The symptoms and treatment of the trigeminal nerve, if it is affected, is complex.
Includes the use of medications, physiotherapeutic methods, and traditional medicine.
Find the answer Are you having a problem? Enter “Symptom” or “Name of the disease” into the form, press Enter and you will find out all the treatment for this problem or disease.
The site provides reference information. Adequate diagnosis and treatment of the disease is possible under the supervision of a conscientious doctor. Any medications have contraindications. Consultation with a specialist is required, as well as detailed study of the instructions! Here you can make an appointment with a doctor.
Nerve cells do not regenerate, so protecting the nerve from inflammation is one of the body’s main tasks.
Possible causes of a pinched nerve
A pinched nerve occurs due to injuries and dental operations (extraction, dental treatment, dentures):
- The pain is aching and prolonged in the jaw area.
- This is accompanied by weakening of the masticatory muscles, trismus (convulsive contraction of the masticatory muscles, accompanied by clenching of the teeth).
- The patient has difficulty speaking, chewing and swallowing.
- Sometimes pinching is accompanied by “goosebumps” crawling across the body.
- A disorder of autonomic function occurs, which leads to circulatory disorders. This can be expressed in increased salivation or dry eyes, the formation of ulcers in the area of the nasolabial folds.
Treatment at home is designed to relieve symptoms in order to prevent further inflammatory process and as a preventive measure.
In many cases, heating is used. Although experts have different opinions on this matter, warming up and hot baths restore the circulatory system and dull the nerve endings.
Warming ointments (“Viprosal”, “Finalgon”, “Capsicam”) are used for the same purpose.
For the anti-inflammatory treatment of neuritis at home, various decoctions, tinctures, compresses, and oils from medicinal plants are used:
- Fir oil Its regular use relieves the most acute pain. To do this, moisten a cotton swab with oil and gently rub it into sore spots 5-6 times a day. Minor redness and swelling may appear, which disappear quickly.
- Aloe Peel the aloe leaves, squeeze out the juice using gauze. Take 30 minutes before meals 3 times a day. This juice cannot be stored, so it should be taken immediately after preparation.
- Chamomile Take 3 tablespoons of chamomile flowers, pour 1 glass of boiling water. After 20 minutes, strain, take the resulting tincture 3 times a day, dividing into equal parts.
- Radish and lavender oil This mixture, prepared at the rate of 20 drops of radish juice per 1 drop of lavender oil, is carefully rubbed in the direction of the facial nerve. Cover with a towel on top for 30 minutes.
If the facial nerve is pinched, massage procedures aimed at relaxing the facial muscles and relieving inflammation will be effective.
Before any use of folk remedies, you must consult a doctor!
Preventive measures aimed at preventing nerve inflammation are important.
For this purpose, it is necessary to strengthen the immune system, and to do this, carry out hardening procedures as often as possible, walk in the fresh air, completely give up bad habits, and lead an active, healthy lifestyle.
Regular medical examination is recommended. And the most important helpers in the fight against any disease are a positive attitude and self-confidence.
Causes of inflammation of the trigeminal nerve
The etiology of nerve inflammation is mixed and has several causes.
Hypothermia is one of the main causes.
Many people are susceptible to inflammation during the off-season due to temperature changes. Draft, damp weather, strong wind outside, air conditioning in rooms can contribute to weakening of the immune system and the development of the inflammatory process.
Other causes of nerve inflammation:
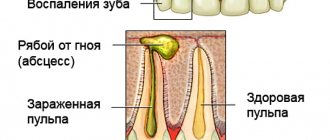
- Infection and its various complications.
- Inflammatory processes in the ear, chronic infectious diseases (tuberculosis, syphilis, herpes), sinusitis, caries can disrupt the structure of the nerve. The onset of inflammation is confused with sinusitis due to the similarity of symptoms; as a result, a person prescribes incorrect self-medication, which leads to complications.
- Multiple sclerosis, which affects the spinal cord and brain, paralyzing nerve endings, which leads to neuritis and many complications.
- Brain tumors.
- Congenital pathologies.
- Incorrect placement of blood vessels on the face can cause compression of nerve branches. Surgery may be required.
- Injuries, damage.
- Surgical intervention – in cases of maxillofacial injuries and facial injuries that lead to severe pinched nerves.
Anatomy of the ternary nerve
The ternary is the fifth pair of cranial nerve tracts. Essentially it is mixed, that is, it contains various fibers, among which are the following types:
- sensory fibers are of two types - centripetal and afferent;
- motor fibers or centrifugal (thanks to these fibers, information passes to the brain through electrical impulses about pain sensations in both superficial tissues, for example, information about skin pain, burns, and information from deeper structures, such as proprioceptive receptors.
Tissue movement is carried out due to the presence of the motor nucleus, which provides the innervation system predominantly to the masticatory muscles. The ternary branches off from the brain in the pons. At the exit from the cranium, most of the fibers pass along the pyramid of the temporal bone. It is at the top of this bone formation that the nerve fibers are divided into three branches, which represent separate nerves, such as:
- Orbital;
- Mandibular;
- Maxillary nerve.
The ternary, together with all three branches, are of particular interest to neurologists; it is also the main one when examining facial paralysis. This is due to the fact that this path powers the entire human face, ensures motor activity of muscle tissue, sensitivity and conduction of impulses to the brain and back. It is quite often affected by exposure to negative factors, such as severe hypothermia of the facial part or the entire head, as well as injury or disease of the musculoskeletal system. Therefore, it is very important to monitor the health of the nervous system and avoid harmful factors.
Symptoms of neuralgia, principles of therapy
Neuralgia is a pronounced pain attack in a nerve without visible changes in the nerve trunk.
To a greater extent, its appearance is facilitated by hypothermia, and to a lesser extent by infectious diseases, injuries and tumors. More often, women over 40 years of age are susceptible to neuralgia; men suffer less often.
The symptoms are the same for everyone:
- A sudden sharp pain appears, progressing over 1-2 minutes, disappearing as abruptly as it appeared.
- The pain syndrome is localized in one of the 3 branches of the nerve or in all 3 at once.
- The attack may cause “shooting” pain in the ear, eye, occipital, and cervical areas.
It is important to consult a doctor if these signs occur to avoid further complications!
Treatment is outpatient and comprehensive. The pain is relieved with the help of anticonvulsants.
The most common is carbamazepine, which reduces impulse in nerve fibers. Carbamazepine is contraindicated in pregnant women!
Drugs based on clonazepam, gabapentin and oxcarbazepine are used.
Painkillers (analgin, ibuprofen, ketorol, baclofen), antidepressants (amitriptyline, sodium hydroxybutyrate), and vitamin therapy are prescribed.
To enhance the effects of drugs, the doctor may prescribe a number of physiotherapeutic procedures: magnetic therapy, laser treatment, electrophoresis and acupuncture.
Surgical intervention is resorted to as a last resort, when medication does not produce results.
Features of treatment of neuritis
The main symptom of nerve inflammation (neuritis, trigeminitis) is pain (neuralgia). Strong, sharp and burning, it does not allow you to lead your usual lifestyle. The patient’s psychological state, sleep, and appetite are disrupted. This determines the main role of symptomatic remedies in treatment:
- Non-steroidal anti-inflammatory drugs (Diclofenac, Indomethacin, Ibuprofen) have an analgesic effect;
- Glucocorticosteroids (Hydrocortisone, Methylprednisolone, Dexamethasone) effectively and quickly fight inflammation;
- Anticonvulsants (Carbamazepine, Tegretol, Phenytoin) reduce impulses in the nerve fiber;
- Non-narcotic painkillers (Ketanov, Voltaren) and narcotic painkillers (Tramadol, Promedol);
- Muscle relaxants (Mydocalm, Baclofen) eliminate spasms of the facial muscles;
- Antidepressants (Amitriptyline) normalize the psychological state.
Drug treatment is usually combined with physiotherapeutic procedures; they enhance and prolong the analgesic effect:
- Cutaneous laser irradiation of the face;
- Ultraviolet irradiation of the face;
- Ultra-high frequency therapy (UHF);
- Diadynamic currents;
- Electrophoresis with B vitamins or with diphenhydramine, platiphylline, novocaine.
Guaranteed, but short-term relief is achieved by using alcohol-novocaine blockade at the nerve exit points on the face. The effect of each subsequent blockade is weaker than the previous one.
For final recovery it is necessary to influence the cause of the disease.
The source of the problem is often:
- Viral infections (shingles, multiple sclerosis);
- Pathology of the nose, paranasal sinuses (rhinitis, sinusitis or space-occupying formations - cysts, tumors);
- Facial injuries and their consequences (hematomas, bone fragments, post-traumatic edema can compress nerve fibers);
- Oral diseases (periodontitis, pulpitis, periodontitis);
- Dental manipulations: tooth extraction, inaccurate filling (the filling material is located outside the tooth root and is in contact with the nerve); errors when administering anesthetic;
- Compression of a nerve by an artery or vein (usually by cerebellar vessels) leads to damage to the nerve fiber sheath (demyelination) and its pathological excitability;
- Allergic or toxic swelling of facial tissues;
- Local or general hypothermia;
- Depletion of the body's protective abilities due to physical or psychological overstrain, deficiency of essential nutrients;
- Malocclusion, accompanied by permanent injury to the temporomandibular joint;
- Narrowing of the bone canals where the branches of the nerve pass, osteomyelitis;
- Pathology of the cervical spine (osteochondrosis).
Some causes can be treated medicinally using drugs:
- Antiviral (for herpes infection, acyclovir and its analogues are used);
- Antibiotics (for sanitation of foci of infection in the nose, paranasal sinuses, oral cavity);
- Antihistamines (to relieve post-traumatic, allergic, toxic edema);
- B vitamins (actively help restore nerve sheaths).
With cervical osteochondrosis and displacement of the facial bones, manual therapy gives good results.
More often, the source of irritation can only be eliminated surgically. Possible options:
- If the cause is a tumor that can be operated on, surgery is performed to remove it.
- In case of narrowing of the infraorbital canal, in which the branch of the nerve passes, a low-traumatic operation to widen it is effective.
- When a nerve is compressed by an artery or vein, microvascular decompression of the nerve root is performed (a spacer is placed between the vessels and the nerve root).
Sometimes the cause remains unclear, and symptomatic treatment does not produce a noticeable result. Violation of nerve fiber conduction is achieved through surgery.
The following types of interventions are used:
- Percutaneous radiofrequency destruction (destruction) of nerve roots. It is performed under local anesthesia. The method is highly effective and has a minimum of contraindications and can be performed on an outpatient basis.
- Stereotactic radiosurgery (cyber knife, gamma knife) – the sensitive root is destroyed using gamma radiation.
Maxillary nerve (human anatomy)
Maxillary nerve
, n. maxillaris, the second branch of the trigeminal nerve, it is mainly sensory. Has a thickness of 2.5-4.5 mm; consists of 25-70 small bundles containing from 30,000 to 80,000 papillary nerve fibers of predominantly small diameter (up to 5 microns).
The maxillary nerve innervates the dura mater, the skin of the lower eyelid, the outer corner of the eye, the anterior part of the temporal region, the upper part of the cheek, the wings of the nose, the skin and mucous membrane of the upper lip, the mucous membrane of the posterior and lower parts of the nasal cavity, the mucous membrane of the sphenoid sinus, palate, dental organs and teeth of the upper jaw. Upon exiting the skull through the foramen rotundum, the nerve enters the pterygopalatine fossa, passes from back to front and from inside to outside. The length of the segment and its position in the fossa are related to the shape of the skull. With brachycephaly, the length of the nerve segment in the fossa is 15-22 mm; it is located deep in the fossa - up to 5 cm from the middle of the zygomatic arch. Sometimes the nerve in the pterygopalatine fossa is covered by a bone crest. With dolichocephaly, the length of the nerve section in question is 10-15 mm and it is located more superficially - up to 4 cm from the middle of the zygomatic arch.
Within the pterygopalatine fossa, the maxillary nerve gives off the ramus meningeus to the dura mater and is divided into three branches: 1) pterygopalatine nerves, nn. pterygopalatini, going to gangl. pterygopalatinum; 2) zygomatic nerve, n. zygomaticus; 3) inferior orbital nerve, n. infraorbitals, which is a direct continuation of the maxillary nerve (Fig. 232, 233).
Rice. 232. Scheme of the structure of the maxillary nerve
1. Pterygopalatine nerves, nn. ptery go palatini, very variable in number (1-7) and length (9-30 mm); depart from the maxillary nerve at a distance of 1-2.5 mm from the round foramen and go to the pterygopalatine ganglion, giving sensory fibers to the nerves starting from the ganglion. Some pterygopalatine nerves bypass the ganglion and join its branches.
Pterygopalatine ganglion, gangl. pterygopalatinum, - the formation of the parasympathetic part of the autonomic nervous system. The node is triangular in shape, 3-5 mm long, contains multipolar cells and has three roots: a) sensitive - nn. pterygopalatine b) parasympathetic - greater petrosal nerve, n. petrosus major, a branch of the intermediate nerve that carries secretory fibers to the lacrimal gland, to the glands of the nasal cavity and palate; c) sympathetic - deep petrosal nerve, n. petrosus profundus, a branch of the plexus caroticus internus, containing postganglionic sympathetic nerve fibers from the cervical ganglia. Branches extend from the node, including secretory (parasympathetic and sympathetic) and sensory fibers: orbital branches, rami orbitales; posterior superior nasal branches, rami nasales posteriores superiores; palatine nerves, nn. palatini (see Fig. 233).
Rice. 233. Olfactory nerve, pterygopalatine ganglion and branches of the trigeminal nerve. 1 - lower nasal passage; 2, 4, 7 - lower, middle and upper turbinates; 3 - middle nasal passage; 5 - olfactory bulb; 6 - olfactory nerves; 8 - sphenoid sinus; 9 - optic nerve; 10, 23 - internal carotid artery; 11 - oculomotor nerve; 12 - pterygopalatine node; 13 - orbital nerve; 14 - maxillary nerve; 15 - trigeminal node; 16 - nerve of the pterygoid canal; 17 - trigeminal nerve; 18 - greater petrosal nerve; 19 - deep petrosal nerve; 20, 31 - facial nerve; 21 - vestibulocochlear nerve; 22 - internal carotid nerve plexus; 24 - lingual nerve; 25 - lower alveolar nerve; 26 - drum string; 27 - middle artery of the meninges; 28 - maxillary artery; 29 - styloid process; 30 - mastoid process; 32 - parotid salivary gland; 33 - perpendicular plate of the palatine bone; 34 - medial pterygoid muscle; 35 - palatine nerves; 36 - soft palate; 37 - hard palate; 38 - upper lip
The orbital branches, rami orbitales, in the amount of 2-3 thin stems, penetrate through the lower orbital fissure into the orbit and further along with n. ethmoidalis posterior go through small openings in the sutura sphenoethmoidalis to the mucous membrane of the posterior cells of the ethmoid labyrinth and the sphenoid sinus.
The posterior superior nasal branches, rami nasales posteriores superiores, in the number of 8-14 stems, emerge from the pterygopalatine fossa through the foramen sphenopalatinum into the nasal cavity, concentrated in two groups: lateral and medial. The lateral branches, rami nasales posteriores superiores laterales (6-10 stems), go to the mucous membrane of the posterior sections of the superior and middle nasal concha and nasal passages, the posterior cells of the ethmoid sinus, the upper surface of the choanae and the pharyngeal opening of the auditory tube. The medial branches (2-3 trunks) branch in the mucous membrane of the upper part of the nasal septum. One of the medial branches is the nasopalatine nerve, n. nasopalatinus, passes between the periosteum and the mucous membrane of the septum together with a. nasalis posterior septi forward to the nasal opening canalis incisivus, through which it reaches the mucous membrane of the anterior part of the palate. Forms a connection with ramus nasalis n. alveolaris superior.
Palatine nerves, nn. palatini, spread from the node through the canalis palatinus major, forming three groups of nerves: a) greater palatine nerve, n. palatinus major; b) small palatine nerves, nn. palatini minores; c) lower posterior lateral nasal branches, rami nasales posteriores inferiores laterales.
Greater palatine nerve, n. palatinus major, the thickest branch, exits through the foramen palatinum majus to the palate, where it splits into 3-4 branches that innervate most of the mucous membrane of the palate and its glands in the area from the canines to the soft palate.
Lesser palatine nerves, nn. palatini minores, enter the oral cavity through the small palatine openings, branch in the mucous membrane of the soft palate and the region of the palatine tonsil, as well as in m. levator veli palatini (motor fibers come from n. facialis through n. petrosus major).
The lower posterior lateral nasal branches, rami nasales posteriores inferiores laterales, enter the canalis palatinus majus, leave it through small openings and, at the level of the inferior nasal concha, penetrate the nasal cavity, innervating the mucous membrane of the inferior concha, the middle and lower nasal passages and the maxillary sinus.
2. Zygomatic nerve, n. zygomaticus, branches off from the maxillary nerve within the pterygopalatine fossa and penetrates through the inferior orbital fissure into the orbit, where it runs along its outer wall and exits through the foramen zygomaticoorbitale, dividing into two branches.
The zygomaticofacial branch, ramus zygomaticofacialis, exits through the foramen zygomaticofaciale onto the anterior surface of the zygomatic bone, branches in the skin of the upper part of the cheek and the region of the outer canthus. Gives a connecting branch to n. facialis.
The zygomaticotemporal branch, ramus zygomaticotemporalis, leaves the orbit through the opening of the same name in the zygomatic bone, pierces the temporal muscle and its fascia, and innervates the skin of the anterior part of the temporal and posterior part of the frontal regions. Gives a connecting branch to n. lacrimalis, sending secretory parasympathetic fibers to the lacrimal gland.
3. Inferior orbital nerve, n. infraorbitalis, is a continuation of the maxillary nerve, receiving its name from the origin of the last branches mentioned above. The inferior orbital nerve leaves the pterygopalatine fossa through the inferior orbital fissure, lies together with the vessels of the same name on the lower wall of the orbit in the sulcus infraorbitalis (in 15% of cases there is a bone canal instead of a groove) and exits through the foramen infraorbitale under the quadratus labii muscle, dividing into terminal branches . The length of the inferior orbital nerve varies. In brachycephals, the nerve trunk is 20-27 mm, and in dolichocephals it is 27-32 mm. The position of the nerve in the orbit corresponds to the parasagittal plane, drawn through the sutura infraorbitalis. The nature of the origin of the branches can also be different: scattered, in which numerous thin nerves with a large number of connections depart from the trunk, or main with a small number of large nerves. Along its path, the infraorbital nerve gives off the following nerves:
Superior alveolar nerves, nn. alveolares superiores, innervating the teeth and upper jaw. The following branches of the superior alveolar nerves are distinguished: a) posterior, b) middle, c) anterior (Fig. 234).
Rice. 234. Maxillary nerve. 1 - posterior upper alveolar branches; 2 - zygomatic nerve; 3 - maxillary nerve; 4 - nerve of the pterygoid canal; 5 - orbital nerve; 6 - trigeminal nerve; 7 - mandibular nerve; 8 - drum string; 9 - ear node; 10 - connecting branches of the pterygopalatine ganglion with the maxillary nerve; 11 - chewing nerve; 12 - inferior alveolar nerve; 13 - lingual nerve; 14 - pterygopalatine node; 15 - inferior orbital nerve; 16 - anterior upper alveolar branches
The posterior superior alveolar branches, rami alveolares superiores posteriores, branch from the lower orbital nerve, usually in the pterygopalatine fossa in an amount of 4 to 8 and spread together with the vessels of the same name along the surface of the tubercle of the upper jaw. Part of the most posterior nerves runs along the outer surface of the tubercle down to the alveolar process. The rest enter through the foramina alveolaria posteriora into the canalis alveolaris, from which they exit onto the outer surface and into the bone canaliculi of the upper jaw, forming with other upper alveolar branches the superior dental plexus, plexus dentalis superior. The plexus lies in the alveolar process of the upper jaw above the apices of the roots; it is quite dense, broadly looped, stretched along the entire length of the alveolar process. From the plexus extend the upper gingival branches, rami gingivales superiores, to the periodontium and periodontium, i.e., to the mucous membrane of the alveolar process, gum and socket in the area of the upper molars, and the upper dental branches, rami dentales superiores, to the apices of the roots and foramina apicalia of the large molars, in the pulp cavity of which they branch. In addition, the posterior superior alveolar branches send thin nerves to the mucous membrane of the maxillary sinus.
The middle superior alveolar branch, ramus alveolaris superior medius, in the form of a stem, rarely 2, branches from the inferoorbital nerve, often in the pterygopalatine fossa and less often within the orbit, passes in one of the alveolar canals and branches in the bone canaliculi of the upper jaw as part of the plexus dentalis superior. It has connecting branches with posterior and anterior superior alveolar branches. Innervates the periodontium and periodontium through the upper desial branches in the area of the upper premolars and the upper dental branches - the upper premolars.
The anterior superior lunate branches, rami alveolares superiores anteriores, usually in the amount of 1-2 trunks, rarely 3, arise from the inferoorbital nerve in the anterior part of the orbit; they leave it through the foramina alveolaria anteriora and exit through the canalis alveolaris onto the anterior surface of the upper jaw, where they form part of the plexus dentalis superior. The mucous membrane of the alveolar process, gums and sockets in the area of the upper canines and incisors and the upper dental branches - the upper canines and incisors - are innervated by means of the upper desi branches. In addition, the anterior superior alveolar branches send a thin nasal branch to the mucous membrane of the anterior nasal cavity.
2. The lower eyelid branches, rami palpebrales inferiores, branch from the lower orbital nerve at the exit from the foramen infraorbitale, penetrate through the quadratus muscle of the upper lip and, branching, innervate the skin of the lower eyelid.
3. The external nasal branches, rami nasales externi, innervate the skin in the area of the wing of the nose.
4. The internal nasal branches, rami nasales interni, supply the mucous membrane of the nasal vestibule.
5. The superior labial branches, rami labiates superiores, in the amount of 3-4 stems, run down between the upper jaw and the quadratus muscle of the upper lip, innervating the skin and mucous membrane of the upper lip to the corner of the mouth. All of the listed external branches of the inferior orbital nerve form connections with the branches of the facial nerve.
content .. 189 190 191 192 193 194 195 196 197 198 199 ..
What is neuritis
With neuritis, the branch of the maxillary facial nerve is affected. This is manifested by the following symptoms:
- A person experiences severe, acute pain that is cyclical in nature.
- Painful sensations have a characteristic and uncharacteristic form. In the first case, the pain is inconsistent, heterogeneous, in the second, it lasts all the time, which significantly complicates treatment.
- Nervous tics, increased sweating, cramps of the masticatory muscles, and pain in the cervical vertebrae are observed.
- A set of measures is used to relieve the current attack and prevent the next one.
- To relieve severe pain, a blockade with novocaine is used, and physiotherapeutic procedures are prescribed.
- Among the drugs prescribed are anticonvulsants (carbamazepine), which block the activity of nerve cells, glucocorticosteroids (prednisolone), non-steroidal anti-inflammatory drugs (Voltaren, diclofenac, ibuprofen, Celebrex).
- To consolidate the effect, B vitamins are prescribed.
Neuritis – when a nerve is overly inflamed
Neuritis of the facial nerve is a one-sided lesion, develops gradually, manifests itself with symptoms:
- weakness in the facial muscles, paresis (paralysis) appears;
- changes in the sensitivity of the skin and muscles of the affected part of the face;
- involuntary twitching of facial muscles;
- distortion of the face, it stretches out;
- impaired motor function of the eye, lacrimation or dryness;
- increased salivation;
- taste disturbance;
- pain in the ears, changes in hearing from deafness to increased hearing.
- variable muscle pain.
Drug treatment of facial nerve neuritis:
- non-hormonal anti-inflammatory drugs (Indomethacin, Piroxicam);
- corticosteroid anti-inflammatory drugs (Dexamethasone, Methylprednisolone, Prednisolone);
- decongestants (Lasix, Diacarb);
- painkillers (Pentalgin, Ibuprofen);
- antispasmodics (No-shpa, Drotaverine);
- anticholinesterase drugs that restore neuromuscular conduction (Nivalin, Galantamine).
According to indications, medications are prescribed that activate metabolic processes in the nervous tissue (Nerobolil, Dinabolon).
Massage, exercise therapy, reflexology, electrotherapy with pulsed current, ultrasound, and ozokerite applications are used.
If the disease is secondary, the underlying disease is treated.
Massage for neuritis of the facial nerve:
\
Colds facial neuritis
It begins acutely, develops quickly, and can recur. If the facial nerve is cold, the following symptoms appear:
- decreased motor function of the facial muscles;
- facial asymmetry, relaxation of facial muscles;
- numbness of the facial muscles;
- pain behind the ear;
- distorted perception of loud sounds;
- The eye does not close, it waters.
Complex treatment of the disease is carried out according to the same scheme as the treatment of other nerve lesions.
Trigeminal neuropathy
This is a characteristic pain syndrome involving the 5th cranial nerve, caused by various traumas and maxillofacial injuries.
More often, neuropathy occurs in the mandibular branch during dentures and other maxillofacial operations.
Symptoms of neuropathy:
- There is a loss of facial sensitivity and weakening of the masticatory muscles.
- The pain is aching and one-sided.
- The severity of the disease varies for many people depending on the individual location of the facial nerve. When the branch of the mandibular nerve is damaged, the ability to lower the lower jaw is impaired.
- There are frequent cases of complete numbness of the face, indicating idiopathic neuropathy (Bell's palsy).
For neuropathy the following is prescribed:
- B vitamins (riboflavin, cyanocobalamin, thiamine),
- Anti-inflammatory drugs,
- Painkillers analgesics (ketorol, baralgin, tempalgin);
- Sedatives (valerian tincture, Corvalol, motherwort).
Causes and prevention of mandibular nerve injuries
The only cause of such damage is considered to be medical errors. Since in preparation for implantation, X-rays of the jaw are taken, which the doctor must carefully study so that when choosing an implant and a place for it, he does not injure the nerve, the injuries are caused by his unprofessionalism or negligence.
Damage to the mandibular nerve most often occurs when:
- improper administration of anesthesia - needle injury;
- choosing an implant that is too long;
- damage by an instrument - when preparing the site for the implant.
The only way to avoid such an injury is for a doctor to responsibly approach the stage of preparation for surgery, carefully studying the condition and structure of his patient’s jaw. The only way of prevention for the patient is to choose a trusted clinic and a highly qualified doctor. Specialists at the Implantmaster clinic have been able to reduce the number of injuries of this kind to 2%, since they carefully study three-dimensional photographs of a person’s jaw before implantation, and can correctly assess the condition of the bone tissue, the location of nerves and blood vessels, and select the optimal size of the implant.
What worries patients if the nerve is cold?
Most people enter the doctor's office in winter complaining of ear pain and difficulty in facial movements.
The nerve can easily get cold. Acute pain in the ear, temple, lower jaw on one side of the face is one of the main manifestations of a cold.
Facial expressions become difficult; in some cases, a person cannot even close his eyes, open his mouth or puff out his cheeks. Damage to the facial nerve can be unilateral or bilateral.
You cannot self-medicate; you must consult a doctor. Many diseases have similar symptoms; if all the symptoms are not removed in time, various complications arise (rashes in the ear, paralysis of the facial muscles, drooping eyelids).
Neuralgia - pain piercing through and through
The main symptom of facial neuralgia is pain, greatest at the exit of the nerve from the skull. It occurs suddenly, of varying strength and localization.
- Associated symptoms:
- muscle weakness with the development of paresis;
- increased or decreased muscle sensitivity;
- development of facial asymmetry;
- excessive salivation and lacrimation;
- loss of taste to the point of complete absence.
Treatment of facial neuralgia is most often medicinal, the following drugs are prescribed:
- anticonvulsants (Carbamazepine, Tebantin);
- muscle relaxants to reduce muscle tension (Baclofen, Sirdalud);
- analgesics, for severe pain - opiates;
- psychotropics to relieve depression (Trazodone, Amitriptyline);
- non-hormonal anti-inflammatory ointments, gels, creams (Diclofenac, Diclak-gel);
- preparations containing vitamin B (Neurorubin, Milgama).
Additionally, electrophoresis with lidocaine, acupuncture, UHF, and microcurrent treatment are prescribed. Light massage and special gymnastics are recommended.
If this treatment is ineffective, they resort to operations - decompression and electrical stimulation of the motor cortex of the brain.
The most effective methods from the patients' point of view
Among patients suffering from trigeminitis, symptomatic remedies are in demand. Diclofenac or drugs based on it help well, with preference given to suppositories or injections.
From the arsenal of traditional medicine to combat pain they use:
- Infusion of common yarrow (per glass of boiling water - a tablespoon of dried herb, infused for 1 hour, take 1 tablespoon 3 times a day);
- Decoction of the root of the plant Amphibian Highlander (one and a half glasses of water per teaspoon of crushed root, boil for 10 minutes, leave for 2 hours, strain, divide into 3 doses per day);
- Hard-boiled egg (cut it in half, apply the halves to the sore spots, as the egg cools, the pain subsides).
Acupuncture (acupuncture) is known for its effectiveness; everyone who used this method noted that after a session of procedures the pain subsided for a long time.
Often, to relieve a painful attack, a complex of analgesics, anticonvulsants, B vitamins (in injection form) and physiotherapeutic procedures (laser therapy) is used. Remission is achieved after 1-2 months. In the vast majority of patients, the effect of this treatment is temporary. The vast majority of patients agree that it is possible to completely get rid of pain only through surgical methods.
Prevention of nerve inflammation
- Careful, timely treatment of foci of infection in the nose, ears and eyes.
- Sanitation of the oral cavity.
- Avoiding hypothermia, especially staying in a draft for a long time (for example, when driving fast in a vehicle with an open window).
- Healthy, balanced diet, seasonal use of multivitamin complexes.
- Hardening.
- Good sleep and rest.
- Adequate physical and mental stress.
- Avoiding facial injuries.
- If there are disorders in the cervical spine, regular massage courses are needed to prevent neuralgia.
Possible complications, consequences
There is no need to postpone a visit to the doctor if you suspect trigeminitis; in addition to debilitating pain, this disease is dangerous due to its consequences:
- Hearing loss;
- Paresis of the facial muscles (flabbiness of facial muscles) or, conversely, uncontrolled twitching;
- Cerebellar hematoma (if the cause of neuralgia is compression of the nerve root by the cerebellar vessels);
- Ataxia (impaired coordination of movements due to damage to the cerebellum);
- Deterioration of vision.
Doctor: Olga Shishkina ✓ Article checked by doctor