What does it mean to “catch a tooth”: expert opinion
It is impossible to freeze the tooth itself, that is, its components such as enamel, dentin and pulp. Therefore, this phrase is absolutely incorrect and is never used in official medicine. But this concept is often used in everyday life, for example, when teeth hurt after a person was hypothermic or was blown away. Some people say this when they have pain due to acute respiratory viral infections, acute respiratory infections, influenza and other non-dental pathologies, although this is again wrong.
Important! Are you feeling cold? It is not surprising that against this background your teeth ache. However, an alarming sign may also indicate the presence and exacerbation of various diseases of a dental and non-dental nature.
Sometimes they also say “the nerve of the tooth caught a cold” or the phrase “the nerve was blown” is used. This usually means inflammation of the neurovascular bundle of fibers (pulp), securely hidden by enamel and dentin. But in this case, the cause of the pathology is not colds and hypothermia; rather, they act as catalysts leading to an exacerbation of the inflammatory process already existing in the tissues in the initial or chronic stage. In official medicine, the disease is called pulpitis.
The dental nerve is chilled: treatment, causes, prevention and symptoms of a chilled nerve
Often, after being in the cold for a long time, a person may develop a toothache. Why does this happen, and how can cold cause pain? The fact is that the dental nerve can get cold.
However, healthy teeth do not react to cold or temperature changes. If a tooth begins to ache in the cold, this indicates the presence of a pathological process inside it. This situation requires treatment.
Let's look at what to do if the tooth nerve is cold and how to recognize the disease.
Where is the dental nerve located?
To understand where the nerve is located, you need to know the structure of the tooth. Its top layer consists of enamel, the next layer is the dentin shell, which is hidden under the enamel.
Attention! In the central part of the tooth there is soft tissue - pulp. It is dotted with many nerves and vessels. Larger nerves are connected to the root processes (as many roots as there are nerves). Small nerves together with blood vessels are collected into a neurovascular bundle.
Any pain in the dental nerve is associated with the development of a pathological process inside the tooth, and therefore requires medical intervention. And the stronger the pain, the sooner you need to seek help from a dentist.
Nerves, as well as lymphatic and blood vessels, are part of the fibrous substance that fills the entire cavity in the tooth, represented by soft tissue. After their removal, the tooth ceases to be alive.
Signs of hypothermia of the dental nerve
If a person has a cold on the dental nerve, this can be recognized by the following symptoms:
- aching pain is felt in the jaw area;
- the pain may be shooting in nature;
- increased sensitivity of the eyes, eyelids, forehead;
- When eating cold food or drinks, the pain intensifies;
- smiling can also be accompanied by pain.
Important! The cause of the pathological process affecting the dental nerve is pathogenic bacteria that penetrate the pulp.
Changes in temperature or slight physical impact cause throbbing or shooting pains.
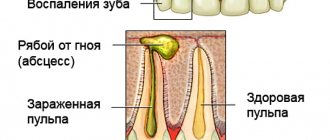
If the pathological process spreads beyond the dental nerve, periostotitis (flux) or periodontitis may develop. The presence of pus and swelling distinguishes periodontitis from pulpitis.
Both women and men are equally susceptible to hypothermia of the dental nerve. Every person, regardless of age, can get a cold in their teeth. What to do if this happens? You should immediately seek help from a dentist. If this is neglected, various complications are possible. The inflammatory process will spread to nearby tissues, causing suppuration. As a result, the dental nerve may simply die. Over time, the tooth will stop hurting, but this does not mean that the problem is eliminated. Inflammation will remain, in addition, it will capture more and more new tissues, spreading the infection. That is why it is so important to eliminate the source of inflammation in time.
Periostitis in common parlance – gumboil – is the rapid spread of pus in the gum tissue. A dangerous disease, the consequences of which can be replenishment of teeth, gums, and the whole body.
Why does the disease occur?
There are several reasons that can cause the disease:
- untreated deep caries, turning into pulpitis;
- injuries, chips, broken teeth;
- poor-quality treatment that caused a secondary infection;
- treatment and filling of teeth with low-quality materials or medications;
- poor-quality tooth treatment during prosthetics;
- penetration of infection into the tooth caused by other diseases.
Deep caries is the last stage of the carious process, it is expressed in the destruction of the tooth crown, the spread of infection in the soft tissues of the tooth, pain when exposed to temperature, mechanical or chemical stimuli.
Home treatments
In case of hypothermia of the dental nerve, you should consult a dentist. He will select adequate treatment and eliminate the problem.
If the patient does not have the opportunity to immediately visit a doctor, you can use traditional medicine.
However, it should be remembered that such treatment will not eliminate the cause of the disease, but will only relieve its symptoms, helping to alleviate the patient’s condition. Therefore, even if the tooth stops hurting, you will still have to visit a doctor.
- Moisten a small piece of cotton wool with alcohol or vodka, then place it in the tooth cavity. It is necessary to ensure that the cotton wool is in the tooth and does not come into contact with the mucous membrane of the oral cavity, otherwise it can burn it.
- Dilute in 1 tbsp. warm water 5 drops of chlorhexidine. Use the resulting solution to rinse.
- The following remedy must be prepared in advance. To prepare it you will need 25 g of birch buds and 100 g of alcohol. Mix the ingredients and leave for 1.5 weeks. Dip a piece of cotton wool into the prepared tincture and apply it to the painful tooth until the pain goes away.
- 1 tbsp. Brew a spoonful of chicory with 1 cup of boiling water. Let it sit for several hours and use as a mouth rinse.
- Brew a couple of tablespoons of sage with boiling water and let the broth stand until it cools completely. Use to rinse your mouth every half hour. Sage has antiseptic, analgesic and disinfectant properties.
- Pour boiling water over 5 teaspoons of chopped willow bark. Cool and then use for rinsing, diluting with warm water. Willow can also soothe pain and relieve inflammation.
- Dilute 2 teaspoons of hydrogen peroxide in half a glass of warm water and rinse your mouth with the resulting solution. Hydrogen peroxide not only soothes pain, but also cleanses plaque from teeth.
- Dilute 1 teaspoon of baking soda in a glass of warm water. Rinse your mouth up to five times a day.
- Clove oil is a good natural pain reliever and disinfectant.
Place a few drops of oil on cotton wool and place into the carious cavity. If the tooth is not damaged, then apply it to the gum. Birch buds, willow bark, sage, hydrogen peroxide, clove oil, chlorhexidine, cat's paw, sorrel, salted lard are some of the remedies used in folk medicine to help relieve pain when the dental nerve gets cold. - You can soothe toothache with fresh or salted lard. It is necessary to cut a small slice and apply it to the gum of the diseased tooth. After about 20 minutes, the pain should subside.
- To quickly relieve pain, you can use garlic. Apply half a clove to the gum and hold until the pain disappears. If held for too long, a burn to the mucous membrane is possible.
- If the pain is not too severe, you can try to get rid of it by chewing fresh sorrel greens.
- Another interesting remedy can be prepared from the cat's paw plant. Grind a little dried plant, wrap it in a piece of tissue paper and roll it into a roll. Light it and smoke, drawing smoke into your mouth, but not into your lungs. After some time, the pain will subside.
Disease prevention
Very often, the cause of hypothermia of the dental nerve is untreated caries. This is due to the fact that any impact on the nerve, including cold, can only cause harm if the tooth is already damaged.
Attention! Healthy teeth do not react to temperature changes. To prevent tooth hypothermia, it is necessary to treat caries in a timely manner, as well as undergo preventive examinations, even if nothing hurts. Maintaining oral hygiene is of great importance in the prevention of dental diseases.
It is very easy to chill the tooth nerve in cold or windy weather. To protect yourself from this, you need to choose the right clothes for the cold season. A hat, scarf, and high collar will help protect your teeth and other organs from hypothermia.
Source: https://ZubNeBoley.ru/lechenie/lechenie-zastuzhennogo-zubnogo-nerva/
The main reasons associated with the unpleasant phenomenon
What happens to a person when he gets hypothermia, gets a strong wind, or catches an infectious or viral disease accompanied by inflammation of the ear-nose-throat area? His body temperature rises, a cough and runny nose appears, and all surrounding tissues swell. Against this background, pain arises, which most often covers the entire head, often radiating to the jaw and teeth - this is one of the main reasons why there is a feeling as if the teeth were blown. But there are other factors that lead to this phenomenon. Let's consider them further.
Exacerbation of existing dental pathologies
With hypothermia, as well as any diseases of the body, the immune system sharply decreases, which means that pathologies that already existed before but were not treated become aggravated and progress. For example, caries, chronic pulpitis and periodontitis. Against the background of decreased immunity, untreated caries can very quickly become complicated by pulpitis and periodontitis[1].
On a note! This unpleasant phenomenon is typical for people with weakened immune systems: children, the elderly, women during pregnancy and breastfeeding.
During this period, a cyst or granuloma may make itself known, which gradually grew and remained undetected for a long time. And periodontitis often leads to the appearance of a lump on the gum, filled with pus and periodically breaking out through the fistulous tract. Also, some people, just after they have been blown by a strong wind or in a draft, discover that they have flux and all the accompanying symptoms: their cheek and face swell, their body temperature rises, and, naturally, their teeth hurt badly.
“In our office the air conditioner is always on, which once gave me a very serious blow. Against this background, my jaw began to ache. Later I noticed that the teeth under the fillings also hurt. When I recovered, it still continued to hurt under one filling. I had to go to the dentist... At the appointment they said that there was periodontitis, which developed due to poor-quality treatment of caries and incomplete filling of the canals. This was an unpleasant surprise! As the doctor said, under the influence of a cold, the sore, which had not manifested itself in any way before, became aggravated and worsened..."
Tanika, review from the dental portal gidpozubam.ru
Features of the treatment of viral and infectious diseases
Both in case of normal hypothermia, and ARVI, influenza, sore throat, herpes virus and other pathologies of a similar nature, the patient is prescribed to drink plenty of fluids in order to quickly remove toxins from the body, support the immune system and avoid dehydration. The following drinks are often consumed for this purpose: rosehip decoction, tea with lemon, fruit drinks and compotes with berries - they all contain large amounts of vitamin C, which has a destructive and irritating effect on the enamel.
Consequence: the enamel becomes hypersensitive, reacts to the temperature of food and any mechanical stress. Due to the abuse of such drinks, erosions appear on hard tissues, and their resistance to cariogenic bacteria drops sharply.
To avoid this problem, doctors advise thoroughly rinsing your mouth with plain water after drinking acidic drinks.
Poor oral hygiene
After hypothermia and infectious viral diseases, many feel severe weakness and malaise, and therefore stop performing thorough daily oral hygiene. Some people completely forget about the brush and toothpaste, which is why plaque quickly accumulates in the mouth, which is the best breeding ground for bacteria that cause caries and other dental diseases.
On a note! After you have recovered, it would be a good idea to purchase a new brush, since the old one may retain pathogenic bacteria that can provoke an inflammatory process in the oral cavity.
ENT diseases
With otitis media, tonsillitis, sinusitis and sinusitis, strange symptoms sometimes occur, for example, the ear and teeth may hurt at the same time. This is again due to the fact that in a sick person, not only the organs where the pathology occurs swell and become inflamed, but also all adjacent areas. In this case, the pain often does not have a clear localization, radiating to the head, jaw, and eyes.
When ENT diseases are neglected or treatment tactics are incorrect, bacteria spread from the affected tissues to healthy ones, penetrate with blood and lymph into the oral cavity, provoke the development of the same caries, inflame the nerve of the tooth (pulpitis occurs) and periodontal tissue.
On a note! The opposite situation also happens: diseased teeth contribute to the development of ENT pathologies. For example, units of the upper jaw affected by deep caries, pulpitis, periodontitis and cysts can lead to the development of odontogenic sinusitis.
Inflammation of the facial nerve
This nerve has branches that cover all areas of the face. Therefore, when it becomes inflamed, the jaw and teeth may become sore. Often the pain has no clear localization. Pathology, again, can occur against the background of hypothermia, impaired blood circulation in the tissues, as well as various dental and non-dental diseases.
Teeth hurt when you have a cold - reasons
So is it possible to catch a cold in your teeth? Although the symptoms of this condition are familiar to many, a detailed consideration of this issue forces the answer to this question in the negative.
Usually, discomfort in the teeth is associated with side effects of treatment and some features of the course of ARVI.
Thus, a person who has a “cold” tooth may actually suffer from the consequences of ARVI treatment. In this case, simple oral care, treatment of the underlying disease (sinusitis, otitis media, ARVI) and drinking plenty of clean water will help.
Another common misconception is “cold” gums. A person who has a “cold” in the gums is actually experiencing symptoms of an exacerbation of the infectious process in the gums under the influence of hypothermia, a viral infection, etc. Aching pain in the gums may indicate the presence of a granuloma - a capsule with pus, which is located at the root of the tooth deep in the gums. Its symptoms:
- aching, bursting pain in the gums;
- swelling of the oral mucosa;
- the pain appeared after hypothermia, an acute respiratory viral infection or another infectious disease.
Granuloma occurs near teeth with caries, as well as in those who suffer from bleeding or inflammation of the gums. Thus, you can prevent its development by regularly visiting the dentist.
What to do if you have a “cold” in your gums, causing an exacerbation of granuloma? There is only one answer - urgently visit the dentist. It is important to understand that the source of infection is deep in the tissues, and applying compresses, lubricating with ointments, etc. will not be able to destroy it.
Signs of nerve inflammation
As mentioned above, often the phrase “the tooth (nerve) caught a cold” is associated precisely with the exacerbation of the inflammatory process in the pulp, which made itself felt after hypothermia of the body and a sharp decrease in immunity against the background of various diseases. In this case, the following symptoms will indicate that the teeth have blown out:
- severe pain that intensifies and does not go away for a long time after eating hot and cold food, being in the cold, at night. Pain sensations spread throughout the jaw and are not always relieved with tablets from a home medicine cabinet,
- hyperemia (swelling and redness) of the gums in the area of the affected unit,
- there may be chips, deep carious cavities and cracks on the diseased element,
- The more advanced the process, the higher the likelihood of an increase in body temperature and the appearance of general malaise.
“The other day I blew out the nerve of a tooth. The pain was unbearable, the pills didn’t help, so I simply couldn’t stand it for more than two days. I went to the doctor. I don’t remember how some people manage to walk with pulpitis for several months and even years. This is just torture! Modern treatment methods make it possible to cure everything in no time, rather than endure this nightmare!”
Stanislav, review from 32top.ru
The nerve does not tolerate excessive external influence
With the negative impact of external factors on the dental nerve and with a cold in the tooth, a number of complications are possible, for example, inflammation of the nerve may occur.
The disease occurs when pathogenic microorganisms penetrate the pulp. It is they who cause inflammatory processes, accompanied by severe pulse-like pain, which increases with mechanical or thermal effects on the affected area.
Often pulpitis spreads beyond the tooth root. Then inflammation of the tissues surrounding the tooth occurs.
In addition, a cold nerve can affect the occurrence.
Accompanied by:
- acute pain;
- swelling of the cheeks, lower eyelid, lips;
- deterioration of health;
- redness of the gums.
It is better to entrust the treatment of this problem to a dentist to avoid serious consequences. Self-medication in this case is not always effective.
If the third molar hurts
Very often, after a wind blows, or after hypothermia, a wisdom tooth begins to ache. This may be due to all of the reasons listed earlier. But sometimes this signals an exacerbation of pathologies that are characteristic directly of the third molar:
- eruption is too long, complex and not always correct: “eights” pass through the bone and touch the nerve endings, sometimes they rest against neighboring elements of the row, put pressure on them and destroy them, provoking vague pain sensations,
- pericoronitis: acute and often purulent inflammation of the gingival hood hanging over the “sage”, under which food debris and bacteria become clogged.
Complications during the eruption process
Most often, the eruption of a wisdom tooth occurs either incorrectly or with partial problems, this is called “retention.” The patient experiences discomfort in any case, and if the painful sensations bring him unbearable suffering, the doctor eliminates the problem by removing the problematic tooth. What complications can occur if teething is very difficult and if you neglect to visit the dentist?
- Since the “eight” is covered on top by a fabric “hood,” inflammation of this area of the gum often occurs, which can result in osteomyelitis and periostitis.
- The wisdom tooth grows for a long time and in a hard-to-reach place, where it is very difficult to clean. Therefore, it is gradually affected by caries, and often completely destroyed by it.
- If the problem is neglected, the painful eruption of the figure eight can cause neuralgia, as well as severe pain in the head, throat, ear, neck and even chest.
To avoid undesirable consequences (even if the eruption of wisdom teeth does not cause discomfort), it is better to consult a doctor just in case. Under the supervision of a specialist, this process will proceed with the least amount of problems.
What you can and cannot do at home
If you think that your tooth has blown out, and even more so, you have discovered the symptoms described earlier, then you need to consult a doctor who will determine the true cause of the problem and provide treatment appropriate to the situation. But not everyone is in a hurry to see a dentist. Some people prefer to wait until their signs of hypothermia and various non-dental diseases have passed. What is appropriate and what absolutely cannot be done during this period? The answer is in the table below.
| Can | It is forbidden |
|
|
If you have a cold or a toothache, what should you do at home? You can only fight symptomatic manifestations (pain, fever), strengthen the immune system in every possible way, and also treat the underlying disease that caused the unpleasant symptom. But if the causes of the pathology are dental problems, and this is precisely the case in most cases, then stopping the symptoms will not help to correct the situation for a long time. In this case, the only right decision is a visit to the dentist.
Treatment of granuloma
If the patient has a cold in his teeth, causing the development of a granuloma, it must be treated as soon as possible.
In the early stages of the disease, granuloma can be treated therapeutically, but in more advanced cases, surgical intervention cannot be avoided.
Therapeutic treatment includes antibiotics. This approach allows you to relieve inflammation only in the early stages of the disease, when the granuloma is small in size and the surrounding tissues are not inflamed.
If a purulent sac has already formed in the gum, the dental surgeon must cut it and drain the pus out. The procedure is performed under local anesthesia. After this, the patient should rinse the mouth for some time with an antiseptic solution, for example, a decoction of herbs. A course of antibiotic therapy may also be prescribed.
If a granuloma forms on the same tooth repeatedly, the doctor cleans and fills the tooth canals with a filling to prevent re-infection.
What treatment options can your dentist offer?
Let's consider what the doctor will do if it turns out that hypothermia, viral and infectious diseases have become catalysts for dental problems.
For caries, pulpitis, periodontitis
As a rule, in this case, the patient requires a competent endodontist dentist who will qualitatively clean, treat and seal the root canals of the diseased unit. If necessary, the specialist will also remove the pulp.
Depending on the severity of the pathology, treatment may require 1-3 or more visits to the clinic. So, during the conservative treatment of pulpitis (preserving the pulp) and periodontitis, the doctor will put medications and antibiotics into the canals, cover them with a temporary filling, and repeatedly take x-rays. Only after the source of infection has been completely eliminated will you be given a permanent filling. If a row element has been severely undermined by disease and destroyed, it may need to be strengthened with a pin and inlay, as well as an artificial crown.
Important! Today, better treatment of pulpitis, periodontitis, as well as cysts and other formations is facilitated by the use of modern optical technology, for example, a microscope. Using this device, the specialist sees all the branches of the root canals, completely removes the infection, hermetically seals and carries out highly aesthetic restorations.
For purulent formations
If it turns out that the pain is caused by flux, fistula, cyst, granuloma and abscess, then doctors will dissect the tissue and ensure the outflow of purulent contents using drainage, then apply sutures. During the rehabilitation period, the patient will be prescribed antibiotics, rinses, symptomatic treatment (painkillers, anti-inflammatory, wound healing), and physiotherapy.
For increased sensitivity
Strengthening procedures - remineralization and fluoridation - will help get rid of the consequences of consuming acidic drinks during the treatment of various diseases and eliminate the sensitivity of hard tissues. At home, it is recommended to consume more products with calcium, as well as purchase remineralizing pastes with fluoride, calcium hydroxyapatite, and beneficial natural ingredients (chamomile, propolis).
On a note! If there is increased sensitivity on units with crowns and fillings, then it is important to check the quality of adherence of the structures to the hard tissues and walls of the tooth. It is necessary to make sure that there are no cracks or chips, that the seal is not broken, and that the service life of artificial restorations has not come to an end, otherwise they must be replaced with new ones. It is also important to understand whether an inflammatory process has developed under the filling and crown, because then the product will have to be removed and the root canals treated using endodontics.