What to do if a tooth hurts after nerve removal and canal cleaning
Treatment of tooth canals is a high-tech manipulation that requires the dentist not only to have relevant theoretical knowledge, but also to have developed skills in the use of special methods and means specific to endodontic therapy.
Simply put, this procedure is complex and involves many possible medical errors. Unfortunately, there are often situations when, after removing the nerve (pulp) and cleaning the canals, the tooth continues to hurt. Sometimes the pain is so severe and persistent for a long time that a person is forced to take painkillers for several days.
And here it is necessary to understand why a “dead” tooth can hurt in general - after all, after cleaning the canals, it would seem that there are no more nerves in it. And how long can this last, is it worth waiting a little at home or should you immediately run to the doctor for an appointment.
Generally speaking, dentists call all pain that occurs after treatment and proper filling of canals “post-filling pain.” Moreover, some doctors believe that such pain is a 100% complication, even if the x-ray shows that the canals are sealed without errors. Other dentists are of the opinion that tooth pain after nerve removal, cleaning and high-quality canal filling is a condition within normal limits, but only if the pain persists for no more than 5-7 days.
Post-filling pain after cleaning the canals can be either constant or occur only when biting or pressing on the tooth, which makes eating very difficult. Most often, pain occurs spontaneously a few hours after the treatment procedure and is constant.
It is acceptable to maintain minor painful sensations for up to 2-3 weeks, if their intensity is characterized by a gradual decrease every week. But a sharp increase in pain a few days after treatment requires urgent diagnosis and, possibly, re-treatment and cleaning of the canals.
But what should a person do if the tooth continues to hurt for a long time and persistently after removing the nerve and treating the canals? Well, in such a situation, you urgently need to make a second appointment with a doctor to assess the advisability of re-treatment.
Firstly, in such cases, pain is often an indicator of complications in the tooth that arose due to errors made by the doctor during treatment. Secondly, you should know the “enemy” (complication) in person in order to be able to correct the situation in time and save the tooth from removal. Inactivity is unacceptable here.
So, let's figure out in order why exactly after removing the nerve and cleaning the canals, the tooth may continue to hurt...
The filling material is brought out beyond the apex of the tooth root
Among all the complications that arise after cleaning and filling canals, the removal of filling material beyond the root occupies, perhaps, one of the first places, even despite the systems available in dentistry for monitoring the accuracy of this procedure. Almost every dentist with more than 10 years of experience has encountered situations at least a hundred times when, after removing the nerve and removing the filling material beyond the apex of the root, the patient’s tooth began to hurt severely on the day of treatment.
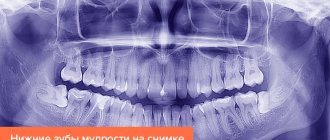
Diagnosing such a complication is possible only after studying an x-ray or visiograph data on a computer. But panoramic radiography of both jaws does not always allow us to examine in detail the apexes of the roots of the treated teeth and identify the problem.
When the filling material is removed beyond the root, the tooth may hurt for a very long time - up to 5-6 months. It all depends on how much material has been released into the surrounding soft tissue, what kind of material it is, and also what level of reactivity of the body the person has (after all, filling material is a foreign body to which an immune response occurs, the severity of which will be different for different people) .
In 1935, dentist A.A. Anishchenko proposed a method of filling tooth canals with phosphate cement, and he expressed the opinion that the best way to restore the destroyed bone around the root during periodontitis is to move the material beyond the root into this pathological focus. Modern dentists consider this method of treatment to be a mockery of the patient, since even if positive results are achieved due to strong sealing of the canal inside and outside it with a cement plug in which bacteria cannot multiply, nevertheless, immediately after the end of the anesthesia, the person will begin to experience hellish pain. They may be even stronger than before dental treatment.
The phosphoric acid solution contained in phosphate cement has a strong irritating effect, and the hardening cement mass itself is a foreign conglomerate that will never “resolve” when located outside the root. For unknown reasons, under the conditions of terrible Soviet dentistry, this method was used for more than 30 years!
Currently, cements are extremely rarely used for root canal treatment, and removal of any filling material beyond the root apex is considered a complication. Thanks to the leap in scientific progress, dentists began to use gutta-percha pins and the Termafil system for obturation (filling) of canals and their branches.
If the working length of the tooth is incorrectly determined, there is no apical stop, or the gutta-percha pin is not adjusted to the correct size, material is removed into the tissue surrounding the root. In this case, on the x-ray you can see how a white strip of filling material passes inside the root, reaches its apex and continues further. Even a person who is not entirely advanced in matters of dentistry can easily diagnose a doctor’s mistake when the gutta-percha pin extends beyond the root by 4-5 millimeters or even more.
Physiotherapeutic methods for relieving tooth pain after nerve removal and canal cleaning are sometimes used phonophoresis with hydrocortisone, helium-neon laser, fluctuating currents, microwave and UHF. These methods are suitable both for “classic” post-filling pain and as an additional therapy for pain after eliminating the consequences of various complications.
Improperly sealed canal
If, when the filling material is removed beyond the apex of the root, the tooth begins to hurt within a short time, then if the canal or canals are insufficiently filled, it may not react at all. As a rule, when the tooth does not hurt in such a situation, the effect of imaginary well-being is created. And the question here is how long he can stay sick after such poor treatment.
In my dental practice, I have repeatedly encountered the retreatment of teeth, which sometimes were not sealed inside the canals at all, or the filling material was simply “smeared” along their walls for a period of limitation from 5-6 months to 7-8 years or more. If the patient himself came for help, the complaints were something like this:
“So many months (years) ago I treated (treated) a tooth, and it, being dead, did not hurt (or hardly bothered me) until the other day when severe spontaneous pain arose, especially when pressing on the treated tooth while chewing hard food..."
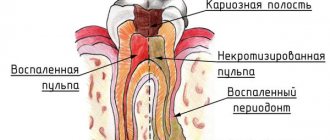
In many such clinical cases, due to the proliferation of bacteria in empty or half-empty canals, certain changes occurred in the bone tissue near the apex of the problematic root: from a slight loss of bone tissue to the formation of a granuloma or even a cyst.
The sooner the root filling is removed and the tooth is re-treated, the faster the pain will go away (if any), and conditions will not arise for the growth and multiplication of infection in the canals with a transition to the peri-root area.
Tool breakage in the channel
If a dentist encounters such a complication for the first time as an instrument breaking off in a canal, then in most cases the doctor panics (a psychological factor is triggered - after all, this is a medical error). However, this, although not the most common, but nevertheless quite common operational error, can be corrected using modern technologies and methods, and the tooth can be saved.
If, while cleaning the canal, part of the endodontic instrument breaks in it, then if it is left in the canal, the tooth will begin to hurt either immediately or after some time. This is due to the fact that a piece of an instrument stuck in the canal does not give the doctor access to the apex of the root, which is why a part of the nerve remains there or an infection that has not been washed out, which will certainly begin to multiply and can lead to very big problems in the future.
Extension of filling material beyond the apex: endodontic failure versus clinical success
Many dentists believe that procedural errors in daily practice, such as extrusion beyond the apical foramen and contact of filling material (most often gutta-percha and zinc oxide eugenol sealer) with periapical tissues after treatment, are a direct cause of endodontic failure.
Some authors show the negative impact of extending the filling material beyond the apex on the predictability of endodontic treatment and emphasize the following:
- High incidence of postoperative pain with exacerbation of inflammation
- Toxicity of materials
- Constant irritation of the periapical tissues with manifestations ranging from mild inflammation to a general reaction of the body.
In contrast, other authors have argued that apex extrusion in itself does not directly contribute to endodontic failure, although it should be avoided. Ingle says that endodontic treatment can be successful despite extrusion of material beyond the root apex. Schilder notes that he has not encountered complications specifically associated with excessive filling of the canal. Weine states that periapical tissues, fortunately, tolerate contact with gutta-percha well and therefore endodontic failure due to its removal beyond the apex is rare. In most cases, there is no pathological radiological evidence, and sometimes there is even a decrease in the amount of excreted material due to phagocytosis.
Image 1 – Mandibular first molar with amalgam filling and insufficient root canal obturation.
After retreatment, the radiograph shows three-dimensional filling of the root canals with a slight extension beyond the apex in the mesial canals obturated with Thermafil #25 and in the distal canal obturated by vertical condensation of heated gutta-percha.
After 5 years, the excess material had disappeared and the periapical tissue remained healthy.
These contradictory results can be explained by differences in research methodology and different composition of the derived materials. In general, the most common causes of discrepancy are related to differences in apical anatomy, limiting the effectiveness of endodontic treatment in various clinical situations.
Image 2 - The main factors leading to the removal of material beyond the root apex:
- External inflammatory apical root resorption associated with apical damage to a previously treated tooth.
- Incompletely formed root.
- Excessive instrumentation with deviation from the natural course of the canal and apical perforation.
- Inadequate handling of plasticized or unplasticized gutta-percha and sealants during obturation.
It is extremely important to identify and distinguish between the removal of filling material in three-dimensionally cleaned, formed and obturated root canals and in canals with obstructive overflow in combination with incomplete internal obturation.
Image 3 – Typical view of an exposed gutta-percha point: note the scratches on the point.
Image 4 – The apical foramen is completely filled.
Image 5 – Proper expansion for obturation, but insufficient filling of the canal. Note the transport of the apex during canal formation. (Courtesy of Dr. M. Vitullo)
Correct filling technique
There are many ways to fill a root formation: lateral condensation of gutta-percha, vertical condensation of heated gutta-percha, continuous wave method, using the Termafil system. However, each of these methods contains a general sequence of actions.
Any filling must include the following steps:
- Removal of all softened enamel and dentin tissue; it is advisable to expand the cavity to improve access to the canal orifices.
- Extraction of tooth pulp.
- Measuring the length of all root canals.
- Processing the canal walls and expanding its diameter using tools.
Treatment under a microscope guarantees the quality of the filling
To achieve the best result, files of different diameters are progressively used. At this stage of treatment, the “step back” technique is usually used - returning to the instrument with a smaller diameter in order to thoroughly clean the canal walls.
Read also: Dental restoration is
As soon as the doctor has treated the root formations, he begins filling. To avoid mistakes, the working length of the canal is measured again with an apex locator, the necessary instrument is left inside the root, and targeted radiography is performed.
After filling is completed, a control photo is taken to ensure that the material has reached the root tip.
A temporary filling is placed on the tooth, and after two to three days it is replaced with a permanent one.
If any of these sequences are broken, then there is a high probability that the filling material will extend beyond the top of the canal. And this can cause severe pain in the tooth, inflammation and pain in the gums, and in the absence of timely treatment, the formation of pus is possible.
Treated pulpitis. The paste extends beyond the root apex. What to do?
The tooth didn't hurt. There was a small caries, 4th tooth from below, on the left. Caries was treated. This was at the end of May 2020. Two weeks later the tooth began to ache. We waited for a while. The pain did not stop. Pulpitis was treated. When using the paste, the tooth ached slightly. The doctor decided to fill the canals. After the anesthesia wore off, the tooth hurt terribly. Now 10 days have passed. The tooth aches constantly, but not so much.
According to photographs and computed tomography, the filling paste from the canal went beyond the root tip. True, they say, not much. Where I treated them they said it was nothing to worry about.
What should I do, tell me? Photos from July 6 and 7, 2020
Indeed, the sealer has gone beyond the apex, and this is unacceptable. There is also a slight vacuum at the tops and, in addition, a foreign body, hence all your worries. Change doctor and see a more experienced therapist.
Comments and reviews 16
When filling the roots of a tooth, the doctor brought the filling paste beyond the apex of the root. Day 4 on painkillers after nerve removal. Will the paste dissolve? How dangerous is this? Answer
The picture is of poor quality; the roots of the teeth are not clearly visible. If the material extends beyond the apex by 2-3 mm, then it is unlikely that it will resolve. Answer
Dental surgeon-implantologist, C.M.N. Work experience 15 years.
I went for treatment to a paid, expensive clinic because I had a toothache. The doctor looked like an experienced woman, removed the nerve and put a filling. Before the filling, the doctor took a syringe with blue paste (I don’t know what it is) and wanted to treat the tooth. The syringe supposedly burst and a needle with a curved nose flew into my throat, and all this paste went into my mouth, it became very sour, my eyes darkened, it was very scary, I almost suffocated. Thank God I didn’t swallow it and spat out the needle. When this paste reacted with water, it turned out that the water was sweet. She received a burn to her mouth. I have a question: how is it possible that they almost killed me for my money? And what consequences should I expect for the stomach from this paste? At the moment the tooth continues to hurt, 4 days have passed. There is a 1 year warranty, but I don’t want to go to them. What should I do in this situation? Answer
The blue paste syringe is an etching gel (37% phosphoric acid). Unfortunately, no one is immune from technical unforeseen circumstances. Ideally, the doctor should work with a coffee dam, which protects against such situations. If concentrated acid falls on the mucous membrane, a burn may occur to the mucous membrane of the oral cavity, and if swallowed, to the esophagus. Phosphoric acid disrupts the acid-base balance in the body and leads to increased acidity. You need to contact a gastroenterologist to assess the condition of the gastrointestinal tract. Answer
Dental surgeon-implantologist, C.M.N. Work experience 15 years.
Please tell me, I really need help. A week and a half ago I was treating deep caries, the doctor warned that if there was pain, we would open and remove the nerves and clean the canals. After the freeze left, pain began, which was relieved with local analgesics. I suffered for a week, last week on Friday I went to the dentist, but not to my doctor, but to another one, since mine is on vacation. The doctor unsealed it, removed the nerves and cleaned two canals. They put a temporary filling in and told me to come back on Tuesday. The pain is aching again. Today I went and had an x-ray done. The picture shows that the filling material or paste, I don’t know (it’s a temporary filling now) has gone beyond the canal. But a specialist, a general practitioner, looked at the picture and said that this was the norm. Could this be the cause of my pain? I will be very grateful for the answer. Answer
Depending on the amount of excreted material and the clinical situation. But according to all the rules, the canals must be filled to the apex of the root to avoid complications in the form of inflammatory processes and pain. Answer
Dental surgeon-implantologist, C.M.N. Work experience 15 years.
After removing the nerve and filling the tooth, slight pain continues for about 3 weeks, and the taste (sour taste) of this new filling is disturbing. On the x-ray, the filling material extends slightly beyond the edge of the canal. This is fine? Answer
The removal of filling material can cause pain. If the canal is sealed with permanent filling material, the canal is often refilled. At the stage of temporary filling, a similar situation may be the norm. Answer
Dental surgeon-implantologist, C.M.N. Work experience 15 years.
I went to the doctor and they said everything was very bad. It is inside the untreated tooth that some kind of paste comes out of the canal and inflammation begins. Is it really that bad? Will it be possible to save my tooth? Answer
Yes, it is possible to save the tooth. The doctor should try to treat the tooth or resort to resection of the root apex. But you don’t need to immediately resort to removal, you need to fight. Answer
Dental surgeon-implantologist, C.M.N. Work experience 15 years.
They treated the tooth, filled the canals, and the material went beyond the canal into the gum. What should I do? Answer
Such teeth often need to be removed. If the filling material is permanent, it will no longer dissolve. Answer
Dental surgeon-implantologist, C.M.N. Work experience 15 years.
Thank you very much for the answer. My doctor refused to do anything, and I simply could not find a good doctor. I consulted at the Stoma clinic, the doctor was 80-90% sure that I had an untreated second canal. But I was so tired of the pain that I removed the tooth. Very sorry. This is what the root looks like in the photo. Could you tell me if there is a second channel? And the one in the last picture is sealed. Answer
Most likely, a second channel is present, and I also observe that the gutta-percha pins are pulled out beyond the apex (root apex), which is unacceptable and is a medical error. Answer
Contact phone number
Of course, I will go for a consultation with another dentist, but where can I be sure that he is a good one? Tell me what should I do in my situation? Re-treat, or some other action? I was told that a little paste came out. Answer
Exit of filling material beyond the tooth
Hello. My teeth on the right side have been hurting for about 3 weeks now. After visiting 4 doctors and taking pictures, we came to the following conclusion: the lower 6 should be re-treated, because it was poorly treated, caries remains, the nerve that gives sensitivity is close (2 weeks have passed since the treatment), the lower 8 is in progress treatment (in the picture with a temporary filling), what worries me most is the aching pain in the upper 7th. 3 doctors could not determine what was wrong, because 2 did not have an x-ray, one said about tooth sensitivity and advised special cleaning. paste. I went to the most expensive and equipped clinic in the city, and the doctor suspected that in 7 the filling material had leaked beyond the boundaries of the tooth. She said that if it was filled with gutta-percha, then they couldn’t help me - and that only removal. I treated this 7 exactly a year ago, also in a reputable clinic. The tooth didn’t hurt for a year, it got sick after I bit into something hard: a sharp pain, then aching. Is it possible that this filling material did not bother me for a whole year, but now it bothers me? From the photo - what can you tell? And one more thing: the doctor, as a temporary measure (I’m going on vacation abroad soon), suggested taking an antibiotic and ibuprofen - is this advisable? Thank you Patient age: 34 years