enamel from the tubercles of all teeth and cutting edges of teeth up to the surface layers of dentin; enamel and dentin tissues up to the cavity (crown) of the tooth). (Groshikov M.I.). |
| By degree of erasure | Four degrees of abrasion (enamel tissue from cutting cusps and edges; cusps to dentin and reduction of the crown by a third; reduction of the crown by two-thirds; reduction of the coronal part to the level of the neck of the teeth). (Bracco, Bracco). |
| Functional-morphological | Depth of damage to the coronal part (three degrees: 1/3, 2/3, more than 2/3 of the crown). Stage of damage (three stages: damage to enamel, enamel and partially dentin, damage to dentin). Surfaces (horizontal, vertical, mixed). The lesion is localized or generalized. (Prof. M.G. Bushan, considered the most complete classification). |
| According to the degree and form of abrasion | Four degrees (within enamel tissue and partially dentin; within dentin tissue without visible translucency of the dental cavity; within replacement dentin with visible translucency of the cavity; abrasion and damage to the entire coronal part). Form of abrasion (horizontal or vertical planes, stepped form, mixed forms, etc.). (Prof. A. G. Moldovanov and L. M. Demner, based on long-term clinical observations and is considered the most modern). |
Causes of increased tooth wear
The causes and factors leading to pathological tooth abrasion can be very diverse. Quite often, tooth wear is caused not by one factor, but by a combination of reasons. But all the causes of this pathology can be formally divided into four groups:
- increased abrasion due to excessive contact of teeth with each other (attrition; from Latin arrtitio = mutual friction)
- increased abrasion due to specific external (mechanical) effects on hard dental tissues (demastikation; from Latin masticare = chewing)
- insufficient hardness of dental tissues
- combinations of the above factors.
Insufficient hardness of dental tissues. It may be a consequence of systemic dental (for example, dental fluorosis, enamel erosion) or internal (for example, hormonal-metabolic) pathologies and diseases. Recent studies show that increased tooth wear may be a kind of “marker” of the presence of hormonal disorders.
Bruxism (teeth grinding). It is considered the most common cause of increased wear of hard dental tissues. Most often it occurs unnoticed and at night, and has a stressful basis. As a result of systematic bruxism, the frontal teeth and their cutting edges are primarily affected.
Incorrect teeth brushing technique. Constant use of an excessively hard toothbrush and toothpastes with a high content of abrasive components (for example, to lighten teeth at home).
Anomalies of dentition. Basically, the cutting edges of the frontal and chewing surfaces of the lateral teeth are subject to increased abrasion. Similar factors include incorrect orthopedic structures or the absence of several teeth, which leads to increased stress on the dental surfaces.
Professional factors. They can appear in work areas with a high content of abrasive microparticles in the air.
Prevention and treatment of wedge-shaped defect.
Correction of nutrition, elimination of traumatic factors - excessively hard and abrasive food, harmful environmental factors - dust, gas contamination, correction of liquid intake, exclusion from drinking acidic juices and carbonated drinks containing organic (citric acid) and inorganic (phosphoric acid) drinks such as Cola, Pepsi, Fanta, Sprite, energy drinks with sucrose, glucose, ascorbic acid and caffeine.
Quote:
Energy drinks have the greatest buffering capacity, which means they disrupt the acid-base balance in the mouth more than others.
According to scientists, after drinking an energy drink, erosions occur on the enamel, which can lead to the development of caries. Regular and diet carbonated drinks, and even iced tea (meaning a synthetic drink with the addition of organic acids) also do not benefit enamel. It would not hurt the reader (with wedge-shaped defects of teeth - I strongly recommend) to read the article “On the choice of toothpastes for sensitive teeth.”
Special toothpastes and preparations that reduce tooth sensitivity To patients with a tendency to develop wedge-shaped defects, enamel erosion, multiple caries, I dedicate the article Correct dental pastes for problem teeth!
Medical stages of prevention and treatment of wedge-shaped defects:
As I have already said, a wedge-shaped defect is a polyetiological disease; accordingly, treatment and prevention cannot be reduced to symptomatic-causal “covered with fluoride varnish, put a filling”; this is not scientifically based shamanism and does not eliminate the cause of the appearance and development of hard tissue pathology. Treatment should be comprehensive and multifaceted:
- identification and elimination of parafunctions of the masticatory apparatus, elimination of bad habits and reprogramming of masticatory functions,
- normalization of the bite, including full-fledged rational and competent prosthetics, which implies restoration of the functionality of the dentition, occlusal relationships of the jaws,
- identification and correction of premature dental contacts, selective grinding of occlusal surfaces and cusps of premolars and molars according to Jenkilson,
- production of uncoupling medical dental guards and bite correction using orthodontic and orthopedic methods
.
As a rule, the final stage of treatment of a wedge-shaped defect is the elimination of symptoms - treatment of damaged areas with remineralizing compounds containing soluble calcium compounds, phosphates, in the form of applications to the surface of the teeth for at least 2-3 weeks, followed by treatment of mineralized surfaces with fluoride preparations and desensitizers.
And only after eliminating all the factors that caused damage to the hard tissues of the tooth can the issue of the manifestation and progression of the wedge-shaped defect be closed. Usually, with pronounced defects, this is carried out under anesthesia, a bevel is created on the adjacent areas of the enamel, some authors recommend additionally creating retention points in the dentin, closer to proximal surfaces of the tooth.
Technique for performing restoration of wedge-shaped defects and know-how from personal experience.
Retraction of the gums with a thread
It is necessary to retract the gums and create (if possible) roughness of the enamel of the gingival area, if it is preserved.
If possible, it is imperative to use a rubber dam as an insulating curtain, ideally.
Below I will describe a situation where the application of a rubber dam or isolation with a liquid rubber dam is not available (there are no conditions available or there are no conditions for clamp fixation of the rubber dam). The information is aimed at specialists.
Technical features of work in the treatment of wedge-shaped defect
Let's get started, about preparation and features of formation it is written a little higher. Total-etch technique, adhesive preparation, preferably filled with one-component adhesive (I recommend PQ-1, OptiBond FL, Gluma Comfort Bond & Desensitizer), (I do not recommend self-etching adhesive systems due to the low level of adhesion in such a difficult and problematic area), on Place a composite insulating material at the bottom of the wedge-shaped defect, for example SDR (Dentsply DeTray), Filtek Bulk Fill Flowable Restorative (3M-Espe). At this stage, the treatment of minor wedge-shaped defects (after fluoridation of the restoration surface) can be considered complete.
Restoration of a wedge-shaped defect
In the case of deeper wedge-shaped defects, with a pronounced loss of hard tooth tissue, cover the surface of the composite insulating material with a thin layer of flowable composite, slightly blowing it over the surface of the defect with a stream of air from a blower.
Excess material should close (overlap) the retraction thread in the gingival sulcus and come to the surface of the gum (see photo above), then they can be easily removed with a probe after polymerization of the entire restoration. It is important.
Add and carefully adapt the restoration material in a thin layer, polymerize in a pulsed mode with a laser LED polymerizer, add an opaque shade of the restoration material, polymerize in a pulsed mode, the restoration is completed with a thin layer of enamel shade.
Completed restoration of a wedge-shaped defect of the lower premolars
Treatment of a wedge-shaped defect restoration, polishing features.
The contouring of the restoration is carried out with a moderately wide carbide cylindrical bur, a well-centered turbine with abundant water cooling to prevent overheating of the thin layer of restoration material. Use a carbide bur with a sharp tip to walk along the gingival perimeter of the restoration, carefully remove the retraction cord, and carefully grind off excess material and the remains of the polymerized adhesive. Use a probe to remove excess materials from the gingival surface. Complete the polishing of the restoration surface with rubber cones with finely dispersed diamond filler, with mandatory water cooling, at low speeds. Cover the surface of the restoration with fluoridating compounds and protective varnish. Finita!!!
Preliminary preparation for high-quality restoration of enamel abfraction or wedge-shaped defect.
Particularly relevant is preliminary preparation - the elimination of marginal periodontitis, gingivitis, and restoration measures must be carried out only after professional oral hygiene. We professionally clean your teeth and treat periodontal disease!
In the presence of inflamed, bleeding, oozing gums and tartar deposits, any “filling-a-la-filling” is doomed to failure; the restoration will not last even a week, in the worst case, under it (“filling type”)
Secondary caries will certainly develop. Neither super-cool material nor ultra-reliable and extra-expensive adhesive will save you.
Treatment of increased tooth wear
General treatment of pathological tooth abrasion is individual and is aimed primarily at eliminating the factors that cause this pathology (including the treatment of internal pathologies that lead to a decrease in the strength of hard dental tissues).
The nature of dental treatment depends on the stage at which the disease is diagnosed. In the initial stages, it is usually sufficient to use preventive measures, for example, training in the correct technique for brushing teeth, selecting the right toothpastes, periodic remineralization and fluoridation of teeth in a dental clinic, wearing special night guards and psycho-neurological assistance for bruxism, bite correction, etc. . For deeper lesions, it is necessary to restore lost dental tissues by filling and microprosthetics, installing dental crowns and dentures.
The prognosis for treatment, especially in the early stages, is considered favorable, but in order to avoid relapses, constant monitoring by a dentist is necessary.
Request a consultation
Definition of disease
Wedge-shaped dental defect is a chronic disease in which the enamel in the cervical area of the tooth becomes pathologically thinner. The lesions have a characteristic cone- or wedge-shaped shape, with the apex of the cavity always facing the gums. In dentistry, this disease is classified as a group of non-carious defects. The prerequisites for development are revealed quite early, even during adolescence.
A wedge-shaped defect occurs in 20-25% of middle-aged and elderly people.
The cavity in the tooth formed due to a wedge-shaped defect usually has a smooth and shiny surface. At the initial stages of development, it does not differ from the natural color of the enamel. Pathology can develop on any tooth, but is more often diagnosed on incisors, canines and premolars (3-5 teeth of the upper and lower jaw). Depending on the extent of the pathology, a single or multiple wedge-shaped defect is distinguished (in this case, symmetrical teeth are affected).
In the later stages, a wedge-shaped defect leads to destruction of the root region of the teeth and provokes the development of periodontal disease. Read more about the causes of periodontal disease here.