There is a coating in the mouth in the morning
The appearance of white plaque on the mucous membranes of the mouth, tongue and inner lips in adults is one of the characteristic signs of thrush. This is a common fungal disease that has a tendency to become chronic. The fungus multiplies quickly in the mouth and is also contagious to other people.
If left untreated, candidiasis or thrush leads to severe discomfort, causing itching and burning. Complex therapy is required, which includes not only the use of antifungal drugs, but also increasing the body's defenses.
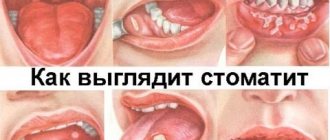
Reasons for the development of stomatitis in the palate
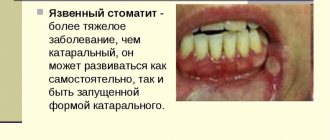
Stomatitis is a disease that affects the superficial and deep layers of the oral mucosa.
The pathology causes inflammatory processes, as a result of which the tissues affected by the disease can swell and swell, their surface becomes sensitive and hyperemic (with superficial lesions), and ulcers or aphthae with a white or yellowish coating often form on it (when the deep layers of the epithelium are affected).
Stomatitis occurs equally often in adults and children, but people with reduced immunity are most susceptible to this disease.
A separate group includes people for whom the likelihood of stomatitis will be higher:
- young children (due to an unformed immune system);
- pregnant women whose immunity is reduced so that the mother’s body does not perceive the fetus as a foreign organism;
- older people, whose immune systems may weaken with age;
- people with diseases that depress the body’s defense systems (HIV, oncology, etc.);
- people after a serious illness who have been treated with antibiotics or other drugs that reduce the body’s protective functions.
Often, an inadequate reaction of the immune system becomes the cause of unpleasant symptoms, and the weakening of the body’s protective functions creates a favorable environment for the influence of negative factors.
The exact etiology of this disease has not yet been clarified.
But the main factors that indirectly or directly contribute to its development have been identified:
- frequent mechanical trauma to the oral mucosa (for example, when wearing orthodontic appliances);
- the use of toothpastes containing sodium lauryl sulfate, which irritates the surface of the mucous membrane, provoking an inadequate immune response;
- stress and long-term emotional tension;
- an unbalanced diet, as a result of which the body may not receive all the substances it needs;
- avitaminosis;
- tendency to allergic reactions;
- changes in hormonal levels;
- gastrointestinal diseases;
- HIV;
- oncology.
Read also: Large toothbrush
There is a white coating in the mouth in the morning after sleep
Among the multiple diseases that occur in humans against the background of reduced immunity, a fungal pathology called candidiasis is widespread. Most often the affected area is the mucous membranes. This is due to the fact that single-celled microorganisms, being in an inactive state, are mainly localized in these places. Candidiasis of the oral mucosa makes itself felt when Candida fungi begin to actively multiply, which leads to the appearance of white plaque and an unpleasant odor from the mouth even after brushing the teeth.
Among the multiple diseases that occur in humans against the background of reduced immunity, a fungal pathology called candidiasis is widespread.
The location of plaque on the tongue is also an important diagnostic sign, as it may indicate pathology of a specific internal organ.
- if plaque appears in the central part of the tongue, then this may indicate stomach diseases;
- at the very base of the tongue - intestinal diseases;
- plaque on the tip of the tongue is associated with heart disease;
- the edges of the tongue indicate diseases of the liver and spleen;
- plaque on the back of the tongue may be a symptom of problems with the pancreas;
- a white coating on the palate may appear due to candidiasis;
- on the tongue and tonsils, near the throat - with sore throat.
How to deal with the problem?
Making a diagnosis when white rashes appear in the mouth involves, first of all, finding out the cause that provoked their formation.
In addition to a visual examination, the patient may be prescribed additional tests to identify viral infections or diseases of internal organs that can cause similar symptoms.
And if the root of the problem really lies much deeper, then it will not be possible to normalize the condition of the oral cavity without first dealing with the underlying disease. However, in parallel, treatment must be carried out at the local level, designed to relieve swelling and inflammation of the mucous membrane, as well as clean it of white plaque and spots.
In general, drug therapy in such cases is based on the use of a number of drugs:
To enhance the effect, you can additionally use decoctions and infusions of medicinal plants for rinsing, for example, chamomile, oak bark, calendula or eucalyptus.
If white spots are detected in the child’s mouth, gels and ointments are prescribed to relieve inflammation and pain, for example, Cholisal or Bonafton, as well as drugs to strengthen the immune system, most often based on interferon.
It is recommended for infants to wipe their gums, lips and inner surface of the cheeks with a decoction of chamomile or a soda solution using a cotton swab or a piece of gauze, and for older children to rinse their mouths with a decoction of string, sage or plantain.
Also, during treatment, changes should be made to the usual diet, excluding from it any food that irritates the mucous membrane, that is, spicy, salty and sour. Solid foods that can cause mechanical damage, thereby only aggravating the situation, as well as excessively hot or cold foods are also contraindicated.
Read also: What is the name of a braces doctor?
It is important to understand that without timely treatment, the consequences of white spots that appear in the mouth can be quite serious, because in their place ulcers and erosions most often form, making the damaged mucous membrane even more vulnerable to various types of infections.
And, of course, preventive measures that can reduce the risk of such a problem to a minimum are of great importance in this regard. We are talking about careful adherence to all rules of hygiene relating to the oral cavity (brushing teeth, using dental floss, mouth rinse, etc.), a balanced diet, thanks to which the body will be reliably protected from vitamin deficiency, strengthening the immune system and giving up bad habits, daily undermine human health.
popular about dentistry.
Join us and follow the news on social networks
Why is there a plaque in my mouth in the morning?
If the film appears exclusively after sleep, without disturbing later during the day, the cause may be respiratory diseases. With normal breathing through the nose, the oral mucosa does not dry out. Symptoms may indicate apnea, temporary interruptions in normal air flow, lack of fluid, and increased blood sugar levels. It is important to undergo a full examination.
According to statistics, women are more susceptible to candidiasis, but fungal infections also occur in the stronger sex. Symptoms may additionally be associated with bad habits - smoking, drinking alcohol. It is recommended to avoid the use of tobacco, alcoholic beverages, and fatty foods. You can rinse your mouth with a soda solution and drink still water during the day - at least two liters.
Symptoms of oral candidiasis
The symptoms of this disease are varied and can occur for various reasons. There are acute and chronic forms. The acute form is of two types: acute pseudomembranous candidiasis and acute atrophic candidiasis. The chronic form is: hyperplastic and atrophic.
These two chronic forms can occur independently or develop into one another. It is worth considering all these forms in more detail.
If this form of candidiasis occurs in adults, then it indicates that there are diseases such as hypovitaminosis, diabetes mellitus, malignant neoplasms, blood diseases and others. The lips, cheeks, back of the tongue, and palate are affected. The oral cavity becomes covered with a cheesy coating.
At first it is easily removed, but as the disease progresses, the plaque becomes denser and more difficult to remove, and the surface of the oral cavity becomes covered with erosion. It becomes very painful to chew.
Plaque in the mouth in the morning causes
Being in the mucous membrane, fungi of the genus Candida, multiplying, penetrate deep into the epithelium and secrete special enzymes that destroy the structure of cells in the human body. For this reason, white plaque on the palate of a child or adult has many unpleasant symptoms. The most common reasons that serve as an impetus for the activation of Candida:
- immunodeficiency;
- hormonal imbalances in women (pregnancy, menopause, etc.);
- diabetes;
- diseases of the gastrointestinal tract;
- deficiency of minerals and/or vitamins;
- long-term use of corticosteroids;
- disturbance of intestinal microflora;
- wearing dentures;
- microtrauma of the oral mucosa;
- use of oral contraceptives;
- consequences of radiation or chemotherapy;
- smoking, drug use, alcohol use.
If an adult observes a whitish coating only in the morning, and after oral hygiene it disappears, then we are most likely talking about incorrect teeth brushing, problems with salivation, poor circulation of the tongue, or various periodontal diseases. If the symptom is accompanied by severe dryness, this may indicate diseases of the digestive system, pancreatitis, ulcers, acute or chronic gastritis.
Symptoms of candidiasis
White plaque can appear on any part of the mouth. The rashes have a curd-like structure. As the disease develops, an adult begins to feel bad. Clinical signs of pathology depend on the individual characteristics of the organism, as well as on the nature of the course of the disease. Most patients complain of dry mouth, problems with swallowing, itching and burning sensations. Toxic substances released as a result of the activity of fungal bacteria worsen the general well-being of the patient.
Thrush in some cases is accompanied by an inflammatory process of the lip border. The degree of inflammation development is determined by the state of the immune system. The main clinical sign of thrush is the formation of a white coating in the mouth. With timely treatment, you can quickly get rid of unpleasant symptoms and pathogenic microorganisms.
In rare cases, white plaque on the palate is a clinical sign of a malignant formation. When analyzing blood cells, attention is paid to the values of tumor markers; if necessary, the patient is sent for consultation to a medical specialist - an oncologist.
Yellow coating in the mouth in the morning
A yellow tongue in a patient most often means the presence of diseases of the gastrointestinal tract. Moreover, these can be either serious disruptions in its operation or minor problems.
If the patient’s tongue is covered with a yellow coating, but it itself is not dense, but translucent, and it can be easily removed from the surface of the tongue, then this is most likely a symptom of the accumulation of toxins and wastes in the body. In this case, patients often complain that their tongue is yellow in the morning, but after carrying out hygienic procedures, the plaque can be removed. True, the next morning he appears again, and this repeats endlessly. The fact is that during the night our body digests the food received during the day. As a result, toxins are released and waste products are formed, which begin to be eliminated from the body in the morning. This is how morning plaque is formed. The more toxins and wastes accumulated in the patient’s body, the more intense the yellowing of the tongue.
If your tongue is covered with a yellow coating, which is easily removed and does not appear again within three hours, then you need to adjust your diet, and everything will return to normal by itself.
In a healthy person, it should be pale pink, slightly moist and in some cases with a slight bright pink tinge. Its sensitivity and functioning should be normal. The absence of an unpleasant odor and taste also indicates that the person is healthy.
If you have a dense dark yellow or yellow-gray coating with an unpleasant odor, then the problems are more serious. After all, the darker its color on the surface of the tongue and the higher its density, the more serious the disease. A yellow tongue and nausea should alert anyone; this is a serious reason to consult a gastroenterologist. Yellow plaque and bad breath are signs of stomach diseases. In more complex and advanced cases, patients complain of a yellow-brown tongue, as well as additional symptoms such as nausea and a bitter taste in the mouth.
A possible complication is invasive candidiasis, which is a lesion of the mucocutaneous tissue. Sometimes internal organs are involved in the pathological process.
Symptoms of invasive candidiasis:
- skin damage;
- dysphagia (swallowing disorder);
- feverish condition.
In the most severe cases, a shock reaction develops.
Causes of oral candidiasis
- Oral candidiasis occurs if a person suffers from serious illnesses or malignant neoplasms. This could be HIV, endocrinopathy, tuberculosis, carbohydrate metabolism disorders, stomach and intestinal diseases.
- Long-term use of glucocorticosteroid drugs and cytostatics, as a result of which the immune system is reduced, which contributes to the attack of Candida fungi >
It has been noted that diabetes mellitus can be asymptomatic, but thrush is its first sign.
There is plaque in the mouth in the morning, what to do?
If plaque in your mouth has become your constant companion in the morning, you should consult a doctor.
If a plaque is detected on the palate of an adult’s mouth, the doctor undertakes:
- Listen to the patient's complaints.
- Collect anamnesis.
- Inspect the mucous membrane and skin.
- Make a microscopy of a scraping from the oral cavity.
Additionally, the patient may be referred for consultation:
- to a dermatologist - in order to identify fungal infections of other systems and organs;
- endocrinologist - to detect endocrine pathologies;
- an allergist - in order to determine the body’s sensitization to the materials from which dentures are made.
After clarification of the diagnosis, treatment is prescribed.
Treatment and prevention
Dysfunction of the oral mucosa leads to complications in the structure of the entire body. Firstly, the presence of a focus of infection contributes to its spread to nearby organs and tissues: teeth, with the formation of caries, sinuses, conjunctiva of the eyes, membranes and substance of the brain. It would seem that an inconspicuous white film on the palate can lead to severe diseases, for example, meningitis and encephalitis with a high risk of death.
Read also: How to treat stomatitis in children with folk remedies
The first thing that needs to be done when a cloudy plaque appears is to establish the etiological factor. After an accurate diagnosis, treatment begins, targeting exactly the cause of the disease. And then the symptoms of the disease are eliminated.
Fungal plaque. For etiotropic treatment, antifungal drugs such as Fluconazole and Ketoconazole are used. The tablet form is purchased at the pharmacy and used for 2 weeks, 2 tablets each. In the presence of systemic manifestations on the skin, ointments are applied topically in the form of applications. Antifungal liniments - Clotrimazole and Nystatin. To relieve pain in the oral mucosa, lotions with Lidocaine or Articaine are used before eating.
Surgical treatment is not performed. After the prescribed treatment, the symptoms subside on the 5th day, and by the end of the second week not a trace remains of the plaque. To prevent the development of recurrent candidiasis, it is advisable for patients to be prescribed drugs that stimulate the activity of the immune system. These include: Anaferon, Kagocel, Interferon. The patient must take them for a month. You can resort to traditional medicine: tinctures of ginseng and eleutherococcus are natural immune activators.
After a course of antibiotics, in addition to drugs for the growth of bacteria in the intestines, antifungal agents should be prescribed.
When treating a sore throat, the choice of drug depends on the type of pathogen that caused the infection. For streptococcal or staphylococcal sore throat, antibiotics are prescribed. New synthetic broad-spectrum drugs are used in combination: cephalosporins, protected penicillins, glycopeptides. In case of viral etiology, it is advisable to prescribe antiviral drugs Anaferon, Arbidol, etc.
With angina, the process of swallowing becomes sharply painful, so the prescription of analgesic sprays, for example, Hexoral and Antiangin, is mandatory.
For the treatment of lichen planus, the drugs of choice are glucocorticosteroids - Prednisolone, Hydrocortisone. They are used in the form of a spray, the effect is local. To avoid side effects, the dose of steroids is gradually reduced and then completely discontinued. Local treatment consists of prescribing Anastezin for pain relief and drugs that enhance tissue regeneration. These include vitamin E and methyluracil.
A fairly common complication after taking steroid medications is a fungal infection; the above drugs are prescribed to prevent it.
Prevention
- Strict adherence to personal hygiene rules: use only a personal toothbrush and toothpaste, preferably for sensitive teeth. Once a day, thoroughly clean the dental spaces with dental floss. Use brushes to clean the palate and tongue.
- Fractional rational nutrition - a variety of foods, with an increased amount of food intake. Washing vegetables and fruits before eating.
- Prevent the development of vitamin deficiency by taking complex medications in the autumn-winter period.
- Timely treatment of dental caries and chronic infections in the body to avoid decreased immunity.
In some cases, white spots are interpreted as markers of precancerous diseases. For verification, it is necessary to monitor laboratory parameters of tumor markers in the blood. Next, a consultation with an oncologist is scheduled.
Additionally
The etiology of leukoplakia has not been precisely established, but in most cases the cause of the development of keratinized areas is mechanical damage. In the mouth, this is possible when the edges of teeth and dentures are not polished enough. Before treatment, the patient is sent for a consultation with a dentist, which most often promotes spontaneous healing of the oral mucosa. But in severe cases, the intervention of conservative medicine is required, in the form of taking vitamins a, b, c, d. The Asepta company has released special vitamin complexes for the oral cavity that cope well with the symptoms of leukoplakia and prevent its further development. In extreme situations, when the condition threatens the patient’s life, laser excision of the affected areas is performed.
Syphilis is treated by a dermatovenerologist; therapy is long-term and sometimes lasts up to several months. The patient is registered at the dispensary, and even after clinical recovery undergoes several diagnostic courses. Specific treatment is carried out with penicillin preparations - benzylpenicillin is administered 2 times a week for 2 months, then laboratory monitoring of the activity of Treponema pallidum is carried out, and the dose is reduced.
The patient is under clinical care for 3 years after infection. Every 3 months a control blood test is carried out, and the decision to deregister is made individually.
Antiparasitic drugs are used to eradicate worms and Giardia. These are Pirantel, Nemazol, Zentel.
Chronic diseases should be in remission, or better yet, in the phase of clinical recovery. If the patient is registered with, for example, an endocrinologist or gastroenterologist, it is imperative to explain the effect of the disease on the immune system. If a white coating forms during gastritis, then first of all it is necessary to treat inflammation of the gastric mucosa.
All adults with plaque detected on the mucous membrane of the hard palate are prescribed antiseptic solutions for mouth rinsing, such as Miramistin, Chlorhexidine, Stomatidine. You should rinse your mouth after each meal to reduce the risk of complications.
Plaque in the mouth in the morning, treatment at home
Treatment involves the use of topical drugs and internal medication.
To treat the oral cavity in adults, with very high sensitivity of the mucous membrane, it is allowed to use a diluted Lugol's solution (2 tsp per 200 ml of warm water from a kettle).
You can also lubricate the oral cavity with baking soda diluted in water (1/2 tsp per 150 ml of warm boiled water). The procedure should be carried out 2-3 times a day.
Drug therapy involves the use of antifungal and painkillers. Antihistamines are additionally used as prescribed by an allergist.
Types of fungal disease
To infect the body and oral cavity with a fungus, exposure to provoking factors is required. In medical practice, oral candidiasis has 3 variations in the course of the disease.
Pathology develops in children or the elderly against the background of a weakened immune system. In adults, the fungal compound Candida is caused by colds and chronic pathologies. If the immune system is unable to resist the pathogen, Candida fungus appears in the oral cavity.
Thrush of the oropharyngeal type
Develops from the use of antibacterial drugs. If the dosage of the drug is violated, the microflora of the oral cavity increases the risk of penetration and activation of infectious diseases of the mouth. Aggressive therapeutic techniques increase the likelihood of developing thrush.
At the initial stages of development, the disease is difficult to diagnose. There are no obvious clinical signs of pathology. The plaque does not exceed 3 millimeters in size.
Mycosis
Mainly develops in newborns. Young mothers confuse the clinical sign of developing pathology with the remains of curdled milk in the gum area. The occurrence of the disease is explained by infection of the mother’s body during pregnancy or infection during childbirth.
Treatment with popular folk remedies
Folk remedies help get rid of white mouth sores faster, and they are also widely available.
- Dilute 1 teaspoon of baking soda in a glass of warm water and rinse your mouth.
- Add a teaspoon of calendula tincture to half a glass of water; you can apply this solution to the affected area.
- Squeeze carrot juice and dilute it 1:1 with water, rinse your mouth.
- Grind 1 clove of garlic, mix with sour cream (1 tsp), apply to the aftertaste.
- Chop raw potatoes and make a lotion on the sores.
- Grind the burdock seeds, add a little salt to the resulting juice, evaporate over heat, adding a little butter to make an ointment. Use this ointment to lubricate all aphthae that appear in the oral cavity.
Traditional medicine is not the ultimate truth; all the remedies described should only accompany the main treatment, and not be independent remedies for aphthae. Before using them, it is important to consult a doctor.
Attention! What is a periodontal tooth: symptoms, photos, treatment methods. Find out everything about this dangerous disease.
Do you feel pain in your tongue, as if it is burned? Then this is the place for you. Our experts are eager to help you.
A selection of cheap analogues of Cholisal gel is presented in the next article. Take note!
Clinical manifestations of diseases
Knowing the reasons for the appearance of white plaque on the sky is not the most important thing. It is also necessary to know the symptoms of diseases that provoke its formation. This will allow a specialist to accurately characterize your condition so that he can make a diagnosis. Also, the accompanying symptoms can suggest how dangerous the disease is.
Diseases in which plaque forms on the mucous membranes can manifest themselves in different ways.
Therefore, it is worth considering the features of each:
- Candidiasis. In addition to plaque, it is characterized by such symptoms as the formation of cracks in the corners of the mouth, a feeling of dry mucous membranes, burning and a bitter taste.
- Angina. If it is present, symptoms of intoxication appear. They include headache, high fever, drowsiness, chills, etc.
- Leukoplakia. Its main feature is the distortion of taste perception. It is caused by changes in the structure of the mucous membranes.
- Lichen planus. This pathology is often accompanied by severe pain while eating. Contact with food leads to rupture of the blisters, which causes pain.
- Worm infestation. This disease is associated with disturbances in the gastrointestinal tract. The patient may experience stomach upset, constipation, nausea and other unpleasant symptoms.
- Giardiasis. Damage to the body by Giardia often manifests itself as intoxication. This may be nausea, headache, fever. Jaundice also often develops.
- Syphilis. Its presence is quite difficult to detect, since it may not manifest itself with any negative signs. It may be indirectly indicated by the fact that the patient is prone to promiscuity.
All detected signs should be described to the doctor so that he can assess the condition and prescribe appropriate treatment.
Video from Dr. Malysheva: