Tooth fracture - symptoms and treatment
Transverse (horizontal) fracture
In case of a fracture of the crown part of the tooth without damage to the pulp, caries may develop in the absence of treatment and subsequently pulpitis and periodontitis. In case of a fracture accompanied by exposure of the pulp, acute pulpitis is a complication. The occurrence of pulpitis is accompanied by pronounced pain in the area of the causative tooth with irradiation (spread) along the branch of the trigeminal nerve to the area of neighboring teeth or antagonist teeth. The pain mainly occurs at night. Without appropriate treatment, acute pulpitis can turn into chronic pulpitis, and later into periodontitis, characterized by the symptom of an “overgrown tooth” (the feeling that a tooth has come out; you cannot bite on it, as it causes pain). You can clearly identify the causative tooth by performing percussion - tapping on the tooth. Pain also occurs when eating hot food.
In the absence of treatment, after some time the process of pulp sclerosis begins - degeneration, pulp atrophy, its replacement with connective tissue. As a rule, there is no acute pain at this stage, but chronic inflammatory processes - osteitis or radicular cysts - begin to develop in the bone surrounding the tooth.
Vertical tooth fracture
This injury is incompatible with the continued existence of this tooth in the alveolus. Without treatment (in this case it involves tooth extraction), the situation leads to the rapid development of an inflammatory local process - dental periodontitis, which can later develop into periostitis (inflammation of the periosteum), osteomyelitis (chronic inflammation of the bone, which leads to resorption of bone tissue in the area of the lesion). ) and into extensive inflammation of soft tissues - an abscess of the maxillofacial area.
In this case, a purulent infiltrate appears around the tooth, melting the surrounding tissue. The patient's general condition worsens, the temperature rises, and swelling of the buccal or submandibular area occurs. Without appropriate treatment (tooth extraction, opening of periostitis or abscess), the process quickly becomes diffuse. In this case, phlegmon of the soft tissues of the face and neck may occur. Such a rapid and dangerous course of inflammatory processes in the oral cavity is due to the structural features of the cellular spaces of the face and neck. Cellular spaces are located between the muscle fascia. They are loose connective tissue. A distinctive feature of this tissue is the rapid development of purulent inflammation in it, which then spreads to nearby muscles and tendons.
Complications of a fracture also include resorption (external and internal) of the tooth root after injury. It appears after a few months. Resorption can be in the area of the apex (apex) of the root or in the area of the tooth root fracture. It occurs due to the lack of a “replacement callus”, which should restore the tissues of the tooth root - dentin and cement. The symptoms are quite sparse. This may be tooth mobility or pain when biting on a tooth. As a rule, it is possible to clearly diagnose resorption after an X-ray examination. This situation is a late complication of a tooth fracture. The tooth must be removed [9].
Kinds
In dentistry, cracks are divided into types, each of which is dangerous in its own way. However , lack of treatment and late diagnosis significantly reduce the chances of saving the tooth, regardless of the nature of the location of the gap in the enamel.
| Classification of cracks in teeth | |
| Name | Description |
| Vertical | This type is characterized by extensive damage to the tooth and root part. If the crack runs along the entire length of the tooth, restoring the structure and restoration is out of the question, a decision is made to remove the incisor. |
| Horizontal | If measures are not taken in a timely manner, a chip will form on the tooth. The closer the gap is to the gum, the greater the likelihood of part of the incisor chipping off. |
| Oblique | The crack runs diagonally across the protective layer of the tooth. Ignoring the problem creates favorable conditions for the development of pathologies. |
| Domestic | It is very difficult to detect such cracks, so during diagnosis they are referred for an x-ray. But often the patient sees the dentist only after a tooth fracture, which was caused by an undetected crack. |
| Root crack | The crack can pass through the root only or affect the tooth in any form. An extensive affected area indicates the need for molar removal. |
| Crack at the base | This type often causes additional problems as dentin is damaged. A crack can be detected by a symptom such as inflammation of the soft tissues around the tooth. With early diagnosis, the gap at the base is eliminated, this makes it possible to save the tooth. |
All types of cracks are conventionally divided into types:
- superficial;
- deep;
- multiple.
The first type is diagnosed much less frequently than the other two. In many cases, there is no pronounced aesthetic defect, so it is worth listening to the manifestations of characteristic symptoms.
The procedure for examining patients with injuries to the maxillofacial area
Patients often have a question: “What to do if a tooth is cracked in half?” or “What to do if the tooth root is cracked?”
In such cases, the dentist carries out the following diagnostic measures:
- Questioning the patient. The specialist finds out the patient’s complaints and the circumstances under which the injury occurred. At this stage, the dentist also pays special attention to the presence of signs of traumatic brain injury.
- Visual inspection. The doctor visually examines the condition of the skin of the face and neck.
- Oral examination . The dentist uses a probe and a mirror to examine the mucous membrane and dentition.
- Additional research methods . These diagnostic tests are designed to clarify the location of the fracture line and determine the viability of the pulp.
Additional examination methods include:
| Diagnostic test | Clinical picture |
| Radiography |
|
| Thermometry |
|
| Electroodontometry |
|
| Translumination |
|
A tooth cracked vertically: what to do?
Dentist surgeon, implantologist
Article checked by doctor
The appearance of vertical cracks in teeth is a rather unpleasant phenomenon that requires the intervention of dentists. At the same time, some experts believe that if there are minor cracks, teeth need not be filled if they do not cause discomfort or lead to pain.
If a crack occurs in a filled tooth, medical intervention is necessary. Only a dentist can prescribe qualified treatment, as well as find out how deep the crack penetrates into the tooth and what danger it poses.
It is especially worth examining cracks in teeth that react to sudden temperature changes or sweet or sour foods. The resulting discomfort may indicate the onset of caries or periodontitis, since healthy enamel does not respond to such food features.
A tooth cracked vertically: what to do?
Important! If an uncharacteristic and difficult-to-diagnose toothache occurs or there is a crack running deep into the root of the tooth, additional intervention by an endodontist who specializes in eliminating defects in the pulp and dental canals is required.
Options for cracked teeth
Causes of fracture
Cracks and fractures of the tooth crown and its root occur as a result of unevenly distributed loads.
The pressure spreads in a vertical (during direct impacts) or perpendicular (during closing jaws) direction. Most often, a tooth fracture is caused by injuries:
- Domestic injuries, such as a blow to the face or an unfortunate fall.
- Violation of tooth reconstruction technology. When installing a pin or during canal expansion, the doctor may destroy the root by applying too much force.
- Errors during treatment. If the bridge length is not optimal or the tooth crown is reconstructed incorrectly, the loads during chewing are distributed unevenly and the root may not withstand excessive impact.
Symptoms
Increased tooth sensitivity is one of the signs of cracks in the enamel.
The problem can be visually identified only on the front incisors. In other cases, when a crack forms, the patient comes to the clinic after the process of bone tissue decay has progressed. If you take into account the manifestation of symptoms characteristic of damaged tooth enamel, the chances of cure increase.
The following signs indicate the presence of a crack in the teeth:
- pain in the mouth without a specific localization;
- increased sensitivity of teeth when eating cold or hot foods;
- the process of grinding food is accompanied by pain.
In the absence of timely treatment, the problem is complemented by the following symptoms:
- inflammation of the gums or soft tissues near the damaged tooth;
- characteristic odor from the mouth;
- change in enamel color;
- bleeding when pressed or during hygiene procedures.
Diagnostics
X-ray of teeth
To identify a crack, in addition to a visual examination, the doctor uses special auxiliary tools and also writes out a referral for an x-ray. The image shows the extent of the affected area and the condition of the soft tissues.
Multiple cracks are diagnosed during examination without the use of instruments; deep cracks are determined under the influence of light, but after obligatory drying of the tooth surface with a cotton ball. And it is possible to detect surface damage only with the help of a magnifying glass (binocular, monocular) or by transillumination (carried out in a darkened room using a light guide).
Diagnosing a tooth root crack is a complex process that requires a lot of experience and knowledge. An erroneous diagnosis leads to the loss of a healthy tooth.
The difficulty in making a diagnosis is due to the lack of characteristic signs indicating the presence of a vertical crack in the tooth root. The doctor has to rely only on the patient's complaints, x-rays and symptoms that arise during examination and endodontic treatment.
It is worth noting that even an X-ray does not reflect the entire nature and locality of the crack , which is due to their location in the mesio-distal direction, which does not fall into the X-ray emission zone.
To make an accurate diagnosis, specialists conduct a thorough combined examination. This process includes the following activities:
- X-raying of teeth
examination of the oral cavity using a magnifying glass;
- examination under a microscope;
- transillumination;
- coloring;
- diagnostic operation.
The essence of the diagnostic operation is to peel off part of the dentin surrounding the tooth and remove granulation tissue for subsequent staining of the damaged surface with methylene blue. This visualizes the parameters of the crack and allows you to avoid misdiagnosis. Sometimes root resection is required for subsequent staining.
crack at the root - remove?
Moderator: Lesya
Read also: Temporary filling for pulpitis
crack at the root - remove?
Post by DmitryN » Wed Aug 15, 2012 15:39
In a private clinic, after a small chip, tooth 6 (46, an old problematic pulpless tooth) was prepared for prosthetics - an inlay and a metal-ceramic crown. The canals were partially filled, an impression was taken, and a temporary filling was inserted. The insertion of the inlay was scheduled after 9 days, but about a week later the prepared tooth began to sag a little. When the doctor removed the temporary filling to insert the tab, there was slight bleeding from the distal root and pain was felt. Examined by a therapist. She said that when the instrument is inserted, there is slight bleeding from two channels, therefore, most likely there is a crack. They sent it for deletion, which made us very upset, because... I wanted to preserve my roots. The picture shows a chipped tooth before filling and after filling, when there was bleeding. I wanted to clarify two questions: 1) do you really need to delete it, or are there any options with the tab? 2) what is better to place an implant (and which one) or a bridge with depulpation of the healthy five and a crown on the dead seven (doctors suggest)? The tooth hurts a little when pressed. Thanks in advance. Based on your answer, I will decide what to do next and where to get treatment.
Re: crack at the root - remove?
Post by Lesya » Wed Aug 15, 2012 21:49
Good evening. Yes, a root crack is a serious problem, especially when it comes to placing a tab on these roots. If there is indeed a crack or perforation in the root, the main problem is that blood and fluid will leak from this place, thereby soon this tab will become cemented and the crown will fall out. That's why the doctor started talking about removal. If there is no chance of sealing this crack and being sure that it will work, then it’s a pity to charge you money for an inlay and a crown. Now there are materials that make it possible to hermetically close perforations, but it all depends on the size of the crack or perforation.
I cannot tell you what to do, since I personally cannot check the tooth. If you are in doubt, it is better to show up to someone else. Let you have the opinions of at least two general practitioners. If the second one says that there is a perforation (or crack), then it is better to remove the tooth. Since any prosthetics for a cracked tooth will obviously be without a guarantee and most likely not successful. That is, at best, a year, then the root will crack and everything will collapse. If you are ready to take a risk, then you can try to seal the MTA perforations (if they are not large), do prosthetics without a guarantee and see what happens next. In this situation, the main thing is not to combine the 6th tooth with 7 crowns, let each one be on its own. So at least you don’t risk having to redo two teeth at once if the root cracks completely.
If the tooth is removed: what to do next? The 7th tooth is in such a condition that it also needs prosthetics. Most of the tooth is already a filling, and in the absence of the main chewing tooth (6), it will begin to crumble under the load. That is, it will have to be covered with a crown. And then it all comes down to finances and the condition of the 5th tooth. If the 5th tooth is without a filling, without caries, and you can afford to pay for an implant, then, of course, it is better to leave the 5th tooth alive and not make a bridge. If there is already caries on it, it is large and you understand that implantation is not yet possible for you, it is better to make a ceramic bridge, preparing the 5th tooth for this. Therefore, for now, I would advise having the 6th tooth checked by another doctor, listening to another opinion and only then deciding what to do. But you need to consult in person, since the decision to delete is never made solely on the basis of the image. You must see it with your own eyes and hands. how bad is everything there?
Clinical picture and tactics of treatment of fractures and traumatic injuries to the coronal part of the tooth
In dental practice, doctors most often encounter the following types of injuries:
Crown cracks
This type of damage is considered an incomplete type of fracture, in which the external integrity of the tooth is preserved. The cause of the crack is a sharp blow. As a result, the front tooth is more likely to suffer.
During a visual examination of the oral cavity, a specialist may notice several random lines on the problem tooth, which are directed towards the junction of enamel and dentin.
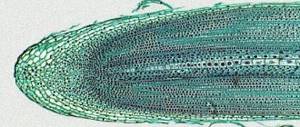
Microcracks on the front surface of the central incisors
As a rule, there is no special treatment for this type of traumatic injury. In such cases, the doctor must check the viability of the pulp. This test should be repeated after 1, 3, 6 and 12 months.
Fracture of a tooth within the enamel
Damage to the enamel mainly does not cause pain in the patient. The main complaints in this case are associated with concomitant trauma to the tongue and lips from the sharp edges of the problematic tooth. In addition, the patient pays attention to aesthetic discomfort in the oral cavity.
Enamel fracture of the central incisor
During examination of such a tooth, an enamel defect with rough edges is noticeable. Erosion is possible on the surface of the nearby mucous membrane.
Treatment for this injury involves grinding off the sharp edges. Filling of the enamel defect is carried out after 1-1.5 months. This is the time needed to restore the pulp and periodontium.
Crown fracture, which is accompanied by preservation of the integrity of the pulp chamber
Such damage is diagnosed by the characteristic external appearance of the damaged tooth.
Trauma of the central incisors within the peripulpar layer of dentin
During a survey of the patient, the dentist notes complaints of pain from temperature, chemical or mechanical stimuli. Probing the cavities also causes an attack of acute pain. But tapping on a problematic tooth does not cause discomfort.
Treatment of this pathology is essentially similar to the treatment of enamel fractures. Only in this case, before installing a composite restoration, the doctor isolates the pulp chamber using calcium-containing material.
Traumatic damage to the crown and pulp
Patients with such damage complain of prolonged and intense attacks from all types of irritants. A damaged tooth becomes sharply painful when biting or touching it.
In such cases, doctors must conduct an X-ray examination to exclude a fracture of the root system.
Root fracture and opening of the pulp chamber
An intraoral examination shows a bleeding point at the bottom of the injured area of the tooth, which indicates an opening of the pulp chamber.
Treatment of injury is aimed at removing the neurovascular bundle, antiseptic treatment of the root canals and filling them. All of the above manipulations should be carried out under local anesthesia.
After treatment of the tooth root, the doctor restores the crown part using photopolymer. The installation of fiberglass pins helps strengthen the restored part of the tooth. Such restorations are distinguished by excellent aesthetic properties and accurate recreation of the anatomical structure of the injured tooth.
Fixing the fiberglass pin
Classification of dental trauma
Varieties of classifications of dental trauma.
According to the International Classification of Dental Diseases based on ICD-10 (WHO, Geneva, 1997), the following dental injuries are distinguished:
- S02.5 Tooth fracture.
- S02.50 Fracture of tooth enamel only;
- S02.51 Crown fracture without pulp damage;
- S02.52 Fracture of the tooth crown with damage to the pulp;
- S03.53 Fracture of tooth root;
- S02.54 Fracture of the crown and root of the tooth;
- S02.57 Multiple fractures of teeth;
- S02.59 Tooth fracture, unspecified;
- S03.2 Tooth dislocation;
- S03.20 Tooth luxation;
- S03.21 Tooth intrusion or tooth extrusion;
- S03.22 Tooth dislocation (disarticulation).
Elements of classification of tooth trauma according to N. M. Chuprynina (Moscow, 1993)
- Tooth luxation:
- Incomplete tooth dislocation;
- Complete tooth dislocation;
- Impacted tooth dislocation
- Tooth root fracture:
- Longitudinal fracture of the tooth root;
- Transverse fracture of the tooth root;
- Oblique fracture of the tooth root;
- Displaced tooth root fracture;
- Fracture of a tooth root without displacement.