{jcomments on}Radicular cysts of the jaws most often occur with the development of a chronic inflammatory process around the root of the tooth, occurring in 95% of cases. Their occurrence in men and women is approximately the same, they are more often found between the ages of 20 and 45 years. Radicular cysts on the upper jaw are somewhat more common than on the lower jaw, in 56 and 44%, respectively. Most often, due to the anatomical and topographical features of the jaws, cysts grow towards the vestibule of the mouth.
Rice. Radicular cyst
Causes
The prognosis of the disease depends on the type, size and location of the cyst.
Most cysts are benign and some do not require treatment at all. Sometimes a cystic lesion can provoke a local aggressive tumor, which, if not treated correctly, can cause destruction of surrounding tissue. This type is usually removed surgically to prevent new cysts from forming. If the cyst reaches a large size, the lower jaw may be weakened so that a pathological crack appears. Source of information: Wikipedia.
The most common cause is infection of the root canal. About 450 species of bacteria live in the oral cavity of a healthy person, which enter there along with food and feed on its remains on the teeth. If the dentist does not follow safety rules when treating a tooth (namely, does not use antiseptic baths during endodontic treatment), small particles of the tooth may get inside the canal.
Also of great importance:
- Poor oral hygiene.
- Weak immunity.
- Mechanical damage to teeth and gums.
- Gum diseases.
- Damage to the tissue of the jaws themselves.
Features of the therapeutic approach
Therapeutic treatment is quite long and consists of the following stages:
- Treatment of root canals: removal of pulp (if they are not filled), unfilling (if they were filled).
- Antiseptic root canal cleaning.
- Injection of an antiseptic directly into the cavity of the dental cyst.
- Filling canals with paste with an antiseptic effect.
- Placing an antiseptic into the cyst cavity and antiseptic cleaning of the root canals are performed for several months at each visit to the dentist.
- If the x-ray shows a decrease in the diameter of the cyst, then the therapeutic approach is effective.
- Final filling of root canals.
- Installation of a seal.
After treatment, the patient needs to have an x-ray every few months to assess the condition of the cyst under the tooth. The dynamics should be as follows: reduction in the size of the cyst and restoration of bone tissue. Statistics show that therapeutic treatment gives a positive result in 70% of patients.
Symptoms and signs
When the tumor is small in size, it does not manifest itself in any way and can only be detected on an x-ray.
Symptoms appear along with an increase in the diameter of the tumor:
- Pain.
- Jaw deformation.
- Increase in jaw size.
- Headache.
- Symptoms of sinusitis (mucus secretion, nasal congestion, inflammation of the mucous membrane and stench).
- When pressing, you can hear the crunch of tearing parchment.
More unpleasant and dangerous signs are observed if a secondary infection is added to the main ailment:
- Sharp pain, especially when opening the mouth, chewing and talking.
- Inability to fully open the mouth.
- Teeth become loose and fall out.
- Fabrics peel off.
- Inflammation of the lymph nodes.
- Earache.
- Discharge of pus into the oral cavity.
- Temperature increase.
- Severe weakness.
If the disease leads to the development of osteomyelitis (death of bone and bone marrow cells), loose teeth and numbness of tissues are possible.
Types of jaw cysts
Jaw cysts are usually divided into two types: odontogenic and non-odontogenic (pseudocysts).
The first are formed from the remains of the emerging tooth. The second category includes all other types.
The formation of odontogenic cysts is promoted by:
- Chronic periodontitis.
- Caries.
- Incorrect treatment.
- Destruction of bone tissue.
- Inflammatory processes in the bone.
The neoplasm is localized at the apex of the tooth. On an x-ray, such a cyst looks like a darkened area around the crown of the tooth. They are always an intraosseous formation. The liquid contents are a derivative of the epithelial lining. Represented by crystalloids and colloids (solutions of crystalline and non-crystalline substances, respectively).
Non-odontogenic cysts most often develop during fetal development. They are associated with so-called embryonal facial dysplasia, i.e., a disorder of facial development during embryonic development. Nasopalatines originate from the remains of the nasopalatine canal.
Symptoms
The cyst is a single-chamber cavity filled with pasty, liquid and semi-liquid contents. Puncture reveals a yellow liquid mixed with cholesterol crystals. The cyst shell consists of dense connective tissue and stratified epithelium, similar to the epithelium of the oral mucosa.
In most cases, the follicular cyst is localized near the lower wisdom teeth (56% probability) and fangs. Less commonly, it fills the maxillary sinus or is located in the nose or below the orbit.
The development of a cyst is a fairly long process that goes through two stages:
- There are no visible symptoms.
- A painless or slightly painful swelling of the gums appears. Pressing on it is easy, the growth is pliable. If the cyst is large enough, a parchment crunching sound may be heard.
In the second stage, infection of the cyst usually occurs.
The fluid filling it becomes cloudy and contains many leukocytes. On average, cyst growth takes from several months to several years. In many cases, due to its painlessness, the process goes unnoticed, even if the bone tissue of the jaw is significantly affected. Usually the patient consults a doctor when the alveolar processes are already clearly growing. Among other things, many patients experience a thickening of the jaw and a corresponding deformation of the face in this place.
On an x-ray, a follicular cyst is very visible: it looks like a clearly defined rounded spot more than 3 mm in size. There is some difficulty in distinguishing between a normal follicular sac and a cyst: in the image they differ only in size (normally, clearing should not exceed 2.5-3 mm).
Classification
There is a classification by location and structure. Cysts of the upper and lower jaws are distinguished by location, and by structure - retromolar, follicular, radicular, aneurysmal, etc. Treatment methods and symptoms of all types are similar.
Retromolar
The second name for this neoplasm is primordial, or keratocyst. It is most often formed on the lower jaw. The name "retromolar" refers to its location behind the molars (marinar). The fluid found in it is called cholesteatoma. After removal of such a cyst, relapses are possible.
Radicular
The most common type, usually appears with periodontitis, is located at the root of the tooth, the walls are thin, fibrous, the lining has many layers, lined with flat non-keratinizing epithelium. It contains lymphocytes and other cells. When there is inflammation, cells often grow inside the wall.
Aneurysmal
This variety belongs to the non-epithelial type (does not have an epithelial lining). As a rule, it occurs on the lower jaw during puberty and in youth. For some time, science considered this species as a special case of osteoclastoma. It looks like a cavity filled with blood or hemorrhagic fluid. In rare cases, there may be no fluid inside at all. The bone cavity is lined exclusively by fibrous tissue, without epithelial cells, but may contain bone cells. The cyst gets its name because it leads to swelling (aneurysm) of the lower jaw.
Follicular
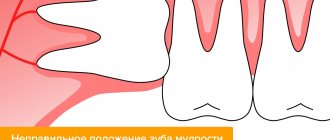
Follicular cysts develop from dental follicles. The reason is the vicious development of this formation or its mechanical injury. Development is influenced by inflammation of the tops of baby teeth. Usually found in children, rare after teeth change.
The neoplasm has an epithelial lining ; the contents can be either liquid or thick (up to a mushy state).
Nasoalveolar
This variety is localized in the vestibule of the nasal cavity and is lined with epithelium. Characteristic location in soft tissues. Protrusion of soft tissues under the influence of a cyst can lead to a narrowing of the nasal cavity.
Residual
Refers to root cysts. They develop on the upper jaw in 2 r. more often than on the bottom. The characteristic ability is growth towards the nasal cavity with the formation of a protrusion in it. Difficult to detect in the early stages, often leading to suppuration.
Traumatic
This variety is characterized by the absence of not only the epithelium, but also the main shell. They are cavities filled with liquid or completely empty.
The mechanism of their formation is not clear, however, it is known that they appear after a strong mechanical blow to the bone, which led to bone marrow injury. According to one version, the cause of the tumor is hemorrhage into the bone marrow. They are observed mainly in young men. Shown up on x-rays.
JAW BONE CYSTS IN X-RAY IMAGE
A cyst is a benign cavity formation, usually having a round shape, liquid or semi-liquid contents and delimited from the surrounding bone tissue by a connective tissue capsule. In the jaw bones, cystic lesions are much more common than in any other part of the skeleton. In the vast majority of cases (more than 90% of cases) they are of odontogenic nature and belong to true cysts that have an internal epithelial lining. A smaller group consists of brushes that are not associated in their development with the tissues of the tooth germ and are false, since they lack the inner bordering epithelial layer. Both types of cysts give the same type of shadow picture of clearing, clearly demarcated from normal bone tissue, with a cortical rim along the periphery.
The epithelial lining of cysts is most often formed from embryonic primordia or from epithelial cells formed as one of the manifestations of tissue differentiation defect. The growth of a cyst, as a rule, is not a manifestation of true proliferation, but reflects periods of rising osmotic pressure of the contents in its cavity with a slow increase in volume, in response to which the surrounding bone is resorbed, and the border areas of the bone tissue are compacted, forming a compact rim.
With the introduction of orthopantomography into widespread practice, the frequency of detection of cysts has increased significantly, including at the preclinical stage of the disease. This technique makes it possible better than others to determine the relationship between the cyst cavity and the roots of the teeth adjacent to it and, thanks to image magnification, early reveals the initial signs of root resorption. Namely, these factors are
CYSTS IN X-RAY IMAGE
sometimes decisive in the X-ray identification of cavities of various natures.
Currently, there are several classifications of cystic lesions of the jaws, which are based on histological examination data and emphasize their different nature and pathogenesis. Considering that not all forms of cysts included in the WHO classification are associated with changes in bone tissue and have radiological manifestations, we present a simplified grouping of cystic lesions, which, it seems to us, is more convenient when considering radiological indicators.
1. Cysts of odontogenic origin—radicular, keratocyst (primordial), follicular, eruption cyst (tooth-containing).
2. Cysts of non-odontogenic origin - traumatic, aneurysmal, cysts of the incisive, nasopalatine and other canals, median cyst of the lower jaw.
Of the cysts of the 1st group, in their origin, only the radicular one is associated with previous inflammatory changes in the periodontium, and the rest are defects in the formation of various tissues of the dental plate, arising at different phases of maturation of follicles or tooth germs. This explains not only the differences in the histological structure of the wall lining, but also the features of the clinical manifestations of cysts and their growth. Cysts of the 2nd group in development are also partially associated with impaired tissue formation (median cyst) of the lower jaw, but in most cases they are caused by other previous pathological processes.
K. Donath (1985), based on large clinical and morphological material, presented the following statistical data on the frequency of cysts of various origins: 80% of them are of inflammatory origin, 19% are caused by impaired tissue formation (of which 11-13% are follicular cysts, and about 18 % - keratocysts). 1% of cysts are pathogenetically associated with trauma or other mechanical effects on the maxillofacial area.
Cysts of any origin of small size, located within the cancellous bone tissue and transition zone, on radiographs have a rounded shape and a delimiting cortical rim. Increasing, they are
| CHAPTER 9 |
They determine the correct shape in accordance with the resistance of bone tissue along the path of their expansion. The cortical end plates of the jaws, especially the lower ones, most stubbornly resist the increase in cavity volume. Therefore, cysts can spread along the long axis of the jaw without causing an increase in its volume and external deformation of the face. Up to the last molars, the lingual cortical plate of the lower jaw is more massive than the buccal one, and beyond 8 | 8 - on the contrary, it is thinner, which determines the direction of increase in the cysts of the mandibular bone. As the cystic cavity grows, the teeth along its path shift, except for the “causal” ones, which do not change position. When trying to carry out differential diagnosis of cysts of various types based on X-ray indicators, it should be taken into account that the level of transparency of the cavity, the clarity of the cortical rim, and sometimes the polycyclicity of the contours is determined, first of all, by the degree of damage to the cortical plates of the bone.
Radicular cysts make up about 94-96% of cavities found in adults. They can be peri-apical and lateral and most often form at the age of 20-30. Only 2.7-3% of radicular cysts occur at the roots of primary teeth. The frequency of cysts in certain permanent teeth is parallel to their susceptibility to caries. According to I. I. Ermolaev, A. I. Rakhmetov (1965), Brown (1961), A. I. Solntsev and V. S. Kolesov (1982), these cysts are more often detected on the upper jaw, and on the lower jaw about 58% of radicular cysts are associated with molars. Back in 1892, Partsch argued that radicular cysts develop as the final stage of granulomatous periodontitis due to the proliferation of metaplastic epithelium bordering the necrotic cavity due to liquefaction of granulomatous tissue and its transformation into a mucin-like substance. In this case, the formation of a cyst is regarded as an indicator of good reactivity of the body, which results in complete separation of the inflammation zone from healthy bone tissue. The presence of a cavity containing fluid, which evenly presses on all walls, determines the geometrically correct round shape of most radicular cysts. The version about the metaplastic origin of the epithelial lining of the cyst is proven
CYSTS IN X-RAY IMAGE
Rice. 9.1. Radicular cyst in [_2
not completely covered. It is believed that the source of the epithelium may be the epithelial remains of Malasse, which are found in the periodontium of almost every tooth. This path of transformation of a granuloma into a cyst is not recognized by all authors. Thus, W. Hacker and N. Fischback (1985) carried out a histological study of 102 periodontal bone processes that had the semiotics of a rounded, delimited periodontal rarefaction, and found 63 radicular cysts, 33 granulomas and only 6 cases that could be regarded as transitional cystogranulomas. The rarity of intermediate forms forced them to speak out against the generally accepted point of view about the transition of periapical inflammation first into a granuloma and then into a cyst. The authors believe that chronic periodontitis can equally give rise to the formation of a granuloma and to the proliferation of epithelial tissue with the formation of a cystic cavity. Both the process lasts about 2-7 years.
Radicular cysts, like apical periodontitis, are themselves caused by carious lesions in only 40% of cases, and in 60% they arise as a complication of endodontic measures - pushing necrotic pulp to the apex of the tooth with the subsequent development of periodontitis, injured pulp during cavity preparation, especially under anesthesia .
| CHAPTER 9 |
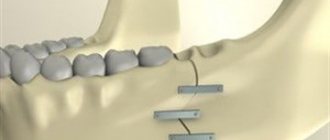
| Rice. 9.2. Large radicular cyst extending to the posterior parts of the body and the right ramus of the mandible |
Clinical and radiological manifestations of radicular wrist! are caused by the peculiarities of its development, the presence or absence of repeated inflammatory changes around the cavity, its localization, and how long it has existed. In most cases, these cysts are relatively small in size on radiographs and rarely exceed 1.5-2 cm in diameter (Fig. 9.1). According to our data, about 8% of cysts have a larger diameter. The transparency of their shadow is quite large and uniform and is caused by a violation of the integrity of one or both end plates of the jaw bones. A rim is visible along the periphery
cortical bone tissue, which has clear contours and small thickness. The cavity of the cyst may contain the root of one or more teeth. The pulp of the “causal” tooth is, as a rule, completely necrotic. Increasing in size, a radicular cyst can lose its rounded shape, stretch along the alveolar process and the body of the jaw, and can displace the roots of the teeth, bypass them, or even include them in the cavity. The vitality of the teeth and the delimiting clear cortical rim along the periphery of the cavity are preserved. With large cysts, the transparency of the cavity may become heterogeneous due to different depths of the defect in the bone tissue. The X-ray picture in these cases is not very characteristic, and the radicular cyst must be differentiated from ameloblastoma, some forms of giant cell tumor, or cysts of a different nature, for example, primordial (Fig. 9.2).
CYSTS IN X-RAY IMAGE
Rice. 9.3. Maxillary cyst at level 4321 I 1
The size of cystic lesions in the maxilla is often larger than in the mandible because the compact endplates of this bone are thinner and more easily displaced by the pressure of the contents (Fig. 9.3). Due to the significantly lower pressure resistance in the alveolar process of the upper jaw, cysts of this localization increase in all directions, which often leads to the formation of an irregularly shaped cavity. The severity of the rim in cysts of any location is often determined by the duration of the cyst's existence.
Lateral periodontal cysts were described by Shear and Pindbor (1975) and histologically studied by Whysckii et al. (1980). They originate from islands of odontogenic epithelium preserved within the gingival tissue. Such cysts can be multiple and are often located in the area of premolars and molars. A distinctive radiological feature of these cysts is that through the lumen of their cavity one can see an unchanged periodontal fissure. Reaching relatively large sizes, cysts can cause erosion of the outer cortical plate of the jaws.
Despite the fact that morphological examination reveals traces of inflammatory changes in the walls of radicular cysts in almost 82% of cases, clinical manifestations of inflammation are usually absent. Only with extensive suppuration do phlegmons
| CHAPTER 9 |
Rice. 9.4. Inflamed cyst in 6 |. local odontogenic maxillary sinusitis. Fracture of the lower jaw in the area 8~\.
Cystograph-nullema y | 2
soft tissues of the maxillofacial area. In this case, along with the remains of a thin cortical plate delimiting the cyst cavity, zones of bone tissue resorption with uneven contours are detected around it, and the cavity itself may lose its correct geometric shape (Fig. 9.4). Its transparency, however, changes little or does not change at all. The connection between cyst suppuration and the appearance of soft tissue phlegmon is explained by the fact that in the area of cysts, especially large ones, the integrity of the cortical plates of the jaw is often disrupted. Maxillary cysts, when inflamed, often involve the maxillary sinus in the process. If inflammatory complications occur repeatedly, rims of sclerotic bone tissue may develop along the periphery of the cystic cavity.
To detect the growth of cysts into the maxillary sinus, there is no need to resort to contrast maxillary sinusography, since it can be detected using orthopantomography or CT. It is most difficult to differentiate the adhesion of a cyst to the anterior wall of the maxillary sinus from its growth into the sinus cavity - this requires multi-projection X-ray examination (CT or panoramic zonography). However
CYSTS IN X-RAY IMAGE
It should be taken into account that bone defects in the walls of the sinus, as well as the cyst cavities themselves, in reality significantly exceed the size of the defects on radiographs. This is due to the parallax of the image with a decrease in size, which occurs in any type of shooting.
If, according to a single-view study, a radicular cyst looked like a very small and not always round, volumetric enlightenment at the roots of premolars or molars and no additional images were taken, in particular radiographs in oblique projections, but clinical data forced the surgeon to undergo surgical intervention, he may detect a large defect in the anterior wall or bottom of the sinus, which is not visible on radiographs. The detection of a cyst in the maxillary sinus itself does not present any difficulties, since the cyst produces a uniform darkening, shaped like a semicircle or semi-oval with a clear outer boundary. The main diagnostic difficulty is to establish whether it is odontogenic in origin or originates from the sinus mucosa itself (for example, retention). In the latter case, the cyst is not true, and there is no need for surgical intervention.
Even in the absence of any clinical symptoms of cyst suppuration, reactions of the mucous lining of the bottom of the maxillary sinuses or alveolar bay are detected on radiographs in almost 60% of those studied. In this case, local limited changes in the mucous membrane are sometimes detected while maintaining a relatively large strip of intact bone tissue between the wall of the cystic cavity and the bottom of the sinus. On orthopantomograms and panoramic radiographs of the upper jaw, one can see protrusion of the bottom of the maxillary sinus with cysts closely approaching the bottom of the alveolar bay, and sometimes usuration of the bottom with the formation of a defect, indicating the ingrowth of a radicular cyst into the maxillary sinus (Fig. 9.5). It is usually not possible to diagnose these details on linear tomo- or zonograms.
The frequent absence of any clinical manifestations of the disease in radicular cysts is evidenced by
| CHAPTER 9 |
Rice. 9.5. Radicular cyst at the palatal root | 6, usura of the bottom of the maxillary sinus. The cyst grows into the sinus
These are the results of using orthopantomography as a “screening diagnostic” technique. We found cysts in 365 out of 6000 people who had no complaints.
Not always uncharacteristic X-ray data can be clarified by the clinic, and the process is verified only by histological examination data.
Cysts can reach gigantic sizes without causing external deformation of the maxillofacial area (Fig. 9.6). According to our data, about 3% of cysts, occupying almost the entire body of the lower jaw, are accidentally discovered during an X-ray examination performed for another reason.
As the cyst cavity enlarges, the mandibular canal may be pushed down. The integrity of its walls may also be compromised. In these cases, the neurovascular bundle is found during surgery in the cystic cavity, but is separated from its contents by a connective tissue capsule. The presence of unerupted teeth in the projection of a radicular cyst can be a deceptive symptom, simulating a tooth-containing follicular cyst. This picture is more often observed in young people in the area of the lower molars
CYSTS IN X-RAY IMAGE
and is associated with the germination of unerupted tooth buds by the epithelial lining of the cyst.
If we exclude large oval cavities, then the radiological manifestations of the bulk of radicular cysts until the last decade were considered pathognomonic. The latest morphological studies indicate that it is almost impossible to differentiate a cyst and granuloma using radiographs. A cortical rim and a rounded cavity are found equally often in both processes. The detectability of the rim is greatly influenced by radiographic conditions. The dimensions and uniform transparency of the cavity are more related to each other than to the nature of the process. Percussion and odontodiagnosis data are of little help, since they can be the same in both diseases.
An increase in cyst size is not always a manifestation of true growth and proliferation of the epithelium. However, morphological data indicate that true growth is possible with radicular cysts. In these cases , radicular cysts of the upper jaw pose the greatest danger, since they can spread to adjacent cavities: the nasal or maxillary sinus In this case, cysts can either grow into the bottom of neighboring cavities or squeeze it upward, which is observed almost
Rice. 9. c. A large cyst extending along the length of the lower jaw. The mandibular bone is not deformed. Incidental radiographic finding
| CHAPTER 9 |
in 46% of cases. The growth of a radicular cyst into the maxillary sinus is not always accompanied by any clinical symptoms and may be an accidental radiological finding.
About 30% of radicular cysts are residual and remain after tooth extraction or loss. The origin of the cystic cavity in these cases is evidenced by its localization in close proximity to the socket of the missing tooth.
Lateral periodontal cysts usually occur in people over 50 years of age and are discovered accidentally during an X-ray examination. Only in cases where they are in close proximity to lingual or buccal bone grafting can a painless bony protrusion covered by intact mucosa occur. The cyst cavity is not connected to the gingival groove. On radiographs, lateral periodontal cysts are usually small in size and located near the lateral surface of the root. The tooth may retain partial vital pulp, despite the possibility of secondary periodontal infection. On histological examination, the cyst cavity is lined with epithelium with islands of keratinization, and is surrounded at the periphery by a connective tissue capsule. Histological evidence suggests that this type of cyst is a developmental malformation, associated with odontogenic epithelium and has nothing in common with a laterally located radicular cyst, although it is very difficult to distinguish from it.
Keratocyst (primordial cyst) was previously combined into one group with follicular cyst. According to statistics from V. Lund (1985), keratocysts make up 11% of all odontogenic cysts. Their formation is associated with degenerative changes in the stellate epithelium at that stage of maturation of the tooth germ when its dense tissues have not yet differentiated. Therefore, this type of cyst is often not tooth-containing. However, developing near the developing follicle, the cyst can be separated from it only by a connective tissue capsule. In these cases, a false impression is created of the presence of a tooth germ in its cavity.
A distinctive feature of these cysts is the keratinization of the epithelium lining their cavity. Inflamed-
CYSTS IN X-RAY IMAGE
| Rice. 9.7. Keratocyst in the area in~\ |
There are no significant changes in the walls. Keratocyst can be single- or multi-chamber. In the latter case, next to the main, rather large cavity, small, poorly distinguishable cystic formations may be located, separated from it by strands of unchanged bone tissue, which perhaps explains the tendency for cyst recurrences if there is insufficient
radical removal. Cysts of this type are found in people of different genders and ages, but more often in men. There are two age peaks for their detection - between 10 and 20 years and after 50 years. Late-detected cysts may also have developed at a young age, but had an asymptomatic course for a long time.
The localization of keratocysts can be different, but most often they are located behind the 8 | 8 in the area of the angle and ramus of the lower jaw, where about 75% of formations of this type are detected. In the upper jaw, keratocysts are mainly localized in the molar area and can spread to the maxillary sinus. Keratocysts often penetrate into the interdental spaces, and their cavity may have partitions. Located within the dentition, the Keratocyst displaces the teeth, but does not cause root resorption or pulp necrosis (Fig. 9.7).
With numerous keratocysts, one should suspect congenital Gorlin-Goltz syndrome and look for basal cell nevi in various areas of the skin, as well as skeletal dysplasia. Multiple primordial cysts are located in different parts of the same jaw or in both jaws.
The growth potential of keratocysts is different - sometimes they are an accidental finding even with large cavity sizes, and sometimes they increase very quickly, sharply thinning the cortical plates of the lower jaw, leading to their fracture. Rapid growth is typical for individuals
| CHAPTER 9 |
young people, however, even in these cases the cyst usually does not grow into soft tissues. As it grows, it increases in the anteroposterior direction more than in the mesio-distal direction. Therefore, large cysts not only lead to the appearance of a well-defined, smooth bulge, but can also limit mouth opening.
X-ray manifestations of keratocysts have nothing characteristic. The transparency of the cavity, as with other types of cysts, depends on its size and the degree of erosion of the cortical plates. The keratocyst, like other types of cystic formations, is delimited from the surrounding unchanged bone tissue by a thin, clear bone rim. Swelling of the affected area of the bone may be completely absent, or it may be pronounced. Therefore, clarifying the nature of the cyst often requires histological data. At the same time, morphological indicators may not always be reliable, especially if the researcher does not have sufficient experience. In the literature of recent years, there are reports whose authors discovered keratocysts during a retrospective review of specimens for which other diagnoses had previously been established. The recurrence rate of keratocysts after their surgical removal varies from 13 to 45%.
Follicular cysts, according to pathologists, make up about 6% of all cystic lesions and are a consequence of impaired differentiation of tooth germ tissues. As a rule, these disorders occur at the stage of formation of the dental papilla, but occasionally at the stage of development of the primitive dental plate. In the latter case, the cyst may not contain a tooth, and its cavity may contain the roots of nearby intact teeth. A follicular cyst is associated in its development with the epithelium of the enamel organ and is most often formed at the stage of formation of tooth crowns (Fig. 9.8). Some authors consider an eruption cyst to be a variant of a follicular cyst. In the early stages of formation, this cyst may appear radiographically as an enlargement of the pericoronal space around an incompletely formed
^/pp. tt 853 | 358 teeth (Fig. 9.9). Most often located in the os-o oso zone>
oyo 000
CYSTS IN X-RAY IMAGE
Fig 98 Follicular cyst in |_3
however, it can come from any other tooth. Typically, a follicular cyst begins to form after differentiation of the hard tissues of the crown in early childhood and slowly increases due to the accumulation of fluid between the capsule and the follicle. Small cysts are an accidental x-ray finding, while large ones lead to the appearance of a painless swelling. Parchment crunch is usually absent. Occasionally, follicular cysts are multiple.
X-ray diagnosis, as a rule, does not present any difficulties. A follicular cyst has the appearance of a round or ellipsoidal cavity with clear, slightly wavy contours. The transparency of its shadow is uniform and very high. In the lumen there are 1 or 2 tooth buds at varying degrees of maturation. Moreover, if an almost completely formed tooth is located in the cavity of the cyst, its roots may be located outside the walls. Since the fluid pressure in the lumen of the follicular cyst exceeds the forces of eruption, the tooth germ is usually located at the bottom of the cystic band, and the crown faces the lumen. Unlike radicular cysts, the teeth in the cavity of follicular cysts are alive.
The presence of an incompletely formed tooth is not an absolute sign of a follicular cyst, since
| CHAPTER 9 |
Rice. 9.9. Multiple eruption cysts in an 11-year-old child
tumors and cystic formations of a different nature, developing near the tooth germs, can merge with them.
Follicular cysts can become inflamed. At the same time, they lose the high and uniform transparency of the shadow. When the cystic cavity is opened, purulent contents are found in it. The cortical plates melt in places, and after the end of the inflammatory process they can thicken again.
The ease of diagnosing follicular cysts can be deceptive. Especially many errors occur in cases where the cyst is first discovered in middle-aged and older people and does not contain a tooth. Difficulties also arise in children and adolescents in distinguishing a cyst from a large follicle, especially in the premolar area. In doubtful cases, observation of the patient is recommended. If repeated X-ray examinations reveal tooth eruption, a follicular cyst should be excluded. Some experts suggest considering all follicles larger than 2.5 cm in diameter as a cyst. Moreover, if the forces of tooth eruption exceed the fluid pressure in the cavity and the crown manages to reach the alveolar edge, the cyst is called a tooth-containing or eruption cyst.
Rare cystic formations include the median cyst of the lower jaw, developing from the remains of
CYSTS IN X-RAY IMAGE
epithelium of the dental plate at the level of the symphysis, as well as a globulo-maxillary cyst, which has the appearance of an incomplete cleft of the upper jaw and occurs in the zone of embryonic “gluing” of jaw fragments.
The genesis of traumatic cysts is not entirely clear, since it is not always possible to detect a history of trauma in their owners. Some authors associate the appearance of traumatic cysts with inadequate mechanical load, in particular during orthodontic treatment. Having no epithelial lining in the cavity, traumatic cysts are false. They are usually located on the lower jaw in the area 654111456, and on the upper jaw - at 54 | 45 (Fig. 9.10). The cyst cavity contains blood or serous-bloody contents, has a round or oval shape, and fairly clear contours. Its wall is a thin connective tissue capsule. These cysts are usually asymptomatic and are a radiological finding, more often found in adolescents and young adults. Traumatic cysts do not cause root usuration or necrotization of the dental pulp. Some authors point out their connection with avascular bone zones, which are sometimes found in the jaw bones, while others consider them to be a consequence of solitary hemorrhages [Blue V.,
Fig. 9 10 Traumatic cyst that developed after dislocation 1 | 1
| CHAPTER 9 |
1968]. Isolated cases of pathological fracture of the mandibular bone in the area of the traumatic cyst have been described.
Naso-palatal cyst is quite common, according to W. Petri et al. (1985), in 1% of all people. It develops from proliferating remnants of the epithelium of the embryonic naso-palatal duct and is located inside the connective tissue canal. The cause of its occurrence may be infection of the nasal canal. As a rule, a non-inflamed cyst does not give any manifestations and is detected by chance on photographs of the central teeth of the upper jaw or upper panoramic radiographs. In these cases, any increase in the diameter of the clearing of the incisive canal over 0.7 cm is considered as a manifestation of brush!. The cyst cavity does not always have the correct rounded shape in the images, which is explained by image distortion when the X-ray beam is tilted. A clear, even cortical rim is not always visible and not along the entire perimeter of the cyst, which is also explained by the skialological features of the image (Fig. 9.11). The roots of the central teeth and the cortical lining of the sockets can be traced through the highly transparent cavity, which makes it possible to distinguish this cyst from a radicular one. When inflamed, naso-palatal cysts cause a bulge on the palate, pain and discharge of pus into the oral cavity.
Rice. 9.11. Incisive canal cyst
CYSTS IN X-RAY IMAGE
The median palatal cyst, on the contrary, is very rare, is located in the area of the upper premolars or molars and is usually surrounded by a clear cortical rim.
The radical method of treating cysts of odontogenic origin is surgery. The presence of epithelial lining in radicular cysts prevents the restoration of bone tissue under the influence of endodontic measures. After surgical treatment with removal of the cyst shell, its cavity is gradually filled with bone tissue, which is formed starting from the peripheral parts. The rate of restoration of normal bone structure depends on the location of the cyst, the age of the patient, the surgical procedure and the use of osteogenesis-stimulating drugs during the procedure - ostima, colapol, bone chips. On average, in the absence of complications, significant replenishment of the cyst cavity with bone tissue can be observed after 3 months.
If the operation is not radical enough, there remains a part of the cavity not filled with bone tissue, which can again increase in size due to the inflammatory process.
Aneurysmal bone cysts occur in children and adolescents. They are characterized by fairly rapid expansive growth. In this case, the periosteum irritated by pressure can produce bone layers on
Rice. 9.12. Aneurysmal bone cyst. Resorption of the cortical plate of the lower jaw from the inside, displacement and resorption of the root 5″). Layering of cortical bone tissue at the base of the mandible
| CHAPTER 9 |
cortical plate, creating a “variegated” radiological characteristic of this hand! with erosion of the end plate from the inside and thickening from the outside (Fig. 9.12).
As can be seen from the presented X-ray characteristics of cysts of various origins, there are not many clear signs that allow them to be differentiated from each other. It is also not always possible to distinguish a cystic cavity from a zone of tumor resorption, but it should be taken into account that in the presence of bone tissue partitions in the clearing cavity, compactions in the lumen, hypercementosis of the root, one can be more confident in favor of a tumor or a dysplastic process. Not a single type of cyst has a characteristic clinical picture. At the same time, cysts lined with keratinizing epithelium have a more malignant course and are prone to relapse. Occasionally, it is possible to detect elements of ameloblastoma in the walls of follicular cysts, so it is recommended to carefully carry out histological examination in those areas of their walls where there is even the slightest unevenness of the cellular composition.
CHAPTER 10
X-RAY
STUDY
FOR SOME CONGENITAL
AND ACQUIRED DEFORMATIONS
FACIAL SKULL
Deformations of parts of the facial skull are a consequence of changes in the shape, size and relative position of its bones and are not uncommon. They develop due to various reasons: past illnesses or traumatic injuries; disorders of the formation or growth of the bone parts of the skull caused by hereditary factors, chromosomal diseases, teratogenic effects on the developing organism, endocrine or metabolic disorders, etc. The combination of changes of such different origins into one group is due to the fact that at present their treatment is more dependent from certain anatomical changes, malocclusion or functions of vital organs that arise as consequences of deformation, rather than from etiopathogenetic causes leading to them. As a result, deformations of the facial skull are distinguished as if into an independent nosological unit.
X-ray examination for all types of deformities plays the role of the most important diagnostic tool, allowing one to recognize their specific individual manifestations, determine in some cases the etiology and pathogenesis of changes, plan and objectively monitor complex therapy and predict its results.
There is no single generally accepted classification of deformities. We believe that the following grouping is quite convenient for practice, including for discussing radiological characteristics:
I- Congenital deformities - clefts, discrania and craniostenosis, syndromes of the I and II branchial arches, phacomatoses, chromosomal diseases.
| CHAPTER 10 |
II. Acquired deformities - post-traumatic, post-inflammatory, post-radiation, deformations of endocrine and metabolic origin.
In relation to the dental system, there is a WHO classification (IX revision), which is widely used in maxillofacial surgery and which we will also use to describe radiological changes. According to this classification there are:
Maxillary cysts
According to statistics, most neoplasms are localized in the upper jaw.
Maxillary neoplasms arise due to inflammatory processes, the prerequisites for which are:
- The presence of untreated teeth or their roots.
- Mobility of teeth.
- Injuries to the teeth or jaw itself. These neoplasms are characterized by minor pain, bleeding, and pressure on the nasal cavity. This group includes radicular (located at the root of the tooth) and residual cysts.
What provokes
The appearance of a cyst in the projection of the root part of the tooth is due to the inflammatory process, which mainly occurs during chronic granulomatous periodontitis. Trying to delimit the source of infection at the stage of development of complicated caries, a granuloma is initially formed.
The latent course, reinforced by the action of toxins secreted by microbes, provokes the development of cystogranuloma from granuloma and then cysts.
Features of the concepts of destructive formations in the area of the apex of the tooth depending on the size:
| Name | Size, mm |
| Granuloma | Up to 5 |
| Cystogranuloma | 5-8 |
| Cyst | More than 8 |
Histological structure of destruction associated with the tooth root.
A radicular cyst may appear due to the following reasons:
- infectious: long-term caries, pulpitis, periodontitis (especially destructive forms);
- iatrogenic: disturbances in the process of preparation and filling of root canals;
- traumatic: bruise, subluxation, dislocation, fracture in the maxillofacial area;
- difficulties in the process of erupting the eighth teeth;
- pathological bite: due to improper distribution of chewing pressure;
- systemic pathology: sore throat, otitis media, sinusitis;
- immunodeficiency state.
Occurs against the background of paste removal beyond the apical region of the tooth.
Features of the pathology
A radicular cyst, also known as a perihilar cyst, is represented by a hollow formation lined from the inside with squamous epithelium. The cavity is filled with a light yellow liquid.
The cavity contains:
- linear calcifications: Rushton bodies;
- hemorrhages: can be in the wall itself;
- siderophages in large numbers;
- cholesterol crystals;
- infiltrate of inflammatory origin: composed of giant multinucleated cells. During an exacerbation, the number of neutrophil granulocytes increases; during remission, macrophages and lymphocytes predominate.
Most often the disease is registered at the age of 20-45 years. In the upper jaw, their occurrence is more common compared to the lower jaw, since there are anatomical prerequisites for development: bone porosity, close location of the maxillary sinus.
Position of the maxillary sinus relative to the dental arch.
By localization:
- apical: located in the area of the apex of the tooth;
- lateral: in the lateral part of the periodontal ligament.
The location of destruction is in the apical region with transition to the lateral region of the root.
Based on topography, this pathology is more often diagnosed at the apex. This is due to the fact that the main provoking disease in the form of chronic periodontitis originates through the tooth cavity, and not the periodontal pocket.
Lower jaw cyst
These include residual, follicular and radicular cysts. They differ in that they cannot affect the nasal cavity. However, despite the fact that the lower jaw is the most distal part of the skull, the nerves here are thicker and more sensitive than in the upper jaw (this is also associated with increased sensitivity of the teeth). This type of neoplasm does not require special treatment approaches.
Possible complications
If the cyst is not diagnosed and treated in a timely manner, this is fraught with the following consequences:
- Increased pain while chewing food.
- The appearance of swelling.
- Development of periostitis.
- Transition to the stage of purulent inflammation to such a degree that there is a danger of threatening the patient’s life.
- Most patients find out that they have a dental cyst only when severe pain begins. Regular preventive examinations at the dentist allow you to promptly detect the presence of a tumor and begin adequate treatment.
To prevent the development of tumors, it is necessary to visit the dentist every six months to heal caries. You should not bring your condition to such an extent that it becomes impossible to endure the pain of a dental cyst.
Treatment and removal
Treatment usually involves surgical removal of the formation. The cyst can be removed with the membrane (cystectomy) or without it (cystotomy). In the first case, dissection with a scalpel is necessary, in the second it is enough to pierce the membrane and suck out the liquid using a special syringe.
Cystectomy is used for large cysts, when more than three teeth are affected, as well as in the presence of chronic diseases and bone deformities. Cystotomy is used as a treatment for small cysts.
Alternative treatment for dental cysts
Another method of treatment is used if root canal treatment does not give the desired result. Apical surgery is also relevant for the treatment of anterior tooth cysts, since the bones in the frontal zone are not as thick as in the area of the posterior roots. The technique involves removing the contents of the cyst and the infected area of the tooth root. After this, the specialist fills the tooth from the inside and sews up the incision. If apical surgery did not allow the patient to forget about the problem, and after the treatment another cyst has formed, the tooth must be completely removed, and then it is recommended to install an implant in its place. Thus, modern dentistry is aimed at carrying out tooth-preserving procedures (even in the presence of a wisdom tooth cyst), and only if they are ineffective is removal of the pathological root and an expensive procedure - implantation. Remember, traditional medicine is not able to stop the development of the inflammatory process - even the strongest drugs from the group of antibiotics and antiseptics cannot cope with this. Therefore, the only method to solve the problem is to remove all affected areas, as well as high-quality treatment and filling of the root canals.