Main signs indicating that there is a dental problem
If there is a problem with teeth, an inflammatory process has begun, can a tooth cause a sore throat? Yes, it can, because painful sensations are easily transmitted to the mucous membrane of the throat and larynx, since there is no border between them.
When a cyst (flux) appears, severe swelling and swelling may occur in the area of the diseased tooth. In such cases, the purulent inflammatory process is quite strong, so the pain is transmitted to the throat, ears and even temples. The same problem is characterized by an increase in body temperature.
In addition, along with a sore throat, swelling may appear; teeth on one side or one tooth and the affected area around it may hurt.
In the absence of obvious signs of a cold, such as a runny nose, mild headache, cough, one can almost certainly suspect the presence of a dental problem.
Dental pathologies
Sore throat is also caused by various diseases associated with poor dental care.
Periodontitis and galvanic syndrome
Inflammation of the gums, called periodontitis, is caused by bacteria entering the gum canals. The causes of the problem may be hidden in the active growth of tartar or in the predominance of soft foods in the menu, which reduces the load on the gums. Weakened gums result in an inability to resist attacks from pathogens. The treatment process begins with cleaning the gum canals and regular rinsing with antiseptic solutions. In most cases, this is enough for a quick and complete recovery.
If a person has a sore throat due to periodontitis, and instead of seeking qualified help, a person self-medicates, he or she runs the risk of experiencing pulp inflammation and serious tooth decay. As a result, it will not be possible to avoid visiting the doctor’s office, and the treatment process will take much more time, effort and financial expenses than in the first stage of the disease.
A tooth that has been extracted can also cause problems. Dentures made of metal create small currents. For the delicate oral mucosa, they are enough to initiate an inflammatory process accompanied by pain. Gradually, the pathological process takes over larger areas, spreading from the gums to the throat. Getting rid of the cause of the pathology is simple - remove the prosthesis. Next, the patient will need treatment using immunomodulators to restore damaged tissue. After the course of treatment, the dentist recommends that the patient wear ceramic dentures.
Aphthous stomatitis
The presence of chronic diseases of the gastrointestinal tract, vitamin deficiency, lack of necessary oral hygiene or smoking lead to the development of aphthous stomatitis. Its main symptoms are sore throat, erosion, inflammation of the lymph nodes and fever. Experts do not exclude the possibility of developing aphthous stomatitis under the influence of a viral infection, but prefer to believe that the root cause of the pathology is a malfunction in the functioning of the immune system. Another reason for the appearance of pathology is the use of low-quality dentures.
Erosion or aphthae that appear have a red border and a white coating. The presence of erosion causes a strong burning sensation, which intensifies when eating. In most cases, aphthae affect the oral mucosa en masse, located on the inside of the lips, in the throat, on the tongue and cheeks. The patient needs to contact the dentist to prescribe a course of treatment. The opinion “I can wait until everything goes away on its own,” which appears in many adults, leads to massive aphthae and severe sore throat. The treatment process involves treatment with antiseptic solutions, taking vitamin complexes, antihistamines and sedatives. The success of therapy lies in an integrated approach. It is possible to avoid relapses only by eliminating chronic diseases and regularly taking medications like Dekaris prescribed by a specialist.
Temporomandibular joint
Can a tooth cause a sore throat? Maybe if there are problems with the functioning of the temporomandibular joint. This joint is a movable joint (discontinuous) that connects the lower jaw and the base of the skull. Such problems occur at the level of functional pathologies, which can arise against the background of spatial disturbances and are associated with muscle tissue. It is possible that the patient has problems closing the jaw. Such problems not only lead to a sore throat, but also often interfere with speaking and even breathing normally.
In addition, if the functioning of the temporomandibular joint is impaired, then the pain can be characterized as migrating. Simply put, at first it seems that your teeth hurt, then your throat, then your throat, then your neck, and so on. It may seem as if there is a foreign object in the throat, sometimes there is dizziness and pain even in the neck and back. When chewing food, lumbago may occur.
This type of pathological process requires medical intervention. At the initial stage, you can use Rotokan, which will reduce pain.
Why does pain go away on its own?
A reduction or complete cessation of toothache without outside intervention in most cases indicates the transition of the carious process from an acute to a chronic stage. The sequence of changes occurring in the tooth:
- Caries at the spot stage - damage to tooth enamel does not cause pain.
- Superficial caries - tooth sensitivity to temperature and chemical stimuli appears, sometimes pain does not occur.
- Medium caries - the upper layers of dentin are affected. The pain becomes more intense and lasts longer, and a carious cavity appears.
- Deep caries is the spread of the carious process into dentin to its entire depth. When food, cold and hot drinks get into the carious cavity, quite severe pain appears, which goes away after the irritant is eliminated. At the last stage of development of deep caries, aching pain persists for a long time even after the removal of the irritating factor - signs of pulpitis appear.
- Development of acute pulpitis. Since the pulp is penetrated by a large number of nerve fibers, when it is damaged, patients experience severe paroxysmal pain, worsening at night. Pain can occur either under the influence of external stimuli or independently.
- If purulent inflammation occurs, lumbago and pulsation are felt in the tooth; the pain becomes constant and difficult to bear without the use of painkillers. Body temperature rises to 38°C.
- Transition of acute pulpitis to chronic.
Stages of pulpitis transition:
- Fibrous pulpitis – pain is pronounced when eating cold food; their peculiarity is that they do not appear immediately after exposure to cold; They pass the same way, not immediately, but after a while.
- Hypertrophic pulpitis - granulation tissue grows in the pulp; pain is not felt in this form of pulpitis; during eating, blood often appears from the carious cavity.
- Gangrenous pulpitis - the pulp dies, pain in the tooth appears only when exposed to hot temperatures and quickly disappears.
The transition of the inflammatory process beyond the apex of the tooth root, the development of acute periodontitis. Mild aching pains occur, which gradually become more intense: purulent inflammation develops.
- Fibrous form - patients do not show any complaints: there is no sensitivity to hot or cold temperatures, percussion (tapping on the tooth) is painless.
- Granulating form - manifested by mild pain in the form of a feeling of fullness, mild pain when biting; bone tissue is thinned out. A fistula periodically appears on the gum; after the purulent contents are evacuated, it disappears.
- Granulomatous form - is asymptomatic, very rarely mild pain may occur when biting. A granuloma forms at the apex of the tooth root, which can only be detected by x-ray diagnostics; destruction of bone tissue and tooth tissue occurs at the apex of the root.
Thus, with the development of chronic periodontitis, pain disappears, and patients may decide that if the pain has passed, then the tooth is cured. But this is a mistake that leads to the development of severe complications.
If you had to remove a figure eight that continued to cut painfully, the rehabilitation period is accompanied by an attack of sore throat. It is important to understand the reasons for this deviation from the norm:
- Proximity to the trigeminal nerve. If its integrity is violated, the hole begins to hurt, and increased salivation provokes an additional attack and a feeling of general discomfort.
- When cutting the gums, the throat also hurts, but in fact the source of discomfort is the open wound. The procedure is complex, so the rehabilitation period is delayed for an indefinite period of time.
- If the repaired molar has begun to cut, it is especially problematic to remove it without complications. The doctor first needs to cut the bone that is preventing the growth of the figure eight, and then remove it with special dental forceps.
- If the root is damaged, the lymph node may become inflamed. A dangerous condition that requires immediate correction. If the general condition is not stabilized, after resection of the third molar, the unpleasant sensation in the mouth will only increase.
Why might a sore throat appear after tooth extraction?
This is due to various reasons:
- Firstly, a sore throat and pain could have existed before, but after dental surgery they only intensified.
- Secondly, pain may be observed not as a result of a throat disease, but as irradiation of pain from an extracted tooth. This is the most common cause of pain in the oropharynx after dental treatment.
Painful sensations often appear as a result of the patient being in an uncomfortable position in the dentist’s chair for a long time - with his head thrown back and his mouth wide open. The muscles of the neck and jaw get tired, the mucous membrane dries out - all this contributes to a sore throat after tooth extraction.
It is rare, but it does happen that a doctor can accidentally damage the mucous membrane with instruments. The resulting abrasion or wound causes pain when swallowing.
All these reasons lead to pain immediately after visiting the dentist. However, a sore throat may occur after a few days.
What is the reason for this condition? If there is a chronic infection in the body, or treatment was carried out against the background of some acute inflammatory process, or teeth with deep caries were removed, this can lead to the spread of infection to the mucous membrane of the throat. A sore throat, paratonsillar abscess, abscess or phlegmon of the jaw develops.
- Firstly. The sore throat and pain could have been there before, but after dental surgery they only intensified.
- Secondly. pain may be observed not as a result of a throat disease, but as irradiation of pain from an extracted tooth. This is the most common cause of pain in the oropharynx after dental treatment.
Sore throat after tooth extraction due to long-term manipulations
Your opinion is very important to us
Discussing: 17 people
Teething in childhood
Can a tooth cause a sore throat in a child? The process of development of a child’s body is very complex and individual for each child. However, there are general trends that are characteristic of all children.
On average, teething occurs between 4 and 7 months after birth. And the symptoms of teeth appearing are completely diverse. Some children don’t worry at all, and parents only accidentally discover their baby’s first teeth. Other kids have a hard time with this process: they cry, sleep poorly, and chew on all the objects they get into their hands. Some children even experience a runny nose, cough and redness of the throat. Naturally, at this age a child is not able to tell what is bothering him, but a red neck can also indicate unpleasant sensations in this area.
It is not worth interfering with this process or treating the baby if his discomfort goes away after a few days.
Effective treatments
Ordinary medications sold in pharmacies without a prescription will help relieve pain. These include Tylenol (acetaminophen) and Advil (ibuprofen). For oral rinsing, doctors most often suggest a chlorhexidine solution. This product will help keep your mouth clean and disinfect. If both your tooth and throat hurt, then if such a solution is not available, you can also use warm salt water or dilute hydrogen peroxide in certain proportions. In some cases, additional antibiotics will be required. For drugs taken orally, Erythromycin or Amoxicillin tablets are suitable.
However, more often the doctor recommends the removal of wisdom teeth as an effective treatment measure. This method is guaranteed to solve all problems associated with inflammation and stop the spread of infection. Sometimes a periodontal abscess develops so rapidly and severely that it becomes necessary to use emergency hospitalization services. A high probability of developing a similar scenario appears with a tumor of the lymph nodes. If wisdom tooth removal is not planned, the dentist can remove the source of inflammation instead. However, this method does not guarantee that the tissue will not regrow and create the same problem in the future.
Gingivitis and pericoronitis
Can a wisdom tooth cause a sore throat? This is the most common cause of pain in the throat area. In this case, discomfort can spread to other areas of the face, ears and temples, and is especially felt while chewing food.
This is due to the fact that wisdom teeth are located near the masticatory muscle and lymph nodes, and the tonsils and the back wall of the pharynx are also located in the rows.
Increased pain may be due to the fact that a bacterial infection begins to develop in the tooth, which gets there with food. More precisely, it gets into the area between the gum and the tooth, and an inflammatory process called pericoronitis begins.
Due to poor oral hygiene, gingivitis, that is, inflammation of the gums, can appear.
Gingivitis and pericoronitis can lead to the development of tonsillitis or inflammation of the tonsils. If the eruption of wisdom teeth is disrupted, it is recommended to immediately consult a dentist; in addition to removal, it is possible that you will also have to undergo a course of antibiotic therapy.
Teeth eruption and removal
If the tooth grows incorrectly, damage to the mucous membrane occurs. In the resulting pocket, food particles begin to accumulate, which turn into a favorable environment for the proliferation of pathogenic microorganisms. An inflammatory process begins, requiring immediate surgical intervention. Removing the pus does not solve the problem, but it reduces the risk of complications by allowing the tooth to erupt.
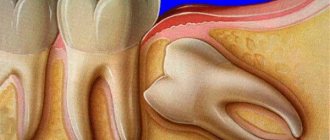
The greatest inconvenience is caused by wisdom teeth. By the time they appear, there is no longer any free space in the jaw, so they have to “move” those teeth that have already become a part of a person’s life. The process is slow, accompanied by severe pain, causes gum swelling, and fever. The inflammatory process often begins, the pain intensifies, radiating to the throat or ears. The lack of adequate treatment leads to the involvement of the tonsils in the fight against infection. When both teeth and throat hurt, be sure to prescribe antiseptic rinsing solutions, for example Miramistin or Furacilin. If the pain is severe, the specialist will prescribe painkillers. Independent choice of such drugs when suffering from toothache can cause complications:
- bleeding;
- allergic reaction to the main drug of the drug course;
- weakening the effect of other medications taken or provoking their side effects.
Even replacing prescribed medications with analogues is dangerous. In severe cases, when the throat and teeth hurt, it is necessary to use antibacterial drugs. Until the infection is suppressed, the problematic tooth is not removed due to the risk of infection entering the open wound.
Removing any tooth comes with risks. Neglecting the recommendations not to smoke, not to eat, not to drink, and to rinse the mouth thoroughly in the first few hours after surgery can cause infection to enter the wound. Then, in addition to the gums, the person may also have a sore throat. Sore throat after tooth extraction and without pathologies. It's all because of the difficult surgery. Damage to a large number of nerve endings some time after tooth extraction provokes pain that radiates to different parts of the oral cavity. It is enough to follow the doctor’s recommendations, and the problem will disappear on its own.
Periodontitis
Does your throat hurt when your wisdom teeth come through? Yes, this is possible, especially if periodontitis has begun to develop. This pathology is a consequence of gingivitis. With periodontitis, in addition to bleeding gums, when brushing your teeth, their color changes. This is actually a buildup of bacteria from food debris, also called plaque.
At an early stage of the disease, detachment of teeth from the gums may occur, that is, small pockets appear where bacteria accumulate and actively multiply. As a result, teeth begin to lose their bone base and weaken. Later, if the patient does not fight the problem, degradation of the connective tissue occurs and the teeth begin to loosen. At this stage, a person feels severe pain in the process of digesting food, and there is a constant unpleasant taste and smell in the mouth. Pain begins to spread to nearby tissues, including the throat area.
Lack of treatment for periodontitis is a direct path to the loss of all teeth.
If you have a sore throat, your teeth may hurt
Every person has felt pain in their gums at least once in their life.
This problem occurs due to many reasons, and sometimes it can be quite difficult to get rid of it. In today's article we will look at the causes of pain in the gums, why they hurt during a cold, and how to treat this disease. Since all body systems form one whole, toothache during a cold is not a surprising phenomenon, the causes of which may be:
- the formation of pressure in the nasal sinuses, which are connected through nerve tissue to the oral cavity. A similar problem arises with sinusitis - inflammation of the largest nasal sinuses (maxillary sinuses);
- consumption of large amounts of acid-containing liquids (cranberry juice, tea with lemon), which have a harmful effect on tooth enamel;
- taking medications, including syrups. Cold medicines contain acid, and syrups contain sugar, which have a negative effect on teeth;
- nasal congestion, which causes the mouth to dry out, which increases its acidity, causing tooth pain;
- an intestinal disorder seen with a severe cold. During the course of the disease, vomiting processes occur, after which (if you do not rinse your mouth) a large amount of acid settles on the tooth enamel;
- inflammation of the trigeminal nerve, which causes loss of sensation in the jaw. At the same time, completely healthy teeth can ache.
Features of symptoms
The inflammatory process affecting the trigeminal nerve may be accompanied by swelling of the face on the affected side and pain in the jaw. At the same time, it is painfully difficult to chew, swallow, and speak.
But it could be worse
Even more pain can result from blockage of the maxillary sinuses, that is, sinusitis.
In this case, purulent sacs may form on the gums, which inflame the root of the tooth and the pain becomes much stronger.
Please note that dental plaque, which can provoke inflammatory processes, appears within a couple of hours after brushing your teeth.
It is a mixture of a water base, saliva salt and bacteria. All microorganisms and bacteria that live in the mouth appear precisely because of dental plaque.
Therefore, to prevent dental problems and inflammation, it is necessary to brush your teeth regularly.
Inflammation of the gums with sore throat
Inflammation of the gums with sore throat occurs due to the fact that inflammatory processes occur in the body, and sore throat, that is, inflamed tonsils, is directly related to the mouth and throat.
Let's look at the symptoms of gum inflammation with sore throat:
- The mucous membrane of the mouth becomes red.
- The temperature rises and the patient begins to feel unwell.
- It is difficult to eat because everything in my mouth hurts.
- A very unpleasant odor appears from the mouth.
- The gums swell and salivation increases.
- A gray plaque forms on the gums, which causes teeth to become loose.
Inflammation of the gums with sore throat requires immediate treatment, and the entire recovery process must be under the supervision of a doctor. The main task is to eliminate sore throat, that is, the cause of inflammation. After this, treating inflamed gums is much easier and more effective.
Inflammation of the gums due to a cold
A cold is a rather unpleasant condition, but inflammation of the gums during a cold is a double problem. You can tell if your gums are inflamed from a cold by looking at several symptoms. The main symptom of inflammation is acute toothache, redness in the mouth, swelling and swelling of the gums.
There are several causes of gum inflammation due to a cold. Very often, the gums become inflamed due to a viral infection, that is, inflammation of the trigeminal nerve. This creates the feeling that not only the teeth, but the entire jaw hurts. At the same time, the face becomes swollen, and any facial movements, be it talking or eating, cause severe pain. But this is not the worst type of inflammation.
Much more problems can arise when inflammation of the gums during a cold occurs simultaneously with blockage of the maxillary sinuses, that is, sinusitis.
In this case, the teeth not only hurt, but also begin to fester. Purulent sacs appear on the gums, which put a lot of pressure on the roots of the teeth and cause discomfort.
In this case, without dental care, the disease cannot be cured.
The main advantages of dental prosthetics
The main thing is to remember that toothache cannot be tolerated. But people who have experienced this condition say that their teeth can really get cold. These are the nerve endings in the teeth that signal that an infection has entered the body. It actively destroys tooth enamel. If such troubles occur, rinse your mouth as often as possible, but it is not recommended to use a toothbrush when rinsing.
Prepare a bath with warm water (36-38 degrees) and add to it a relaxing composition based on essential oils and any base (milk, honey, oil, sea salt). Dosage: 5-7 drops of essential oil per 1 tbsp. chosen basis.
Anti-stress essential oils for toothache and colds:
A hot decoction of sage also fights toothache. It should be kept warm in the mouth in the place where the painful tooth is located.
Source: https://ormira.ru/pri-angine-mogut-bolet-zuby/
Galvanic syndrome
Can a tooth cause a sore throat? Of course, especially if there are metal dentures in the mouth. This problem can arise if two or more types of metals are present in the oral cavity, although most metal teeth have many more types of metal, because they are made from alloys with the addition of titanium, zinc, silver and copper, cobalt. Upon contact with saliva, a weak electrical current may occur, leading to pain. If this happens constantly, then the inflammatory process begins, the teeth begin to ache, then the gums and throat. Other discomforts may also be present, such as headache, insomnia, and a metallic taste in the mouth.
Can a tooth cause a sore throat and how to treat galvanic syndrome? Only by replacing metal structures with ceramic or polymer ones. Although even after replacing teeth, nearby tissues will have to be treated. The dentist may recommend a course of vitamin therapy and immunomodulators.
Treatment
Pain after dental treatment appears for the following reasons:
- When treating caries, the nerve endings of the dentinal layer are irritated when a deep, prepared carious cavity is dried and treated with an adhesive solution.
- When treating pulpitis, depulpation is performed - removal of the dental nerve; pain after medical intervention can occur due to trauma to the periapical tissues with instruments or irritation with antiseptic solutions.
- Resumption of the carious process under a filling. Secondary caries develops if the filling was placed in violation of the rules for its selection and installation technology, or if the service life of the filling is exceeded (it depends on the type of filling material).
- Barodentalgia - acute toothache occurs when diving to great depths or flying. The reason is that under a poorly fitting filling there is an air bubble, which, when atmospheric pressure changes, increases in volume and puts pressure on the surrounding tissue.
Aphthous stomatitis
Can a tooth cause a sore throat? Maybe even if aphthous stomatitis is diagnosed. The disease is characterized by the appearance of ulcers and erosions in the mouth, cheeks, lip membranes and gums. These wounds are quite painful, accompanied by a burning sensation and can spread to the throat area.
The recurrent form is characteristic of childhood and adolescence.
Constant stress, smoking, and food allergies can lead to the development of stomatitis. Poor quality dentures can also cause the disease. Some detergents and toothpastes contain sodium lauryl sulfate, which can cause aphthous stomatitis. Another reason is a drop in the level of progestogens in the female body, that is, a change in hormonal levels.
In some cases, the appearance of stomatitis may be associated with Behcet's syndrome, problems with the gastrointestinal tract, and immune disorders.
It is quite difficult to cure stomatitis on your own; it is best to consult a doctor. During the treatment process, you will have to give up sour, spicy foods, and carbonated drinks, so as not to further irritate the mucous membrane of the mouth and throat.
How to relieve toothache
If the cold is in full swing and at the same time your tooth hurts badly, you can try to delay going to the dentist for a few days. To relieve toothache, you should follow these recommendations:
- Non-steroidal anti-inflammatory drugs will help with pain and fever. This includes Paracetamol and Ibuprofen.
- Lollipops containing menthol oil will help relieve pain. They cool well and relieve pain.
- Frequent rinsing with a solution of baking soda and salt will help eliminate pain. To do this, dissolve half a teaspoon of dry substances in a glass of well-warm water and gargle several times a day.
- You can rinse your mouth with decoctions of chamomile, sage and St. John's wort. Such medications are good at eliminating inflammation and reducing pain.
- Traditional medicine recommends rinsing the mouth with a solution prepared based on alcohol tincture of propolis. This medicine disinfects well and relieves inflammation.
- During a cold, you need to eat fruits, as well as dishes with garlic and onions . These products contain many vitamins and minerals that help strengthen the immune system.
Sometimes toothache subsides as soon as the cold is cured. But this is not at all a reason to postpone visiting the dentist after an illness. Only a doctor can say what could provoke acute toothache during a cold.
During a respiratory illness, do not forget to brush your teeth. After each meal, you should rinse your mouth with clean water or a decoction of medicinal herbs.
It is not worthwhile to routinely treat diseased teeth during a cold, as a number of complications may arise. But if the pain is very severe and is accompanied by gumboil, then you need to go to the hospital immediately. The dentist will definitely select the optimal treatment method, which will minimize the risk of complications.
Most of those who are susceptible to colds prefer to be treated at home. This also applies to the inflammatory process of the larynx - laryngitis. The lack of timely adequate therapy can lead to the development of severe complications, especially from the child’s body. How to treat laryngitis at home effectively and quickly? Let's look further.
Can a tooth hurt your throat and ear?
Yes, such situations are possible. Some people report that their ear, throat and teeth hurt at the same time. It is quite difficult to determine the cause on your own. Possible reasons include:
- Inflammation in the middle ear or mouth.
- Inflammatory process of the trigeminal nerve. On the side where the inflammation began, redness may be observed on the outside of the face. In this case, only a neurologist will help.
Main causes of pain
Most often, the problem lies in the presence of an infection that has appeared in the patient’s oral cavity due to the rapid spread of harmful bacteria. It usually develops around one of the most painful teeth. It can be distinguished from others if you pay attention to the excess gum tissue that covers it. Bacteria and food debris accumulate in the resulting space every time after eating. An abscess gradually develops, causing both tooth and throat pain. This happens when pericoronitis is left without proper and timely treatment, and the infection spreads to the rest of the soft tissues of the oral cavity.
We can say that this is mostly a disease of young people under the age of 20 with poorly developed wisdom teeth. Risk factors include those patients who have excess gum tissue in areas of their growth, as well as difficult access for proper regular hygiene.
Is it possible to remove a tooth during ARVI?
As is known from medical practice, in most cases, ARVI is accompanied by high fever, cough and many other symptoms. But there are a number of factors when it is permissible to undergo dental procedures even in this case.
These are cases of urgent need:
- progress of inflammatory processes in the tooth structure;
- there is a high probability that flux will appear at the next stage of the disease.
In such cases, the dentist will always undertake treatment, despite the acute phase of ARVI.
Everyone knows what unbearable toothache is. In medical practice, there are many examples when specialists urgently begin treatment, despite the progressing cold infection in the body.
Such cases include:
- instant development of inflammation in the tooth structure;
- inflammation is accompanied by suppuration;
- rapid development of flux.
In such situations, visiting a dentist is vital. It should not be put off even if there is no strength to get out of bed.
If you have a cold, your teeth may become sensitive. It may be accompanied by pain during eating, when eating salty, sour or sweet foods.
To relieve pain, medications with an analgesic effect are prescribed. In case of severe pain, the patient is referred to physiotherapeutic procedures after the recommendations of the dentist.
In addition, in such cases, you can use your grandmother’s methods at home. Many of them are characterized by high efficiency.
Pain caused by hypersensitivity can be relieved if:
- rub sore gums with garlic;
- rinse your teeth with a decoction of yarrow;
- rinse the mouth with a decoction of sage and thyme leaves;
- Place a small slice of lard between the sore spot and your cheek.
Many people, having fallen ill with ARVI, forget to follow the basic rules of oral care. They do not rinse their mouth after taking medications or food, and also, citing weakness, do not brush their teeth at night.
Such inactivity leads to toothache. To avoid this, you need to remember basic hygiene rules even during an acute period of illness.
During a cold, you can resort to the following pain relievers:
- Tooth drops - lightly moisten cotton wool in the product and apply to the sore spot.
- To relieve pain, the doctor prescribes anesthetics.
- Rinse with a soda solution (1 tsp per 1 glass of warm water). This will help relieve inflammation and reduce irritation of the periodontal tissue. The procedure should be repeated up to two times within an hour.
- Hot sage decoction – 1 tbsp. l. dry crushed leaves per 1 cup of boiling water. You should insist for at least half an hour. After taking the infusion into your mouth, you should hold it for some time in the part where the pain is located, this will increase its effectiveness. The prepared infusion can also be used to create an anesthetic compress. To do this, wet a small piece of cotton wool and apply it to the sore tooth for a few minutes.
- Thyme decoction: 1 tbsp. l. dry herbs in 1 cup of boiling water, leave for 15 minutes, can be used in a similar way to sage decoction.
- Yarrow decoction – 3 tbsp. l. pour 1 liter of water. Cook for 10 minutes, cool, strain. Use for rinsing.
- Plantain root applied to the tooth will shorten the time of pain.
- Reduce the amount of time acidic drinks stay in your mouth (for example, tea with lemon) - drink quickly.
- You should also temporarily avoid eating excessively cold or hot food.
Before using any medications, be sure to consult a specialist.
It is necessary to urgently go to the dentist, despite pain in the larynx and other unpleasant symptoms, in the following cases:
- flux formation;
- development of purulent and inflammatory processes against the background of an infectious disease;
- strong, pronounced pain syndrome;
- increased swelling.
In situations where toothache is acute and unbearable, dental care will be provided to the patient in any case; you should not endure it, it can be extremely dangerous.
In addition, sore throat sometimes occurs as a symptom of dental disease. Stomatitis, periodontitis, improper teething (in children or wisdom teeth in adults), and galvanic syndrome can provoke painful sensations localized in the larynx area.
Therefore, if you have problems with your teeth, a sore throat suddenly appears, but there are no other signs of a sore throat, cold or viral disease (sneezing, rhinitis, fever, muscle pain, cough syndrome), then you should see a dentist as soon as possible .
We suggest you read: There is no temperature on the throat of white formations
When it is very difficult to obtain a ticket for tooth extraction and you still have to wait several days until your turn comes, the toothache reaches terrible proportions. And suddenly, oh, sadness... A cold comes along. The patient doubts whether it is possible to remove a tooth if he has a cold, and begins to worry even more, exacerbating his general condition.
A confident doctor will say: “You must remove it, drink a capsule of antibiotics, and the cold will get better, and the wound after tooth extraction will heal quickly and without problems.” There are different situations with tooth extraction during a cold, and the dentist considers the specific situation each time.
Indications for tooth extraction
First of all, the question is whether it is possible to postpone tooth extraction until the cold is cured. The general condition of the patient is considered, whether the cold is so severe as to postpone depulpation of a complex, long-painful tooth. It is clear that a tooth intended for removal by a doctor is a breeding ground for infection and microbes in the oral cavity.
https://www.youtube.com/watch?v=CLWt8DNt3v0
No amount of brushing and rinsing will help overcome hordes of germs. Here the doctor considers the question of whether these same microbes are causing the inflammatory process throughout the body, and whether it is because of them that the ear shoots and the head hurts unbearably on the very side where the harmful tooth is lodged and waiting its turn.
Here the issue is resolved together with the therapist: it is necessary to remove the tooth and include antiviral drug therapy, taking painkillers in order to relieve the general symptoms of a cold, and to prevent infection from getting into the wound after tooth extraction. At the same time, the intake of immunostimulants and vitamin complexes is added to help the immune system overcome the painful condition and accelerate the improvement of the general condition.
The therapist and dentist jointly resolve the issue
Problems that the therapist and dentist solve together:
- strengthening the patient's immunity
- antiviral therapy
- antibacterial treatment of the wound after tooth extraction
- disinfection of possible wounds and cracks in the oral mucosa
- protecting the dentist himself from contracting a virus or infection
Dental tissue deteriorates quickly, and if there is a question about further installation of an implant, then the wound after tooth extraction must be kept clean and healthy so that the mucous membrane is not damaged by microbes. Therefore, it is imperative to remove the tooth, taking precautions against infection of the wound, despite minor manifestations of a cold. After all, while waiting for treatment for a cold, caries damage can spread to neighboring teeth, which is very undesirable for the general condition of the teeth.
Urgent cases of tooth extraction, despite a cold in the body, include all types of fluxes, when the danger of their development prevails over the danger of an inflammatory condition.
The dentist may refuse to remove a tooth if there are herpes sores on the lips, around the line of the mouth, and along the lower edge of the nose. The infection that causes herpes is stronger than cold viruses, and dentists are rightfully wary of it.
During a cold, the body fights germs and infections, which significantly weakens the strength of its immunity. Therefore, the risk of infection of open wounds that appear after dental surgery increases. Here the doctor makes a fundamental decision about what is more important for health – tooth extraction or eliminating problems with colds.
An important argument for postponing tooth extraction due to a cold is the use of anesthetics and painkillers during pulp removal, which can have a bad effect on a person weakened by a cold.
Cold without fever
Yes, most dentists recommend postponing tooth extraction due to a cold. At the same time, ARVI cannot be an absolute contraindication for depulpation. It still allows you to remove a tooth in case of emergency, which dentists attribute to a high risk of gumboil development and progression of purulent inflammation. Yes, there remains a high risk of infection of the wound after manipulations to remove pathogenic bacteria and cold germs.
But. Every patient should know: in such a situation there is a way out. Specialized dental centers using modern technologies, the latest equipment, and the latest drugs are ready to help patients in such situations. They use high-quality antiseptics, disinfect the oral cavity and herpes wounds on the lips, thereby achieving the complete destruction of germs and bacteria.
The use of innovative techniques when extracting a tooth in patients with colds guarantees the complete exclusion of infection of the wound after depulpation and the dental tissues adjacent to the extracted tooth.
Doctors with high professional training work with high quality, take responsibility for the patient’s health and their own health status, so patients can be sure that the procedure of tooth extraction along with anti-cold treatment will be carried out promptly and with minimal inconvenience for patients.
Oct 7, 2016Violetta Lekar
What to do?
For sore throat and other viral diseases accompanied by toothache, if the patient decides to postpone a visit to the dentist, some measures should be taken to alleviate his condition:
- Non-steroidal anti-inflammatory drugs and painkillers have a good effect, but taking any medications should be discussed with your doctor.
- Rinsing with a warm soda solution will help relieve toothache and relieve inflammation. Traditional medicine includes onion and garlic compresses and geranium leaves.
- A cotton swab pre-treated in propolis, dental drops, antiseptic or anesthetic solution can be applied to the lesion.
If after a few days the toothache becomes more and more severe and acute, you need to go to the dentist, not paying attention to the pain in the throat.
Moreover, sore throat, colds, and acute respiratory viral infections are not direct contraindications for dental procedures.
Is it possible to remove a tooth if your throat hurts?
Why is dental treatment not recommended for sore throat?
Dentists identify the following reasons why it is recommended to postpone dental treatment if you have a sore throat:
- The infectious process occurring in the body significantly increases the risks of complications such as stomatitis and gumboil.
- Nasal congestion, cough syndrome, pain in the larynx complicate the process of nasal breathing, as a result of which it becomes difficult for the dentist to carry out all the necessary medical procedures.
- Taking medications for the treatment of sore throat or infectious and colds does not combine well with anesthetics used in the dental field, which can cause side effects and unwanted reactions.
- The immune system is weakened, and accordingly, the infection can spread deep into the body through dental wounds.
- There are risks of pathogenic pathogens from the oral cavity entering the bloodstream.
We invite you to read: Darkened tooth - why and what to do?
In addition, the human factor must be taken into account. If a patient has a sore throat, it is possible that the disease is transmitted by airborne droplets, which means that the dentist and other patients can be infected.
Is it possible to treat your teeth when you are sick?
During illness, especially if there is a rise in temperature, you want to stay under the covers and drink tea with lemon. But what to do if at this time you have a scheduled dental treatment or, even worse, have a toothache? Is it possible to treat teeth if you have a cold? This article will provide comprehensive recommendations on these and other popular questions on the topic.
Is it safe to treat your teeth when you are sick?
Most dentists are inclined to think that a visit to a doctor should be made in a healthy state, that is, without any ailments. Some doctors even advise postponing a visit to the dentist during an exacerbation of chronic diseases such as gastritis, colitis, dermatitis, etc.
The fact is that during an illness, a person’s immunity is subject to a heavy load: he has to not only cope with the infectious agent, but also take care of restoring the normal functioning of the body.
At the same time, some methods of dental treatment, for example, anesthesia, depulpation, tooth extraction (extraction), etc., also put a strain on the body’s defenses. There is no need to overstrain your immune system.
Do cold symptoms – runny nose, cough, fever – affect treatment?
Manifestations of a cold or viral disease in the form of a stuffy nose, cough, sore throat, low-grade fever in themselves cause discomfort.
But in the dentist's chair it will increase several times, because you will have to sit motionless, with your head thrown back, for a long time. And at the same time breathing through your nose, which will be difficult with a runny nose.
In addition, it will be difficult for the doctor to carry out manipulations if the patient has a severe cough.
“Girls, never treat your teeth when you have a runny nose! Even if you put drops in your nose before taking it. Breathing through your nose is not the main problem. The main thing will begin later in the form of gumboil. Didn’t want to postpone your treatment date by a week because of a runny nose? Get two weeks of gumboil, a course of antibiotics, drainage of pus from the gums and all 33 pleasures. It almost didn’t come to the point of surgery.”
Post by user NataPustova from the ladycity.ru forum
Even if there is no runny nose or cough, but the temperature is elevated, dentists do not recommend dental treatment on such a day.
The fact is that an increase in temperature is the body’s protective response to the presence of any virus or bacteria, so an extra load on the immune system in the form of stress and drugs used by the doctor in dental treatment is undesirable.
In addition, tissue regeneration during such a period is reduced, which means that after visiting the dentist there may be complications: long-term persistence of the pain effect, poor blood clotting, incorrect reaction to anesthesia.
Important! If the increase in temperature is not caused by ARVI, but by an inflammatory process in the oral cavity (for example, inflammation of the gums, gumboil, cyst formation, etc.), then treatment should be carried out immediately. This condition can lead to more serious complications, so doctors advise not to delay your visit to the clinic.
Is it possible to remove a tooth during ARVI?
Surgeons, as a rule, do not advise a patient to remove teeth if he has symptoms of ARVI. The risk of infection of an open wound during such manipulation is very high. Even the immune system of a healthy person sometimes fails to protect itself, and complications arise. And if the immune system is loaded with the fight against the virus, then this is an almost one hundred percent guarantee of the development of complications after surgery.
Attention! Tooth extraction during a respiratory viral disease is possible only for health reasons. In this case, the surgeon must thoroughly disinfect the entire oral mucosa and surface of the teeth, as well as the patient’s lips.
After removal, he treats the wound itself with antiseptic drugs, and the patient is prescribed a course of antibiotics and drugs that strengthen the immune system. It is recommended to adhere to the schedule for taking such medications throughout the entire course of treatment.
Is it possible to treat teeth if a “cold” appears on the lip?
The appearance of herpes on the lip (or, as it is called in everyday life, a “cold”) itself is rarely accompanied by malaise, fever or other symptoms.
However, if a painful blister appears on the lip, this means that the body’s immunity is weakened and it does not have enough strength to contain the virus.
In such cases, patients are advised to first cure herpes and take care of supporting the immune system.
In addition, the herpes virus is also dangerous because it can get from the lip through instruments to open areas: wounds on the gums or nerve canals of the tooth. This will lead to complications of treatment - stomatitis, suppuration in soft tissues, etc.
In what cases is it acceptable to treat teeth during a cold?
Dental treatment for ARVI is not recommended, but there are cases when you cannot postpone a visit to the doctor. The most striking example is the risk of periostitis (flux).
Periostitis is a purulent inflammation of the periosteum, which can provoke the development of more serious diseases. Infection of the periosteum can develop against the background of hypothermia and ARVI, acute periodontitis or pulpitis. In this case, treatment must begin immediately, before the formation of a purulent sac, otherwise intoxication of the body cannot be avoided.
Worth remembering! Sometimes painful sensations in a damaged or previously filled tooth can occur against the background of a cold and fever. As a rule, pain and discomfort go away after 3-4 days, as soon as the cold symptoms disappear.
Complications after dental treatment during a cold
Viruses most often enter the body through the mucous membrane of the throat or nose, so these tissues are the first to become inflamed. The proximity of the infected area to the treatment site increases the risk of the virus entering the tooth tissue, for example, along with saliva. This can not only slow down recovery after manipulation, but also cause complications:
- sinusitis: if a virus or bacteria enters the maxillary sinuses. This disease is very dangerous because a large amount of pus forms in the sinuses close to the eyes and brain, which leads to intoxication,
- Otitis media: If an infection enters the inner or middle ear and causes inflammation. Severe otitis media can lead to hearing loss,
- pneumonia: if the infection enters the respiratory tract, inflammation will begin in the lungs. Treatment of pneumonia is very long, and if it is started untimely, the risk of death increases,
- meningitis: viruses or bacteria enter the brain through the circulatory system, causing inflammation of its membranes. This disease is characterized by high mortality,
- osteomyelitis: when the infection spreads through the bloodstream or infected surrounding tissue to the bone tissue. The course of the disease is such that it leads to bone deformation or degeneration.
How to get rid of toothache during ARVI
In general, the acute form of ARVI lasts 3-5 days, and it is better to spend this time in bed, following the doctor’s instructions. However, if the toothache worsens due to illness, you can try to relieve it with home remedies.
- rinsing with herbal decoctions: chamomile, sage, St. John's wort, eucalyptus,
- rinsing with antiseptic solutions: furatsilin, chlorhexidine, Miramistin, etc. Moreover, rinsing not only the throat, but also the entire oral cavity, will help reduce inflammation of the mucous membrane and speed up recovery,
- the use of drugs that increase immune resistance: vitamins (C, A, E, B, D), as well as macro- and microelements (magnesium, calcium, omega-3),
- taking painkillers and NSAIDs: here it is better to consult a doctor regarding the dosage and regimen.
In any case, you should refrain from dental treatment if you have a cold. After all, visiting a dentist during an acute respiratory viral infection is fraught not only with complications: the carrier of the virus spreads it to others, thereby provoking the development of an epidemic.
Source: https://mnogozubov.ru/mozhno-li-lechit-zuby-pri-prostude/