Poor dental condition brings aesthetic discomfort, disrupts digestion, and negatively affects human health. According to statistics, the third tooth is considered the most problematic tooth – the number eight or wisdom tooth. This is explained by its remote location and late onset of growth. Often wisdom teeth begin to crumble: what is the reason for this, what to do in such a situation?
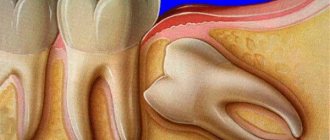
Wisdom tooth in the picture
General information about wisdom teeth
Its other names are third molar, figure eight. The peculiarity is that they erupt much later than other teeth in the row. Due to its late growth, the tooth got its name, since it is believed that at the age of 20 or more a person is already quite smart and wise. In total, 4 wisdom teeth grow, 2 eights each on the upper and lower jaws, 1 each in the dentition (right and left).
In 80% of the population, wisdom teeth do not erupt throughout their lives. This is not a pathology or a problem, since eights have long been considered a vestigial (obsolete) element. The third molar does not take part in crushing hard pieces and chewing food.
The structure of eights is no different from the structure of other teeth. Their features are different.
- Growth usually begins no earlier than 16 years of age.
- Problems may already appear at the teething stage. The tooth needs to “break through” the gum and make room for itself in the jaw.
- Difficulty in treatment and removal due to distant location and curved roots.
How long does it take for gums to grow onto a tooth?
The speed at which the gum grows on the crown of the tooth depends on the reason that caused its growth. A slow change is characteristic of fibromatosis, hyperplasia, and the eruption of a wisdom tooth. More rapid influx of gum onto the tooth occurs with fibrous gingivitis. Quick signs of swelling occur when baby teeth are replaced and carious cavities appear between the teeth.
Stages of development of hyperplasia:
- the appearance of a painless compaction at the base of the front teeth at a height not exceeding a third of the crown;
- the edge of the gum is deformed and rises up to half of the teeth;
- the overgrown tissue reaches the chewing or cutting edges of the teeth, the surface of the gums becomes covered with bleeding seals.
The gums retain the fragments of teeth for several years.
What to do if the gum has grown on the tooth:
- Methods for treating gum influx on a tooth in most cases are surgical intervention: removal of overgrown mucous tissue.
- Growing teeth, if they do not have enough space on the jaw, put pressure on the gums, which causes them to swell. Gum hypertrophy, formed during the change of baby teeth, is dangerous due to disruption of the nutrition of bone tissue, as a result of which the child will be left without teeth. All baby teeth and part of the overgrown gums must be removed.
Read also: What gums look like after tooth extraction
The consequences of untreated hyperplasia can be:
- osteoporosis;
- disruption of the replacement of baby teeth;
- destruction of interdental septa.
Diagnosis of hyperplasia consists of radiographic and histological examination of the gums. If the diagnosis is confirmed, the overgrown tissue is excised with a scalpel. At the same time, oral health is required:
- removal of tartar;
- filling;
- prosthetics;
- removal of debris.
The purulent form of pericoronitis can spread to adjacent tissues, and cause an abscess and breakthrough of pus into the buccal, sublingual, and palatal areas. Acute pericoronitis requires excision of the mucous membrane.
For the treatment of fibrous gingivitis, the following are used:
- cryotherapy;
- diathermocoagulation;
- gingivectomy.
Methods of cryodestruction and diathermocoagulation mean exposure of mucous tissue to low temperature or ultrahigh frequency current. The goal in both cases is the natural removal of part of the overgrown gum. After a few days, the damaged gum dies, a granulation layer forms, and heals without scars.
Gingivectomy is a surgical operation to remove a piece of gum using a scalpel or laser under local anesthesia.
Why can wisdom teeth crumble?
This is a common problem that can affect wisdom teeth before they are fully grown. The process of crumbling enamel is a signal that there is a complex malfunction in the functioning of the whole organism, and not just the oral cavity. To accurately determine the cause, an examination by several specialists (dentist, gastroenterologist) is required.
Metabolic disorders
In normal condition, saliva cleanses the oral cavity and saturates the enamel with calcium. With intestinal inflammation and fermentopathy, the acid-base composition of saliva changes: the liquid becomes acidic and destroys the tooth.
Poor oral hygiene
The third molar is difficult to reach with a brush; carious lesions may begin to form in it. The tooth is slowly crumbling.
Mechanical injury
Crunching nuts, untying knots on bags, opening bottles with teeth - small cracks appear in the enamel, the tooth is weakened and gradually destroyed.
Malocclusion, habit of grinding teeth and clenching jaws tightly
Premature wear occurs and fragility increases.
Grinding your teeth leads to tooth decay
Avitaminosis
Enamel is especially acutely affected by a lack of vitamin D. Calcium is not absorbed, teeth crumble.
Impact of chronic diseases
Possible ailments include diabetes, osteoporosis, and arthritis.
Possible complications
After the removal procedure, complications may arise due to the fact that harmful microbes and infection enter the unhealed wound.
They cause inflammation:
- Alveolitis. If a blood clot does not form at the healing site, the socket remains defenseless against bacteria. Because of them, an inflammatory process develops. The main symptom is pain after removing the remains, which occurs after a few days. Other signs include: swelling of the gums, inflammation of the edges of the socket, fever, and general deterioration of the condition. Sometimes symptoms manifest themselves in pain when swallowing, enlarged lymph nodes.
- Socket bleeding. One of the common consequences. It does not necessarily occur immediately after the extraction procedure, but also after a couple of hours, even days. The following factors can provoke: the use of adrenaline; non-compliance with specialist recommendations; injury to the hole; accompanying illnesses.
- Paresthesia. A rare but common complication in dental practice. The key symptom is numbness of the tongue and cheeks.
- Displacement of neighboring teeth.
- Injuries that occurred during the operation.
Side effects:
- Trauma to the oral cavity.
- Tooth fracture.
- Jaw fracture.
- Removal of a piece of alveolar ridge.
What to do when a wisdom tooth crumbles
There is a high risk that wisdom teeth will begin to crumble in women while carrying a child. During this period, hormonal levels change, demineralization occurs - lack of calcium, teeth become fragile. This condition is also typical during menopause and adolescence (if wisdom teeth have already begun to grow).
If you find that the figure eight has completely or partially crumbled, you should contact your dentist. If possible, take several pieces chipped from the enamel and show them to the doctor. Also, before going to the dentist, you are allowed to rinse your mouth with a saline solution - this will reduce pain and ease the inflammatory process.
What to do after surgery
The recovery period after removing an overgrown root, as a rule, is longer. This is due to the need to cut the gums. Medicines are selected by the doctor individually, depending on the initial condition and complexity of the operation. Typically prescribed:
- Anti-inflammatory drugs. The doctor may prescribe oral anti-inflammatory drugs and rinses.
- Painkillers. After any dental surgery, the patient feels pain. There is no need to take painkillers constantly. If discomfort occurs, you can take any analgesic.
- Healing agents. After surgery, it is important to ensure rapid healing of the wound channel. For better healing of the cut gum and tooth socket, the doctor may prescribe medications that accelerate tissue regeneration and promote rapid healing.
It is important to follow all the doctor’s recommendations, otherwise there is a risk of developing an inflammatory process. After final healing, the patient undergoes prosthetics.
Despite the fact that in the vast majority of cases the overgrown tooth is removed, there are exceptions. For example, if the crown was destroyed due to injury, the root is strong and healthy, a new crown can be built on it. In any case, the doctor makes the decision to remove or preserve the root based on the results of the examination.
When to delete
If the figure eight begins to erupt with damaged enamel and caries, most dentists recommend immediately removing such a tooth. Filling and treatment will be complicated due to the distant and inconvenient location of the third molar, and the procedure will not provide long-term results.
Wisdom tooth removal
If the wisdom tooth has fully grown, and then significant mechanical destruction of the enamel has occurred (a large part has broken off), removal is also indicated. The area where such a chip occurred will constantly injure the inside of the cheek, accumulate plaque and food debris - this will cause the development of caries.
When is removal still required?
- Complete destruction of the figure eight.
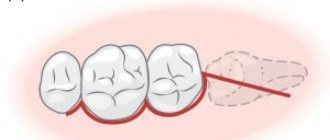
- The wisdom tooth is impacted - incorrectly positioned (there is no possibility of eruption).
- The enamel is deeply affected by caries; due to lack of access, the tooth cannot be treated.
- Unpleasant symptoms appeared - inflammation of the gums, headache, discomfort when swallowing.
What are the dangers of rotten teeth, consequences for the body
Many people ignore the process of tooth decay unless it is accompanied by severe pain. But the consequences of the carious process can be unpredictable and dangerous. If you have rotten teeth, the following complications may develop:
- Destruction of bone tissue of the musculoskeletal system.
- Endocarditis is inflammation of the lining of the heart.
- Inflammatory pathologies of the kidneys.
- Infections of ENT organs.
- Psychological complexes due to discomfort during communication and dissatisfaction with the appearance of the dentition.
- Purulent-inflammatory diseases in the gums (abscesses, phlegmons) and, as a result, the spread of infection throughout the body, leading to general intoxication.
The health of baby teeth greatly affects the condition of the permanent buds. Therefore, if nothing is done about the decay of milk dental tissues, in the future the child may have big problems with the formation of a permanent dentition.
How to relieve pain
A decayed wisdom tooth is a source of inflammation and the development of infectious processes. The problem cannot be solved with painkillers. Failure to seek help in a timely manner may result in the appearance of pulpitis or the onset of abscess growth. You can only take medications to relieve pain for a short time if you cannot get an urgent appointment.
Baking soda rinse
For pain relief at home, a solution of baking soda, salt and water (1:1:3) or herbal infusions is recommended. You can make a decoction of sage, calendula, strawberries, and chamomile. The following healing herbs will also reduce pain:
- mint, oregano and St. John's wort;
- sage, celandine, oak bark;
- chamomile, currant leaves, string.
Take only dried ingredients and brew with boiling water. After insisting, rinse. If the pain is severe, you can take Ibuprofen, Nimesulide, or treat the area with Metrogyl-Denta or Cholisal gel. Before using these products, it is better to consult your dentist by phone.
Treatment of the tooth socket
After removal, it is necessary to treat the wound. The doctor, as a rule, suggests that the patient rinse the mouth with a special substance. This is a 2% sodium bicarbonate solution. In other cases, the dentist places a gauze pad on the wound, considering rinsing unnecessary.
After the operation, the person must firmly press the gauze to the wound with his teeth. After a quarter of an hour, when the bleeding has completely passed, the tampon is removed. During the day, you should not apply mechanical pressure to the wound.
Eating is allowed approximately 4-5 hours after the procedure. To avoid causing bleeding again, the patient should not drink hot drinks. You should rinse your mouth with tincture of medicinal herbs. These are calendula, oak bark, chamomile.
Washing the wound is done after each meal for 3 days, when the wound is completely healed.
How to rinse the socket correctly so that the blood clot that has formed on the socket, which prevents infection from entering the blood, is not washed away? This happens if the patient performs the procedure too intensively.
This leads to bleeding, inflammation of the socket and other complications:
- On the first day, do not rinse your mouth, but use baths. The solution is drawn into the oral cavity, kept for up to 5 minutes, and spat out. You should not drink or eat for an hour after this.
- Ask your doctor exactly when to rinse and for how many days after surgery. If the procedure is prescribed by a specialist, perform it very carefully so as not to harm the clot.
What is the best way to rinse:
- chlorhexidine;
- miramistin;
- saline solution;
- a solution of salt and soda, in a ratio of 50/50;
- decoction of medicinal plants (sage, chamomile, calendula, eucalyptus);
- solution of potassium permanganate in low concentration;
In modern times, almost all procedures are performed under anesthesia. However, many patients who want to remove a tooth root are tormented by the question: does it hurt? How will I feel during the process?
Before the operation, local anesthesia is given by injection with an anesthetic drug. If there are remains above the root that you can grab with forceps, no one will cut the gum. Even if there is an incision, the patient will not feel any pain. It will be much more painful when the root becomes inflamed and an infection appears in the mouth, which subsequently spreads to the remaining teeth.
In general, removing a tooth root is no more painful than removing a whole tooth. In the first hours or even days after removal, there will be unpleasant sensations that bring discomfort, but painkillers solve this problem.
Be sure to pay close attention to choosing a specialist. An experienced doctor will perform the procedure painlessly and without dangerous consequences.
What to do if the tooth crumbles but the root remains
If all that remains from the figure eight is the root, which has no structural defects, the question of the sequence of further actions arises. If there is an infection, there is a threat of cyst or fistula growth - such a root must be removed. If an inflammatory process begins at the root, treatment in 3 stages is indicated.
- Removal of dead pulp, treatment of the root with an antiseptic.
- After 3 days, re-treat with an antiseptic and place medication in the root canals.
- If no signs of suppuration are found, the issue of tooth extension is decided.
Other actions
In case of minor damage to the enamel (if a small part has broken off), restoration and extension is indicated. When a carious lesion begins on a normally growing and functioning figure eight, it is not recommended to rush to remove it. It is enough to carry out timely and complete treatment. When filling, classic preparation of the carious lesion using a drill is used.
It is necessary to preserve wisdom teeth from which a small part has broken off, since they often act as a support when installing crowns. Also, a bridge prosthesis is attached to the figure eight in case of loss of the 6th and 7th teeth.
Tooth extraction – review
There will be no photo of the pulled out tooth and the location of the hole. My wisdom tooth (“eight” in the language of dentists) completely came out a little more than six months ago. It immediately began to deteriorate and even part of the tooth broke off. What should I do? I made an appointment with the dentist. He looked and reported to me and said it needed to be removed.
The filling cannot be treated. I made an appointment with a dentist-surgeon for removal. The doctor groaned that the tooth was complex and sent me for an X-ray. Tooth on the lower jaw. Especially for review. Here it is, my painful wisdom tooth: the first one on the left. The roots are not twisted, not retinal (that is, they grew straight, according to all the rules).
The whole difficulty was that there was nothing to hook the tooth onto. Those. there was almost no crown (I thought that I had half of it, but in reality there was just a little cap. There was a huge hole inside), and the roots all remained inside. Well, here they like to show “hamster cheeks” - I don’t have them as such WAS.Photo before.
——————–
The process of wisdom tooth removal.
She has arrived. I sat down in a chair (took a survey about allergies, etc.). The doctor filled the syringe with painkillers. Moreover, the syringe was a five. I was scared of the needle (before that I had done a filling in a sensitive place, also with an anesthetic, so the syringe and needle were tiny. But, of course, I tried not to show it (after all, I’m almost thirty). But, removing the tooth was still a little scary.
The doctor injected me with painkillers on both sides of the tooth. The first injection was sensitive, but not much, about an injection in the butt, i.e. almost painless) The second one was a little more noticeable. Well, they left me right in the chair for 15 minutes (for the freezing to take effect). At this time, the doctors were talking among themselves about dentures, and I looked out the window at the flying snowflakes and listened to them with half an ear.
And now, the “finest hour” has come. The doctor took some kind of tool that looked like a hook. I picked something there, it crunched (maybe it was opening my gums). The painkiller worked well; I felt no pain in this area.
(A sneaky thought crept into my mind that if the doctor’s hand fell off and the hook stuck in my tongue or under my tongue, it would be very painful). Then the dentist called the assistant and picked up the CHISEL. And she cheerfully told me that we would scare the next visitors.
The assistant held my jaw (precisely held from below, behind the chin), and the doctor, using a hammer and chisel, removed the roots of my figure eight... By the way, just now I read on the Internet that
In general, the use of a chisel is prohibited in modern dentistry. Doctors of the old school use a chisel. Such removal is considered traumatic. Amazing! That is, I tried the old methods on myself. I didn’t even know (and didn’t think about) how to remove teeth and roots. In general, she removed all the roots for me in 8 mini-strikes.
With the first blow, I felt a trickle of blood flow (in my mouth), then a small one flowed down my lip onto my cheek. The vibration from the blows was felt in my jaw. But I hoped that they wouldn’t roll it up for me (they’re holding it, hee hee). Then, the doctor put the chisel aside, took the tongs and pulled out the pieces. I didn’t even realize that it was all over. They put medicine in my wound, then a gauze pad.
In general, the whole procedure took: 15 minutes for freezing + 10 minutes for wisdom tooth removal. Photo almost immediately after removal: I came out: there were frightened people around the office, waiting for their turn. I can imagine: the sounds of the chisel are probably annoying and I have bloody lips... (although I didn’t squeak or even make a sound. Absolutely painless, I just heard crunching, vibration, etc. They numbed me well).
The recommendations that the dentist gave me after the tooth extraction: - after half an hour, remove the bandage and throw it away.
- don’t eat for two hours - don’t rinse, don’t warm (bath, hot shower is excluded) - don’t drink/eat hot things - for pain - Ketonal (I have this kind of medicine at home) - severe bleeding, fever, pain (without the pills work) and other things that worry me are a reason to immediately contact her (i.e., the dentist). Photo after: It seems to me that my cheek is not swollen at all.
Let's see what happens in the next days. I'm talking normally, but for now I haven't eaten for 3-4 hours (but soon I'll try to eat at least yogurt). The effect of the injection has almost worn off, it started to wear off on the way back from the clinic: “a feeling of tingling and goosebumps " And now, after 4 hours, the effect has almost worn off, now I feel a nagging pain in the tooth socket.
I’m wondering if I should drink Ketonal or is it too early? (Later, I’m afraid it will be too late)…I dreamed to myself that I wouldn’t be able to eat for 2-3 days and would eat yogurt-kefir. This was not the case: first I ate yogurt, then halva, then a full dinner (grilled sausages and pasta). Of course, I chewed on the opposite side of the jaw. At night, my jaw began to ache; it seems difficult to open my mouth when talking.. ———————
Day two after removal.
At work all day. But I still tried to talk less; my jaw ached during a long conversation. I drank chamomile tea. She brushed her teeth carefully. I still feel the taste of the medicine that was put into the hole that formed. ——————- Day three. The cheek is still swollen. Almost no one notices except me. The jaw doesn't ache. But I still don’t drink hot food and chew on the opposite side. ———-
A week later.
I had already forgotten about this unpleasant procedure. I still chew on the opposite side, but (forgotten) also on the side with the hole. I advise everyone to look on the Internet for photos showing the stages of healing. I looked and was worried whether the gums were healing properly after tooth extraction. I was especially worried about something white in the hole.
Well, naturally the Internet helped: White socket after tooth extraction Normally, by the 3rd day after tooth extraction, the socket is covered with a thin white film, which indicates the beginning of healing. By 4–5 days the entire socket becomes white, which is also normal.
Therefore, if the color of the hole is white and not some other shade, and there is no unpleasant odor coming from the oral cavity, then this only indicates the normal course of the healing process. ———————Main: The roots of the tooth were removed with a chisel and hammer. This is an old method.
The whole procedure took 25 minutes (15 minutes for the painkiller to take effect and 10 minutes for the tooth extraction itself). Cost: approximately 10 dollars (state clinic, Belarus). An X-ray of a tooth costs about $2 more.
If I have to extract a tooth again, I will look for a clinic that does not use a chisel.
Source: https://irecommend.ru/content/udalenie-zuba-mudrosti-ostalis-vnutri-korni-ne-za-chto-bylo-podtsepit-udalenie-kornei-zubov
Preventive measures
If wisdom teeth are crumbling due to vitamin deficiency or calcium deficiency, you need to take a course of vitamins. Often chips and cracks are a consequence of improper functioning of the digestive system - acidic saliva destroys the enamel. In this case, consultation with a gastroenterologist and taking prescribed medications is required.
What general rules will help protect wisdom teeth from destruction?
- Regular dental checkups.
- Be careful with your teeth (do not chew hard objects).
- Monitor the balance of drinking water - a sufficient amount of minerals, fluoride.
- High-quality oral hygiene.
So, if a wisdom tooth has crumbled, this is the result of the influence of a complex of factors. The list of possible causes includes disturbances in the acid-base balance of saliva, lack of microelements, mechanical damage, and heredity. If the figure eight has just begun to grow and has already crumbled, removal is indicated. If the chips are small and caused by injury, the tooth is restored and preserved.
Diagnostics
A person can notice putrefactive processes on his teeth during a visual examination of the oral cavity. As a result of destruction, dark and white spots become visible on the enamel. This condition indicates tooth decay in an advanced stage.
In the early stages, the problem is identified using special dyes or dental floss. Fluorescent examination allows you to see the darkening against the background of white enamel. Private dental clinics use the Diagnodent device to determine damage to tooth enamel.
The essence of the technique is irradiation of tooth enamel with light waves and further analysis of the reflected light. If an abnormal composition of bone tissue is observed, the device gives a signal. If putrefactive processes have spread to the root part of the tooth, then you can only find out about the problem with the help of an x-ray. The pictures show the affected areas of bone tissue.
Removal or treatment?
Removal of wisdom teeth occurs in several stages. After visiting the dentist, the patient is sent for an x-ray, and if there are no contraindications, an anesthesia option is selected.
To remove or preserve a diseased tooth is the main question for the attending physician after the patient’s treatment. What does this depend on? In fact, there are many reasons:
- the degree of neglect of the tooth decay process (tooth flux, huge holes, the last stage of decay, perhaps it has already crumbled badly);
- the presence or absence of an adjacent molar;
- exact position of the tooth (angle of inclination, degree of eruption, gum hardness);
- risk of developing crowded teeth;
- the need for prosthetics (using a specific tooth as a support for dentures).
Read also: What is tooth depulpation
In certain cases, it is more rational not to remove the wisdom tooth, but to try to cure it. But in such a situation, how can you get rid of the hellish pain caused by a wisdom tooth? You can temporarily weaken it with the help of antibiotics purchased at a regular pharmacy. But even in this case, consultation with your doctor regarding the use of certain medications is simply necessary.
There are several simple ways to relieve pain from a rotten tooth and get rid of the smell using improvised methods. The most effective of them is rinsing the mouth with a lukewarm, low-percentage salt solution. This simple action will relieve toothache and odor almost instantly and for a couple of hours.
Still, it is necessary to solve the problem with the worrying wisdom tooth once and for all. And no matter how sad it may sound, the most effective remedy for pain in molars is extraction. This process requires careful preparation and consultation with a dentist. A smoother and more painless procedure will depend on the good specialist you choose.
Indications for removal
Retention can manifest itself as a stage of eruption. Over time, the crown completely appears above the gum and the tooth can function normally. Therefore, the decision on the need for removal should be made by a doctor only after examining and diagnosing the condition of the dental system. Indications for surgery are the following clinical cases:
- Constant pain;
- Complications of eruption;
- Trauma to an adjacent molar;
- Pressure on the dentition and its deformation;
- Horizontal or angular position of the third molar in the jaw;
- Dental crowding, which can be aggravated by wisdom teeth;
- Orthodontic and orthopedic indications, that is, the need for extraction to correct the bite or prosthetics.