Leukoplakia of the cervix is a disease in which changes occur in the epithelium lining the cervix with its thickening and keratinization. During a visual examination of the cervix, elevated areas of whitish or gray color visible to the eye can be noted, which are later found in the cervical canal. Leukoplakia has a special place among other gynecological pathologies, since it refers to a precancerous condition of the genital organs and, in the absence of timely treatment, often develops into cervical cancer.
Kinds
The outcome of the disease leukoplakia and the methods used for its treatment largely depend on timely diagnosis and the stage of development characteristic of the disease at the moment. There are several forms of leukoplakia and each of them has its own characteristic features:
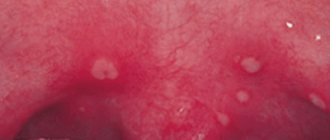
- A simple or flat form of leukoplakia, when whitish plaques are found that do not rise above the surface of the organ . This stage of the disease does not have symptoms that can attract attention to the disease; its manifestations are so insignificant that the gynecologist may not notice the changes in the mucous membrane that have occurred.
- A scaly or warty form of leukoplakia, with clearly visible elevated areas of altered dense epithelium. With several foci, the plaques layer and form a bumpy surface. It is very easy to detect the disease at this stage and it is necessary to perform a biopsy, since it is this stage of leukoplakia that can turn into a malignant form. Sometimes epithelial cells begin to change their shape and size, causing cellular atypia. The reasons for such degeneration and malfunction are not fully understood, but it is considered a precancerous condition.
- An erosive form of leukoplakia with the appearance of white areas surrounded by erosive tissue or cracks.
Leukoplakia of the cervix: what is it, can it develop into cancer and how to treat it?
The theory of the hormonal origin of leukoplakia was put forward in the 60s of the twentieth century. According to it, the main cause of hyperplasia (proliferation) of pathological tissues is progesterone deficiency and excess estrogen. This hormonal imbalance occurs due to ovulation disorders in the ovaries. Anovulation develops with any disorders in the hypothalamic-pituitary system, ovaries or uterus.
cervical injuries (during childbirth, abortion, rough sexual intercourse);
Diathermocoagulation is widespread, but it has a number of side effects. After this procedure, it is possible to develop implantation endometriosis. At the moment of rejection of the crust formed after cauterization, there is a high probability of bleeding and pain. There is also a risk of relapse of the disease.
Can cervical leukoplakia go away on its own?
Cauterization with the drug "Solkovagin"
Timely and adequate treatment of leukoplakia gives a positive result. However, the occurrence of relapses of the disease cannot be excluded. Therefore, the patient needs further observation. You should be careful when using traditional methods of treatment and thermal procedures. They can contribute to the malignant transformation of leukoplakia and aggravate the course of the disease.
The prognosis for flat leukoplakia without atypia and deformation of the cervix is favorable for both life and pregnancy.
There are a number of signs by which one can suspect malignant transformation of one or another form of leukoplakia. Such signs include the sudden appearance of compactions or erosions in the focus of flat leukoplakia, its uneven compaction, covering only one edge of the lesion. For the erosive form, signs of malignancy are: the appearance of compactions in the center of erosion, ulceration of the surface, the formation of papillary growths, a sharp increase in the size of erosion. It should be noted that the absence of these signs is not a guarantee of the benign quality of the process and can be observed in the early stages of malignant degeneration of leukoplakia.
Endogenous factors include:
Chemical cauterization of cervical leukoplakia with the drug “Solkovagin” is still used. This drug causes coagulation (cauterization) of the epithelium. The medicine penetrates to a depth of 2 mm, which contributes to the destruction of the lesion. Treatment with Solkovagin is painless. In young nulliparous patients with simple leukoplakia, the effectiveness of such therapy exceeds 70%.
Herbal treatment for leukoplakia is permissible only in order to improve hormonal balance and general condition and includes red brush, hogweed, and white cinquefoil. Courses of adaptogens – lemongrass, eleutherococcus, and Rhodiola rosea – can be beneficial.
Causes of the disease
There are a great many reasons that can cause such pathological deviations and not all of them are fully understood. But some of this number have been identified that can provoke the development of leukoplakia:
- infectious diseases of the genital organs with a complicated course, including those acquired through sexual contact;
- hormonal imbalances, expressed in an imbalance between estrogen and progesterone;
- immunodeficiency;
- injury to the cervix caused by surgical interventions or during medical procedures on the genitals;
- advanced gynecological diseases that have not received timely and correct treatment, most often pseudo-erosion of the cervix.
In women of reproductive age, leukoplakia occurs in 1 percent out of 100, and the overall incidence of this pathological disorder among all cervical diseases reaches 12%.
All the many reasons that can become an impetus for the development of leukoplakia are divided into two directions - endogenous and exogenous. Endogenous disorders include hormonal disorders caused by a lack of progesterone, while exogenous disorders depend on infections, injuries and chemical exposure.
The above factors cause processes that include the mechanism of cell keratinization, leading to keratinization of the cervical epithelium.
Interesting video:
LEUKOPLAKIA OF THE CERVIX
The occurrence of cervical cancer in women of reproductive age is preceded by inflammatory processes of the uterus and appendages, menstrual dysfunction, and chemical and traumatic effects are of great importance. A comprehensive examination for FSM includes clinical, colposcopic, cytological, morphological, as well as bacterioscopic and bacteriological methods. Currently, many different methods of treating patients with cervical cancer have been proposed. The most effective methods of treating FSM today include the cryogenic method and especially high-intensity laser exposure. Uterine cervical leukoplasia (UCL) occupies a special place in the structure of diseases of the uterine cervix. Its etiology and pathogenesis has been so far controversial. The occurrence of UCL in reproductive females follows prior inflammations of the uterus and appendage, impaired menstrual function; chemical exposures and injuries are also of great importance. Comprehensive study in UCL involves clinical, colposcopic, cytological, morphological, bacterioscopic and bacteriological methods. Many different treatments for UCL have been proposed. At present, the most effective treatments are cryogenic therapy and especially high-intensive laser radiation.
V.N.
Prilepskaya - Prof., Doctor of Medical Sciences, Head of the outpatient department of the Scientific Center of Obstetrics, Gynecology and Perinatology (Director - Academician of the Russian Academy of Medical Sciences Prof. V.I. Kulakov), Russian Academy of Medical Sciences, Moscow
Prof. VN Prilepskaya, Dr. Sci., Head of Outpatient Department, Research Center of Obstetrics, Gynecology, and Perinatology, (Director Prof.VIKulakov, Academician of the Russian Academy of Medical Sciences), Russian Academy of Medical Sciences
L
Cervical neucoplakia (CMP) occupies a special place in the structure of cervical diseases, since the issue of its pathogenesis, benignity or malignancy of the course is still controversial. According to modern data, cervical cancer is a polyetiological disease and is based on many predisposing factors: previous infectious diseases, disorders of the immune status, hormonal homeostasis, traumatic effects on the cervix during childbirth, abortion, incorrect and inadequate treatment of cervical pathology and many others. Currently, the oncological aspect of gynecological diseases is considered inextricably linked with the endocrine function of the reproductive system. Data have emerged on the role of functional hormonal disorders in the pathogenesis of cervical diseases. Thus, the works of a number of authors have proven that the incidence of cervical diseases in patients with menstrual dysfunction is 5 times higher than among the general population [1]. Data on the frequency of leukoplakia in the structure of cervical diseases are contradictory [1–4]. Some researchers note a high incidence of this disease – from 11.7 to 12.5% [2, 5, 6]. According to M.Yu. Novikova [7], the frequency of cervical cancer is 1.1%, and in the structure of cervical diseases it accounts for 5.2%. And although this pathology does not occur very often, malignant transformation of stratified squamous epithelium (MSE), according to some researchers [2], is observed in 31.6% of patients with cervical cancer; in this regard, timely diagnosis and treatment of this disease is an important preventive measure and reducing the incidence of cervical cancer. The term “leukoplakia” (translated from Greek means “white plaque”) was first proposed by Schwimmer in 1887 and remains generally accepted to this day in Russian literature and clinical practice [2]. An analysis of foreign literature over the past 10 years has shown that the term “leukoplakia” itself in relation to lesions of the cervix is not used in some countries, while for leukoplakia of other localizations (vulva, oral mucosa) this term is widely used. Leukoplakia without cellular atypia, the so-called simple leukoplakia, is classified by foreign researchers as hyper- and parakeratosis [4], and leukoplakia with dysplasia atypia is classified as “cervical intraepithelial neoplasia” (CIN) [8 – 10].
Etiology and pathogenesis
In the etiology of FSM, it is customary to distinguish the following groups of factors: – endogenous (disturbance of hormonal homeostasis, changes in immune status); – exogenous (infectious, chemical, traumatic). In the 1960s and 1970s, the theory of hormonal genesis of underlying diseases of the cervix and leukoplakia in particular began to develop. As a result of functional disorders in the hypothalamus - pituitary gland - ovaries - uterus system, the ovulation process is disrupted. The consequence of anovulation is relative or absolute hyperestrogenism and progesterone deficiency, leading to the development of hyperplastic processes in target organs. The occurrence of cervical cancer in women of reproductive age is preceded by inflammatory processes of the uterus and appendages against the background of menstrual dysfunction such as oligomenorrhea in 35.5% of patients and by the type of defective luteal phase of the cycle (in 64.5%). According to M.Yu. Novikova [7], in patients with cervical cancer the function of the pituitary-ovarian system is impaired. Chemical and traumatic effects also play an important role in the occurrence of cervical cancer. It has been proven that more than 1/3 of patients with cervical cancer had previously received intensive and inadequate drug treatment for pseudo-erosion of the cervix, and 33% of patients with clinically significant leukoplakia had previously undergone diathermocoagulation [7]. Thus, patients with menstrual irregularities, previous inflammatory diseases of the genital organs, and a history of recurrent pseudo-erosions of the cervix should be included in the risk group for the occurrence of cervical cancer.
Clinical manifestations and diagnosis
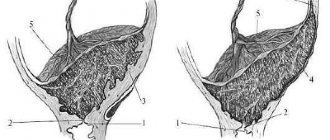
Clinical examination data are of great importance. When analyzing anamnesis data, attention is paid to the nature of menstrual function (age at menarche, duration of the period of formation of menstrual function, rhythm of menstruation, etc.), the presence and outcome of pregnancies, the presence of a history of cervical pseudo-erosions, as well as the nature and effectiveness of previous therapy , duration of the FCM disease. Noteworthy is the asymptomatic course of the disease, as well as the absence of specific complaints. Only a small number of women complain of profuse leucorrhoea and contact spotting. A comprehensive examination for cervical cancer includes clinical, colposcopic, cytological, and, if indicated, morphological, as well as bacterioscopic and bacteriological methods. The most informative are extended colposcopy and morphological research methods. Extended colposcopy allows you to clarify the size and nature of leukoplakia, assess the condition of the integumentary epithelium of the vaginal part of the cervix. Depending on whether leukoplakia is detected only during colposcopy or is visible to the naked eye, colposcopically and clinically pronounced forms are distinguished. The colposcopic form includes “silent iodine-negative zones”, which can only be diagnosed using the Schiller test, and the clinically pronounced ones include “simple leukoplakia”, “base of leukoplakia” and “fields of leukoplakia”. Colposcopic forms of leukoplakia are described in various domestic and foreign guidelines on colposcopy [2, 3, 11]. Until now, the clinical-endoscopic-morphological classification of I.A. is generally accepted for clinicians. Yakovleva and B.G. Kukute [5], according to which simple leukoplakia without atypia is classified as background processes, and leukoplakia with atypia is classified as precancerous conditions. Some authors classify simple leukoplakia as hyper- and parakeratosis, and leukoplakia with cellular atypia as CIN of varying severity, which depends on the severity of atypia. Simple leukoplakia is a thin white film that can easily peel off, or dense lumpy plaques with clear contours. The external manifestations of simple leukoplakia depend on the thickness of the keratin layer. After its removal, shiny pink areas are visualized, indicating the true size of the lesion, the Schiller test is negative, the vessels are not visible, since leukoplakias are devoid of vessels. The base of leukoplakia colposcopically looks like an iodine-negative area covered with red dots of equal size. Red dots represent connective tissue papillae in stratified squamous epithelium, in which loops of capillaries are visible. Mosaic or fields of leukoplakia during colposcopy look like polygonal areas separated by red threads of capillaries, creating a mosaic pattern. When treated with acetic acid, the mosaic pattern becomes more distinct, the Schiller test is negative. For the purpose of early diagnosis of cervical cancer, impression smears from the surface of the integumentary epithelium of the cervix are examined. It is convenient to take material for cytological examination with an Eyre spatula or a special cervical brush. At the same time, smears are taken from the vaginal part of the cervix, transition zone and the lower third of the cervical canal. However, due to the presence of the stratum corneum on the surface of the MPE, cells with dyskaryosis from the deep layers, where differentiation disorders, proliferation and atypia are possible, are not included in the smears. Dyskaryosis is characterized by the following features: an increase in the nuclear-cytoplasmic ratio, size, change in the shape of the nuclei, unevenness of their contours, hyperchromasia, multinucleation and the presence of numerous nucleoli in the nuclei. With simple leukoplakia, the impression smears contain clumps of keratin, accumulations of superficial cells devoid of nuclei, the cytoplasm of which is stained yellow or orange using the Papanicolaou method. The smears also contain layers of polygonal keratinizing cells with a pyknotic nucleus of irregular shape - dyskeratocytes. The main method for diagnosing cervical cancer is a morphological examination of a cervical biopsy.
For its high-quality implementation, it is necessary to perform a targeted knife biopsy under colposcopy control from the affected areas of the cervix. Simultaneously with the biopsy, the mucous membrane of the cervical canal is scraped. The need for revision of the cervical canal is due to the fact that the pathological process can develop not only on the vaginal part of the cervix, vagina and vulva, but also in areas of squamous metaplasia of the mucous membrane of the cervical canal. Therefore, to exclude precancerous changes and malignant transformation of the epithelium, it is necessary to include curettage of the endocervical mucosa in the complex of diagnostic measures. The morphological picture of leukoplakia is characterized by the following structural changes in the MPE: •thickening of the integumentary epithelium, mainly due to an increase in the number of cells of the spinous layer while maintaining their complexity; it may be caused by acanthosis - immersion of epithelial layers into subepithelial connective tissue; •the presence of a stratum corneum on the surface of the epithelium, which is normally absent; •the presence of a granular layer, which is located under the stratum corneum and is represented by 2–3 rows of cells, the cytoplasm of which is filled with a moderate amount of basophilic granules; •scattered or focal lymphoid infiltration of subepithelial connective tissue. In areas of leukoplakia, glycogen is always absent. Also, with leukoplakia, parakeratosis is quite common - incomplete keratinization of the MPE. In this case, the surface layer of MPE is represented by several rows of flattened cells, elongated parallel to the base, with small pyknotic nuclei and oxyphilic cytoplasm. Under the parakeratosis, the granular layer is absent. In areas of parakeratosis, glycogen is either not detected or traces of it are visible. In the histological assessment of leukoplakia of any localization, the presence or absence of cellular atypia in the lower layers of the MPE is very important. As already mentioned, leukoplakia without atypia is a benign lesion of the cervix and refers to background diseases, and in the presence of atypia - to precancerous conditions, and is also classified as cervical dysplasia depending on the severity of atypia. In recent years, microcolpohysteroscopy has been used for a more detailed examination of the cervix and cervical canal. The advantages of this method are the possibility of atraumatic passage of the cervical canal under constant visual control, without any anesthesia. Microcolpohysteroscopy allows you to assess the condition of the walls of the cervical canal in patients with cervical cancer, detect atypical cells, and perform a targeted biopsy.
Treatment
Currently, many different methods of treating patients with cervical cancer have been proposed. From the arsenal of means available to practitioners, the most commonly used are diathermocoagulation, cryogenic exposure, high-intensity laser radiation, and various medicinal methods based on the general or local effect of drugs on the pathologically altered cervix. Until now, clinicians have difficulty managing and treating such patients. It should be emphasized that when FSM is combined with inflammatory processes of the vulva and vagina of various etiologies, it is first necessary to eliminate the inflammatory process, for which antibacterial drugs of various spectrums of action, antitrichomoniacal, antifungal, antiviral, antichlamydial agents should be prescribed according to the regimens generally accepted in clinical practice in accordance with preliminary data bacterioscopic and bacteriological examination, as well as the results of examination for chlamydia and viruses. Doctors should be warned against using products that affect tissue metabolism (sea buckthorn oil, rosehip oil, ointment containing aloe, etc.). These drugs can enhance proliferative processes and the occurrence of cervical dysplasia. Chemical coagulants are still used for the treatment of LSM. Of this group of drugs, Solkovagin deserves special attention, which is a mixture of organic and inorganic acids and has a coagulating effect selectively on the columnar epithelium. The penetration depth of the drug reaches 2.5 mm, which is sufficient for coagulation of the pathological area of the ectocervix. Treatment with solkovagin is painless and ensures complete destruction of the pathological focus due to a sufficient depth of penetration. The effectiveness of treatment of simple LSM with this method in young nulliparous women was 74.3% [1]. Diathermocoagulation is still widely used in everyday practice. However, according to long-term clinical observations, this method produces unwanted side effects. These include: implantation endometriosis, bleeding at the time of scab rejection, exacerbation of inflammation of the uterine appendages, menstrual dysfunction, pain syndrome, prolonged course of reparative processes, frequent relapses of the disease. The most effective methods of treating FSM today include the cryogenic method and especially high-intensity laser exposure. Cryotherapy causes necrosis of the pathological focus due to the influence of low temperature. It is carried out by contact method, most often once, its duration is determined by the nature and extent of the pathological process and ranges from 2 to 5 minutes. The advantages of this method include the painlessness of the procedure and the possibility of use on an outpatient basis. The effectiveness of this treatment ranges from 54 to 96%. One of the disadvantages of the method is the recurrence of the pathological process, especially in patients with menstrual irregularities. One of the most modern and effective methods of treating cervical cancer is the use of high-intensity laser. The advantage of the CO2 laser is its ability to contactlessly, painlessly, aseptically, bloodlessly evaporate, burn and coagulate pathological tissues, forming a thin coagulation film on the wound surface that prevents infection from penetrating into the underlying tissues. As a rule, laser coagulation is performed on an outpatient basis without prior anesthesia in the first half of the cycle (on the 4th – 7th day). Before laser exposure, the cervix is treated with Lugol's solution to more accurately determine the area of pathological tissue to be removed. In case of extensive damage to the cervix with the spread of leukoplakia to the fornix and vagina, it is advisable to use two-stage laser radiation: Stage I - laser coagulation of the vaginal part of the cervix; Stage II – removal of the pathological epithelium of the vagina (performed during the next menstrual cycle). Complete epithelization occurs on the 16th – 40th day, depending on the prevalence and extent of the process. In cases of combination of leukoplakia with pronounced deformation and hypertrophy of the cervix, it is advisable to use surgical methods of treatment - knife or laser conization, wedge-shaped or cone-shaped amputation of the cervix, reconstructive plastic surgery with restoration of the normal anatomy of the cervical canal. Thus, currently in the arsenal of doctors there is a sufficient number of methods for treating cervical cancer, which, of course, should be used differentiatedly. However, none of these methods are perfect. It should be emphasized that preference for this pathology should be given to laser coagulation.
Prevention
The principles of prevention of cervical cancer include rational treatment of previous background processes in the cervix, excluding the traumatic effects of diathermocoagulation and chemical coagulates on the ectocervix, as well as timely treatment of inflammatory processes of the genital organs and menstrual irregularities. Patients with a history of exposure to the cervix with diathermocoagulation and chemical coagulates due to previous pathological processes require dynamic monthly colposcopic monitoring, especially during the first year after local exposure to the cervix.
Literature:
1. Prilepskaya V.N., Kostava M.N., Nazarova N.M. // Obstetrics. and gin. 1992. - No. 12. — P. 62-5. 2. Vasilevskaya L.N. Colposcopy. – M.: Medicine, 1986. – 157 p. 3. Prilepskaya V.N., Rogovskaya S.I., Mezhevitinova E.A. Colposcopy. M.: Medicine, 1997. – 108 p. 4. Boon ME., Suurmeijer AHH. The PAP Smear. Coulomb Prees Leyden 1991;77-82. 5. Yakovleva I.A., Kukute B.G. // Arch. Pat. 1977. – T. 39. – No. 1. — P. 18-25. 6. Burk CE., Henderson PH. Amer J Obstret Gynec 1963;21,(3):279-90. 7. Novikova M.Yu. Author's abstract. diss. Ph.D. honey. Sciences - 1995. 8. Burghardt E. Kolposkop. Stuttgart: New York, 1981; 253. 9. Cartier R. Practical Colposcopy. – Gustav Fischer Verlag: Stuttgart, New York, 1984;114-438. 10. Coupez F J Gynecol Obstet 1976;5 (3):177-8. 11. Prilepskaya V.N., Novikova M.Yu., Ezhova L.S. .// Obstetrics and gyne. – 1994. – No. 3. — P. 6-9.
Signs
Leukoplakia does not have pain symptoms, since there are no pain receptors on the cervix, and this disease does not differ in other characteristic manifestations. Only occasionally do women notice more abundant discharge from the genitals. Leukoplakia is most often diagnosed by examination under a microscope during colposcopy using the necessary samples in this case. During examination, the pathological focus looks like a white spot tightly attached to the mucosal epithelium with an uneven surface, which can be rough, folded, or covered with keratinized scales. When leukoplakia occurs, such a surface is formed from a keratin layer formed from a dense protein layer.
When the keratin layer is removed, a smooth pink surface can be found, from which the actual size of the pathological area is determined. Under a microscope, areas affected by leukoplakia are represented by growths of connective tissue into the epithelial layer in the form of papillae with tiny blood vessels located in them.
Classification of leukoplakia
That is, the upper layer of the epithelium hypertrophies (thickens), which corresponds to the processes of keratinization. Clinically, areas of leukoplakia appear as whitish or whitish plaques. The disease is not so rare, and is diagnosed in approximately every 20th woman.
According to some authors, the incidence of this disease reaches 5–12% in the structure of all cervical pathology. Among all women, leukoplakia is observed in approximately one in a hundred. It is believed that a third of patients with this disease may undergo malignant transformation. Therefore, it is so important to diagnose and treat this condition in a timely manner.
The process of development of leukoplakia consists of several stages passing one into another. It begins with the appearance of a small, mildly expressed inflammation on the mucous membrane. Subsequently, keratinization of the epithelium of the inflamed area occurs with the formation of a characteristic white focus of flat leukoplakia. Often the white color of the changed mucosa resembles plaque or film. However, an attempt to remove the “plaque” with a spatula fails.
Leukoplakia is a single or multiple whitish or white-gray lesions with clear contours. They can be of various shapes and sizes. As a rule, changes in the mucosa develop unnoticed, without causing any negative sensations. In this regard, the disease is often an accidental diagnostic finding when visiting a dentist. performing colposcopy. operations to circumcise the foreskin (circumcision), etc. Exceptions are leukoplakia of the mucous membrane of the scaphoid fossa of the urethra, which leads to difficulty urinating, and leukoplakia of the larynx, which causes coughing, hoarseness and discomfort when speaking.
The causes of this disease are numerous.
Since in such patients the cervix is often initially changed, treatment of leukoplakia causes difficulties. Treatment of cervical leukoplakia in combination with significant deformation is carried out surgically. Wedge-shaped or cone-shaped amputation of the neck or laser conization is used.
Diagnostics
All forms of leukoplakia do not have specific symptoms, so some symptoms are likely to apply to other female pathological conditions. That is why in such situations there is a need for additional examination. If the doctor still suspects leukoplakia, biopsy and colposcopy methods are used to confirm an accurate diagnosis. The results of such a study help determine the presence of cells of an atypical nature and prescribe the necessary procedures aimed at preventing malignant processes in the cervix. Sometimes, under areas with leukoplakia, changes are found in the cells of the more hidden basal layer; this pathology is also classified as a precancerous condition. If a hereditary form of leukoplakia is identified, treatment may be ineffective.
What happens
Depending on the clinical course, it is customary to distinguish the following types of leukoplakia.
- Plain or flat. One of the common forms. In this case, leukoplakia lesions look like ordinary white spots on the cervix and vagina. They are often noticeable even without colposcopy. Upon careful examination, it is noticeable that, in addition to color, the tissues are no different from adjacent ones - in elasticity, relief, the “plaque” is not easily removed when touched with an instrument (unlike, for example, candidiasis), but only with force, but with the appearance of bloody discharge in this place.
- Warty or verrucous. The resulting growths are similar to ordinary warts. They appear due to the fact that keratinized epithelial cells actively multiply, but do not slough off, but grow “like a horn.” At the same time, they are easily removed with a tool, leaving behind a mark on the neck in the form of a pinkish spot. It has to be distinguished from ordinary papillomatous growths.
- Ulcerative-necrotic. It is characterized by the fact that keratinizing cells are rejected over time to form ulcers. It is necessary to differentiate from ordinary erosions; often the diagnosis can be understood only with the help of a biopsy and subsequent tissue examination.
Based on the results of histology of the material, typical or atypical leukoplakia is established. In the latter cases, areas with abnormal cells are identified, which increases the risk of further malignant degeneration.
Changes in leukoplakia
Exposure to unfavorable factors can disrupt the metabolism in the cells of the cervix that exits into the vagina. This causes rapid keratinization of the surface of the squamous epithelium with thickening and the formation of a scaly layer. Leukoplakia can occur not only in the flat layer, but also in altered areas with single-layer columnar epithelium and even affect the deep basal layers. This close contact is justified not only by the common causes of occurrence, but also by the ability to move from one pathological state to another.
Treatment
An important question that arises for a doctor when diagnosing leukoplakia is what is the most effective treatment method to use in order to prevent the pathological disorder from degenerating into a malignant condition.
The main treatment methods for the occurrence of leukoplakia consist in the rapid elimination of the source of the disease and minimal injury to healthy tissue by the procedures performed. For this purpose, methods are used that allow choosing individual treatment with maximum effectiveness for each specific case of leukoplakia, for example:
1.Electrocoagulation (cauterization) is a widely used method for the treatment of leukoplakia . Due to its accessibility and being an inexpensive method of treatment, electrocoagulation is available to all segments of the population and has almost no contraindications. The equipment necessary for the procedure is available in every clinic. However, there are also disadvantages to using electrocoagulation:
- long-term healing of the injured area;
- painfulness of the procedure;
- damage to healthy tissue around the site of the disease;
- the occurrence of bleeding after rejection of the crust remaining at the cauterization site;
- the possibility of resumption of the disease after an area not completely covered by treatment;
- the appearance of a rough scar at the cauterization site, complicating the stretching of the cervix during subsequent births, therefore, electrocoagulation is not recommended for young nulliparous women.
2. Laser coagulation, a fairly effective method of cold exposure. It is painless and non-traumatic; the only disadvantages, as in the case of electrocoagulation, are the recurrence of leukoplakia, as well as some shortening of the neck after the procedure. Laser exposure is one of the best methods of treatment, as it is painless and antiseptic, does not injure organ tissue and does not cause bleeding. The surface film formed after the procedure on the surface of the organ protects against infection and prevents inflammation from developing. Healing occurs within a month.
Treatment of leukoplakia in women with a deviated cervix is often difficult, in such cases it is necessary to resort to surgical operations. For this, wedge-shaped or cone-shaped partial amputation of the affected area is used.
3. Radio wave surgery is a non-contact, gentle method that uses radio waves. The affected cells are evaporated using an electrode inserted into the vagina. Healthy tissue of the genital organs is practically not damaged, and areas of necrosis do not form.
All procedures for the treatment of leukoplakia can be carried out in laboratory conditions on the fifth day of the menstrual cycle. Simultaneously with the use of basic methods affecting leukoplakia, it is important to treat with therapeutic drugs, especially for ongoing infections of the genital organs.
Treatment and removal of leukoplakia
First of all, based on the research results obtained, they try to find the cause of leukoplakia. If it can be found, then treatment begins with treatment of the underlying disease.
The main methods of treating leukoplakia:
- Chemical coagulation . This method is based on the use of chemicals that act on the affected area. The drug used causes the death of pathologically altered cells. The most commonly used medicine is Solkovagin. Its effectiveness is noted in more than 95% of cases. No scar tissue forms on the mucous membrane after treatment and the mucous membrane completely restores its functions;
- Laser exposure . The affected area is cauterized with a laser beam. A crust forms, under which healthy cells form. The crust disappears after a few weeks. There are undeniable advantages when using a laser: it is painless, very effective and there are no relapses, it can be used for all patients. There are no scars after healing, healthy cells are not affected, recovery after the procedure is rapid;
- Surgical methods . These include loop excision and complete removal of the cervix. Excision involves using a special tool - a loop - to excise and remove problem areas of the affected tissue.
In cases where leukoplakia has greatly deformed the cervix and caused its destruction, the affected organ is removed completely.
- Radio wave surgery . For this manipulation, an electrode with radio waves is placed into the cervical canal. With their help, it is possible to eliminate the problem area. When exposed to radio waves, a high temperature is generated, which “melts” the area requiring removal. The use of this method does not harm healthy tissues, it can be used by young girls, there is no scarring or pain during the operation.
- Electrocoagulation . During this procedure, areas with leukoplakia are exposed to high-frequency current, i.e. cauterized. A crust forms to cover the wound, which will fall off over time. This method has contraindications: it cannot be used by nulliparous girls and pregnant women, it is not used in the presence of inflammation and cervical cancer, it cannot be used if a woman has problems with blood clotting.
- Cryodestruction . Its essence is the effect of low temperatures on the focus of leukoplakia using liquid nitrogen. In this case, frostbite of the cells occurs, the treated area is deprived of nutrition and dies over time. Dead cells come out in natural discharge over several months. The undeniable advantage of this method is the absence of scars, the absence of pain during the manipulation process, minimal impact on healthy cells, it can be used for nulliparous patients, and there are no complications.
- Conservative treatment . It may include the use of both general and local medications. Typically, medications are used for any disease concomitant with leukoplakia, or therapy is required for a simple form of the disease.
A wide range of antiviral, antibacterial and antimicrobial drugs are used. For example:
- Depanthol . This is an antimicrobial agent. They are used in the form of suppositories, supplementing therapy after cauterization of leukoplakia in various ways, for erosions, and so on. Candles are used twice a day for a week to ten days.
- Genferon . This is a broad-spectrum medicine. Boosts immunity, fights bacteria and viruses. The form of candles is also used. Prescribed for infectious diseases, inflammation, erosions, viral diseases. The usual duration of use is ten days, twice a day, simultaneously using two suppositories intravaginally. It is also possible to use this remedy for chronic diseases, using Genferon from one month to three.
- Panavir . It is an immunostimulant that also has an antiviral effect. Prescribed for detection of papilloma virus, cytomegalovirus, herpes infection and other diseases. This drug is used for intravenous administration. During the treatment period, 5 ampoules are used. Initially, three injections at intervals of two days, the last two with a break of three days.
Prevention
Patients at risk should especially carefully monitor the slightest changes in well-being and take preventive measures to prevent the development of leukoplakia. These include those who have menstrual irregularities, who have suffered from infectious diseases of the genital organs, who have had erosion or rupture of the cervix during previous births. Preventive measures include mandatory follow-up treatment of inflammatory processes in the reproductive organs, bringing hormonal levels close to normal, and constant monitoring by a gynecologist with colposcopy.
Important! Leukoplakia of the cervix is a dangerous disease only due to its possible degeneration into a malignant condition. Women whose atypical form of leukoplakia is accompanied by increased activity of cells located in the basal layer are likely to be at risk of developing cancer. In the case when the basal layer remains unaffected, the precancerous stage does not threaten.
Classification
The pathology can be simple or with cell atypia.
- Simple cervical leukoplakia is the formation of keratinized cells on the surface of the cervix, which form a plaque. Such cells are characterized by the accumulation of a dense protein - keratin, which, for example, forms the basis of nails, hair, and is also found in the upper layers of the skin. There are no microstructural changes.
- Leukoplakia with atypia is accompanied not only by the formation of a large number of keratinizing cells, but also by a change in their microscopic structure - an enlargement of the nucleus, the appearance of additional nucleoli, a high rate of division, disruption of shape, and so on.
Is leukoplakia cancer or not?
Doctors answer this question as follows: ordinary leukoplakia is only a background condition and does not transform into cancer. It belongs to the group of hyper- and parakeratoses, that is, keratinization disorders. Leukoplakia with atypia is a precancerous condition related to cervical intraneoplasia.
Depending on the prevalence of the disorders, leukoplakia is classified in the same way as cervical neoplasia. With grade 1, cell atypia is present only in the lower third of the epithelial layer, with the second it occupies 2/3, and with the third it covers the entire epithelial layer.
Leukoplakia of the cervical epithelium as a colposcopic sign, according to modern nomenclature, refers to abnormal data from a colposcopic examination.