Features of retention
The prerequisites for eruption anomalies in most cases are laid during the period of intrauterine development of the fetus. As for the third molar, it begins to grow into the gum as it does not have enough space in the jaw. The problem may also be associated with supernumerary crowns, which begin to grow near normal ones, squeezing them and injuring the mucous membrane.
If a tooth has grown in the gum, this is considered not only a cosmetic defect, but also a pathology that requires elimination. The main treatment is removal.
Improper eruption can be caused by abnormalities of the jaw, lack of space for normal growth, horizontal eruption, traumatic injuries and surgery.
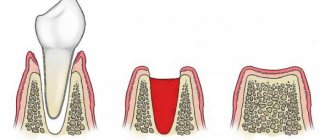
Retention can be of two types - complete and partial. In the first case, the tooth is not visible; it is completely covered by gum and cannot erupt. With partial retention, the apex of the crown is visible, which appears next to the normal one.
Signs of tooth growth into the gum
The first signs of a disorder can be observed during the teething period, but pathology can be detected earlier by taking an X-ray of the jaw. Parents may notice that crowns erupt in a chaotic manner, and some are completely absent. Another sign will be that another tooth appears very close to a healthy one, but does not erupt completely.
The presence of an anomaly in eruption is indicated by the following manifestations:
- reddened mucous membrane in the eruption area;
- incorrect position of the crown, its direction to the side;
- swelling of the tissues, a lump resembling a fistula may occur;
- general symptoms occur - weakness, fever;
- When chewing, the inflamed area is painful.
Good to know!
This problem most often arises with the growth of a wisdom tooth, which cannot fully erupt because it is covered with a “hood.” This causes pericoronitis, inflammation. The pathology appears again and again if an incision is not made in the gum or the causative tooth is not removed.
Wisdom tooth: inflammation of the hood and its symptoms
Patients who have inflamed gums near a wisdom tooth usually complain to the doctor that their wisdom tooth is growing, their gums are swollen, and there is also an odor from the wisdom tooth. The formation of an unpleasant odor is caused by the formation of pus, which is gradually released from under the hood. Patients also complain of pain in the area of the wisdom tooth. Such symptoms correspond to only a mild form of pericoronitis.
What do the symptoms of pericoronitis look like in the video? Please note that in the video below you can see the following symptoms: redness and swelling of the hood above the upper wisdom tooth, a small amount of purulent discharge (white) from under the hood. Such symptoms correspond to a mild form of inflammation.
If pericoronitis occurs, treatment is only possible with a dental surgeon. But at the initial stage, patients try to relieve the symptoms on their own using available means: antiseptic rinses, dental drops, painkillers. In most cases, this is ineffective and the inflammation only increases. The following symptoms increase (in various combinations):
increasing pain- severe swelling and redness of the gums,
- swelling of the cheek (Fig. 4),
- purulent discharge from under the hood,
- painful swallowing
- difficulty opening the mouth,
- increase in body temperature,
- weakness,
- swelling and tenderness of the submandibular lymph nodes.
Important: if at this stage the wisdom tooth hood has not yet been removed (see below), then you should be prepared for the next development of events. Firstly, because inflammation occurs in the area of the masticatory muscles - their spasm can lead to almost complete closure of the mouth. If at this moment you decide to go to the dentist, then he will not be able to do anything for you if your mouth is not opening enough, except to refer you to the hospital.
Secondly, pus may begin to spread not into the oral cavity, but rather deep into the bone and soft tissues, which will cause the formation of an abscess or phlegmon (peripharyngeal or submandibular). The latter complications will also mean inevitable treatment in a hospital, and therefore it is better not to bring the inflammation of the wisdom tooth to a critical level.
What complications can there be?
In children and adolescents, retention can be observed for several months. It is a mistake to believe that the milk bite will change and the problem will go away on its own. In fact, anomalies in the eruption of the first crowns affect the state of the permanent occlusion. The problem must be eliminated at any stage of the formation of the dentition.
If retention is ignored, it threatens the resorption of healthy roots. There is also constant trauma to the gums, which causes them to become thinner and may recede. An inflamed wound becomes an entry point for infection, which threatens the development of periostitis, that is, gumboil.
Further ignoring the problem leads to destruction of bone tissue, and osteomyelitis occurs. In this case, long-term treatment with surgery is already necessary.
As for the figure eight, if the tooth has grown inside the gum, it will become a factor in chronic inflammation. At the same time, there is constant pain and it becomes difficult to open your mouth. The problem leads to frequent biting of the gums, which causes severe discomfort. A person begins to chew predominantly on the healthy side, and this threatens bone atrophy.
How is an overgrown tooth removed?
Root extraction is a fairly common dental operation. It is performed under local anesthesia and, as a rule, does not cause complications. An overgrown root cannot be removed using traditional methods, since it is completely covered with gum tissue and there is no access to it. Treatment is carried out in several stages:
- Examination by a dentist, x-ray examination. X-ray allows the doctor to see the size, position, and depth of the root. The dentist assesses the risk of damage to adjacent teeth during surgery.
- The operation is performed under anesthesia. First, the doctor makes an incision in the gum, providing himself with access to the root. After this, the root is removed and sutures are applied.
- During the rehabilitation period, the doctor selects anti-inflammatory drugs and agents that accelerate wound healing.
The process of removing an overgrown root is individual in each case. The complexity of the operation is influenced by many factors:
- Tooth location. Removal of roots on the upper and lower jaws has its own characteristics and is carried out using various dental instruments.
- The degree of damage to the root and nearby tissues, the presence of fragments. Sometimes, for a successful and as painless removal for the patient as possible, the root is destroyed by a drill into several parts. Separation is required in cases where the tooth has several strong, deep roots. As a rule, after destruction, individual parts are easily removed using ordinary tools.
- The presence of pathology in the surrounding bone tissue, inflammation of the gums.
If you have a problem similar to that described in this article, be sure to contact our specialists. Don't diagnose yourself!
Why you should call us now:
- We will answer all your questions in 3 minutes
- Free consultation
- The average work experience of doctors is 12 years
- Convenient location of clinics
Single contact phone number: +7
Make an appointment
If there is no inflammation, the gum is carefully separated from the alveolus and the tooth is removed using suitable dental forceps. The inflammatory process “melts” the surrounding tissue, so for successful removal it is enough to provide access to the root by making an incision in the gum. Application of forceps does not require labor, and there is no need to additionally separate the gingival tissue from the alveoli. In difficult cases, elevators are used.
The tooth grew in the gum photo
Treatment options
Supernumerary teeth must be removed, but with the rest, things are different. According to the organ conservation principle, if something can be cured, extraction is not performed.
Attention!
The indication for removal will be a condition that requires long-term treatment without a guarantee of complete recovery. If the sharp edges of the crown constantly injure the gums, surgery is needed. This also applies to advanced caries and the presence of a cyst.
After removing a diseased tooth, anti-inflammatory therapy should be carried out. The dentist prescribes tablets, dental gels, and rinses. After complete recovery, the option of implantation or prosthetics to replace the defect is considered.
In the case of an impacted figure eight, treatment can be carried out without removal by cutting the mucosa. The essence of the operation is to remove the cavity between the gum and the tooth over which it hangs. This is necessary because pathogenic microflora and food particles accumulate in this gap, which provoke constant inflammation.
After treatment, the doctor prescribes painkillers (Nimesil, Ketanov, Ibuprofen). The gum removal and incision procedure itself is performed under local anesthesia.
All treatment options when the crown erupts in the wrong place:
- Resection of the mucosa, restoration of the shape and position of the coronal part using dental materials.
- Extraction to prevent relapse and complications (performed more often when the third molar is impacted).
- Removal along with the tissues that surround the causative crown with subsequent extension.
Other pathological causes
Situations when a hole in a tooth is overgrown with gum and it extends beyond its limits can occur with the following dental diseases:
- Deep caries. The development of this pathology occurs as a consequence of the proliferation of pathogenic microflora. This leads to the development of edema with severe hyperemia. Soft tissues increasing in size create a visual effect that gums begin to grow from the cavity of the tooth. This pathological process is accompanied by a painful syndrome and an increased reaction of the jaw row to temperature and taste stimuli. Teeth react to hot and cold foods, and there is also a burning sensation from spicy, sour, or salty foods.
- Inflammatory processes localized to the gum papillae. The main cause of this pathological process is chipping or destruction of incisors or molars on one side. Permanent injury to the area of soft tissue between the teeth is accompanied by abnormal growth of the gingival surface. In addition to visual changes, at the initial stage of the disease the patient experiences a feeling of discomfort due to constant pain. The chronic course of the disease is asymptomatic. During an exacerbation, when the overgrown tissue increases significantly in volume, the painful feeling of discomfort returns again, and the person begins to experience inconvenience while chewing food. Therapy is carried out only in a dental clinic using the coagulation technique (cauterization). However, it is better to seek help at the earliest stages when the “meat” begins to grow. If a growth has grown in the tooth hole, this may indicate bifurcation - destruction of the base of the roots of the chewing organ; in such cases, extraction (removal) is indicated. Therefore, you cannot delay contacting a specialist!
- Epulis. A type of benign formation. Various factors can play in the pathogenesis of the pathological process. Most often, this condition is provoked by a hormonal imbalance in the body or periodontal trauma. Sometimes the impetus for the development of this pathology is an abnormal bite, poorly placed dentures or braces.
The absence of painful sensations leads to the fact that a person does not consider it necessary to see a dentist. This occurs when heterogeneous tissue has grown and extended beyond the dental crown.
Surgical therapy is the only method to get rid of this pathological manifestation. The operation is performed under general anesthesia, since it involves dissection of the entire thickness of the soft tissue, and in severe cases, part of the affected bone is removed.
Prevention measures
The problem can be prevented even at the stage of teething of the primary occlusion. To do this, you need to take your child to the dentist and get an x-ray. The doctor will be able to see the position of the rudiments in the image. If an anomaly is observed, appropriate action will be taken.
When the problem occurs in an adult, the procedure is no different. It is necessary to take an x-ray, determine the position of the third molar and draw up a treatment plan. Some dentists immediately recommend extraction to prevent relapse in the future.
Eruption anomalies must be promptly identified and eliminated. This is easier to do in childhood. Parents are advised to visit the dentist with their child from the moment the first crown erupts, and not when a problem appears. This will allow timely detection of pathologies and effective treatment.