What is gingivitis?
Gingivitis is an inflammation of the gums, in which the mucous membrane becomes red and bleeds when brushing the teeth. The difference between this disease is that the ligamentous apparatus of the tooth is not destroyed, the symptoms are reversible. This distinguishes gingivitis from other gum diseases (periodontitis, periodontal disease), which progress inexorably and inevitably lead to tooth loss. In fact, gingivitis is the initial stage of inflammation, which is why it is so important to start treating it as early as possible.
Pathogenesis of catarrhal gingivitis
The mechanism of pathological changes in the gums can be briefly presented as follows. The stage of early inflammation is characterized by the penetration into the gum tissue of a large number (up to 70% of the total number of cells) of small and medium-sized lymphocytes, as well as polymorphonuclear leukocytes, macrophages, plasma and mast cells. Therefore, the morphological feature of the early stage of inflammation is precisely dense small cell infiltrates with a predominance of lymphocytes in the preparations.
In healthy gums, T-lymphocytes numerically predominate over B-lymphocytes in all its zones.
In chronic periodontitis, numerous B lymphocytes and plasma cells are found in the gums. The more severe the disease, the higher the content of B-lymphocytes and plasma cells producing IgG, IgA, IgM.
Morphologically, the phase of established inflammation is characterized by the predominance of plasma cells in the cellular infiltrate, which reflect the immune response to damage.
At the stage of established inflammation, a picture of a mixed infiltrate is observed, consisting of polymorphonuclear leukocytes, small and medium-sized lymphocytes, and large plasma cells. This indicates that a pattern of chronic and acute inflammation is simultaneously observed in the tissues.
The main difference between the phase of progressive inflammation is that... that plasma cells make up up to 80% of all exudate cells. This indicates the chronicity of inflammation and the active involvement of immune mechanisms of inflammation. Plasma cells are the final stage of development of B lymphocytes; they provide humoral immunity through the active production of immunoglobulins. In periodontal lesions, the number of plasma cells increases in proportion to the severity of the process and the degree of tissue destruction.
Causes and symptoms of gingivitis
The gums become inflamed due to a traumatic factor, which in most cases is hard and soft dental plaque. Doctors answer that 80% of Russian residents visit the dentist untimely, without performing professional cleaning of the oral cavity. Therefore, the vast majority of patients have initial problems with gums, expressed to one degree or another.
The next most common reason is the presence of defective fillings in the mouth that have chips and gaps. The sharp edge of such a restoration can not only damage the mucous membrane, but also cause inflammation of the adjacent gingival area. It is necessary to visit the dentist once every six months in order to correct the filling in time. On the website, you can tell your doctor whether a specific restoration is a provoking factor for gingivitis, and whether it needs to be changed. To do this, you need to send a clear photo of the tooth with a filling and the surrounding gum.
The main symptom of gingivitis is redness of the mucous membrane surrounding the necks of the teeth. When cleaning the oral cavity, the gums may bleed, and pain, itching and burning also often occur. A characteristic sign is their swelling, an increase in volume, they seem to be floating on the teeth.
Gingivitis - symptoms and treatment in adults
Common symptoms of inflammation are discomfort and bleeding gums, changes in taste, and bad breath. On examination, swelling, thickening of the gums and local foci of erosion are noted.
Treatment consists of several stages. First of all, foci of infection and hard deposits must be eliminated. During the treatment period, you should use soft toothbrushes and toothpastes with an anti-inflammatory effect.
Anti-inflammatory therapy is carried out using solutions and ointments, but in some more complex cases, the doctor may recommend surgical treatment. The use of folk remedies is also encouraged, but only as an additional auxiliary therapy.
How to distinguish gingivitis from other gum diseases?
Only a dentist can accurately diagnose gingivitis after examining all the teeth, examining with a special instrument - a periodontal probe, and taking an x-ray of the entire oral cavity - an orthopantomogram. However, certain features help distinguish gingivitis from other gum diseases.
Periodontitis
With periodontitis, the destruction of periodontal fibers occurs, as a result of which the tooth begins to become loose. This is the main difference between these two stages. However, it should be noted that in the initial stage of periodontitis, the patient will not always be able to see slight tooth mobility. Therefore, an accurate diagnosis can only be determined by consulting a periodontist.
Periodontal disease
Periodontal disease occurs as a result of a violation of the trophism (nutrition) of the gums, which causes it to thin and become pale in color. The necks of the teeth begin to become exposed, causing increased sensitivity to cold air, food, and drink. Unlike gingivitis, with periodontal disease there are no symptoms of inflammation of the mucous membrane - redness and swelling.
Gingivitis
In most cases, gingivitis occurs without disruption of the periodontal junction. If the entire gum of the jaw or both jaws is inflamed, then gingivitis has become widespread. But localized gingivitis is more often diagnosed when a small portion of the gum is affected. With limited gingivitis, nearby teeth are also affected. If only the gingival papillae are affected by gingivitis, then papillitis is diagnosed; if the entire gingival margin is affected, they speak of a marginal course of gingivitis.
In acute gingivitis, there are classic manifestations of the inflammatory process - swelling, hyperemia, local increase in tissue temperature, pain and hypersalivation. There is bleeding of the gums, pinpoint hemorrhages, and sometimes with gingivitis there may be ulceration of the gums.
Chronic gingivitis occurs due to prolonged exposure to adverse factors. And most often his clinical picture is blurry. The main manifestation of chronic gingivitis is gum hyperplasia; sometimes the entire crown of the tooth is covered with gum tissue, which normally should not be the case.
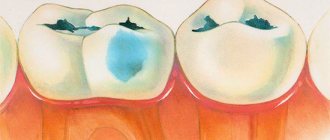
Catarrhal gingivitis is characterized by a pronounced inflammatory reaction, with redness and swelling of the gums. The inflamed surface becomes sensitive to temperature changes. Some patients with catarrhal gingivitis report itching and pain when eating.
With ulcerative-necrotizing gingivitis, ulcerated areas and areas of necrosis appear on the mucous membrane of the gums. The gums are sharply painful. Due to the proliferation of putrefactive microflora, halitosis appears - bad breath. The patient’s general condition suffers: the temperature rises, sometimes to febrile levels, and regional lymph nodes enlarge. Due to pain, food intake is disrupted, sometimes with gingivitis, persistent refusal to eat (anorexia) is observed, general weakness and symptoms of exhaustion increase.
Hypertrophic gingivitis is clinically manifested by an increase in gingival papillae, which over time cover most of the tooth. At the initial stages, hypertrophic gingivitis practically does not manifest itself, and there are no unpleasant sensations either. Tissue hyperplasia is usually noticed during a routine dental examination. But over time, in the absence of therapy, gum pain increases during eating and during touching. Brushing teeth for patients with hypertrophic gingivitis becomes a difficult and painful procedure; as a result, they refuse oral care, which results in multiple caries.
In addition to the phenomena of gingivitis and caries, there is bad breath, accumulation of plaque and tartar. Eating becomes sharply painful. A particularly acute reaction is observed when taking sour, hot and spicy foods. With atrophic gingivitis, gum atrophy occurs. The gum level gradually decreases, the neck of the tooth is exposed, and then its root. Subjectively, it manifests itself only as pain when eating cold or hot food.
During menopause, women often develop desquamative gingivitis. The formation of keratin-containing epithelial cells decreases, which is manifested by an increase in mucosal permeability. The gums are easily damaged, bleed and are painful even when touched slightly. Sometimes the appearance of gingivitis is preceded by the formation of blisters.
Gingivitis is not an independent disease. Basically, this is one of the clinical manifestations of periodontitis and periodontal disease, so it is important to promptly identify signs of gingivitis and carry out therapy.
Treatment and prevention of gingivitis
Treatment of gingivitis begins with eliminating its causes. First of all, the periodontist carries out a comprehensive cleaning of the oral cavity - removing hard tartar with an ultrasonic device, removing plaque with a sandblaster, polishing the enamel with an electric brush with an abrasive paste. If necessary, the doctor will teach the patient how to properly brush his teeth and select individual personal hygiene products (brushes, floss, rinses). Concomitant therapy is prescribed (oral baths with chlorhexidine, miramistin). If the cause of inflammation lies in poor-quality fillings, they are ground or redone. After following these measures, the symptoms of gingivitis disappear within 2-3 weeks.
Treatment of gingivitis
Correct diagnosis of gingivitis plays an important role in the treatment of the disease, since the pathology has similar symptoms to periodontitis, stomatitis and periodontal disease. When conducting an examination at the Telo's Beauty clinic, the basic diagnostic method is to calculate the hygiene index, which is carried out using special coloring preparations. They are applied to the dental plaque and, based on visualization, areas of damage to the tooth and gums are determined.
Additional diagnostic measures for gingivitis include:
- determination of bleeding of the gingival groove - is carried out using periodontal probes, which make it possible to identify hidden areas of bleeding;
- an x-ray with which the doctor can understand whether the disease is gingivitis or whether it has already turned into periodontitis;
- orthopantomogram - an x-ray study aimed at studying the condition of the roots and their rudiments.
After diagnosis, treatment for gingivitis is prescribed, the methods of which may vary depending on the form of the disease.
Treatment of acute gingivitis
Anti-inflammatory and antibacterial treatment plays an important role in the treatment of acute gingivitis. Relief of inflammation is carried out through irrigation, rinsing and applications using medicinal ointments and gels. If there is no positive dynamics, non-steroidal anti-inflammatory drugs are prescribed, which help relieve inflammation and get rid of symptoms.
To eliminate the source of infection, soft and hard deposits on the teeth are removed. For this purpose, ultrasonic scalers or manual curettes are used. To prevent the re-formation of plaque, which can cause gingivitis, teeth are polished using special rotating instruments followed by the use of polishing pastes.
Since improper oral hygiene has a high probability of re-developing gingivitis, the patient is taught how to care for his teeth and individual cleaning products are selected.
Treatment of chronic gingivitis
Complex therapeutic measures for chronic gingivitis include eliminating the causes of the disease and influencing pathological foci. For this, the patient is prescribed:
- local anti-inflammatory gels and ointments;
- vitamins and means to improve blood circulation in the oral cavity;
- cleaning teeth and removing deposits;
- treatment of caries and removal of decayed teeth;
- correction of bite and other anomalies that provoke the development of gingivitis;
- electrophoresis, ultraviolet irradiation, laser therapy.
Treatment of ulcerative-necrotizing gingivitis
When deciding how to cure gingivitis in the ulcerative-necrotic form, doctors focus on a combination of local and general therapeutic measures. The patient is prescribed antibiotics, immunomodulators, antiallergic and restorative drugs, and the ulcers are cleansed and treated with wound-healing agents. An obligatory point in the treatment of gingivitis is the fight against dental plaque, which includes brushing the teeth and removing deposits. After the ulcers disappear, treatment of diseased teeth is performed.
Treatment of hypertrophic gingivitis
Hypertrophic gingivitis is treated in a similar way to catarrhal gingivitis. For the fibrous form, the same methods are used as for chronic catarrhal gingivitis, and for the edematous form, methods for treating the acute catarrhal form are used. Since in many cases conservative therapy does not give the desired effect, the patient often undergoes cryodestruction of hypertrophied papillae or their diathermocoagulation. Sometimes the indication for treatment is gingivectomy - a surgical procedure during which an overgrown area of the gum is excised.
Treatment with folk remedies for gingivitis
Treatment of gum inflammation at home is only possible in conjunction with professional methods. It is impossible to completely get rid of the disease without consequences; it will return periodically. During the consultation, the periodontist may recommend rinsing the mouth with herbal solutions. The advantage of this method is that it can be used indefinitely; unlike chlorhexidine, infusions do not disrupt the composition of the normal microflora of the oral cavity.
To prepare a home remedy, dry herbs of chamomile, calendula, and oak bark are used. 2 tablespoons of the workpiece are poured into 500 ml of boiling water, the solution is kept until it reaches room temperature. After this, it can be used in unlimited quantities, ideally 3 times a day after meals.
Prevention
- maintaining oral hygiene
- to give up smoking
- using electric toothbrushes[16]
- dental gels with metronidazole, for example Metrogyl Denta
- ambazon, 2,4-dichlorobenzene alcohol, amylmetacresol in the form of lozenges
- rinsing the mouth with solutions containing chlorhexidine, hydrogen peroxide, ethanol, thymol, cineol, methyl salicylate, menthol, methylparaben, benzalkonium chloride, fluorides and xylitol. Recent scientific research has also shown the beneficial effects of mouthwashes containing essential oils[17]
- use of toothpastes with triclosan[18]
- use of calcium supplements[19]
The above preventive measures are also used for treatment. Dental floss is not advisable.[20]
Special cases of gingivitis
In some cases, the treatment of gingivitis will take into account specific conditions of the body, and treatment is prescribed based on these factors.
Teenage years
Between the ages of 10 and 17 years, children often experience gum swelling and redness. Typically, this condition is accompanied by a large amount of soft plaque on the tooth enamel. The reason is hormonal changes in the body, poor cleaning of the oral cavity, and the nature of the food eaten (sweets, starchy foods). Adolescent gingivitis goes away on its own by the age of 18 and does not require special treatment.
Pregnancy
During pregnancy, hormonal levels also change, the gums swell greatly and float over the teeth. Contrary to popular belief, women can and should remove dental plaque with ultrasound during pregnancy; this procedure does not in any way affect the health of the unborn child. After his birth, the swelling of the gums gradually disappears.
Etiology of gingivitis
Let's look at what gingivitis is. As previously noted, gingivitis is an inflammation of the gum tissue, without disruption of the dental ligament, and the formation of pathological dental-gingival pockets. The main cause of this inflammation is the microbial factor. As is known, soft and dense dental plaque contains a significant number of microorganisms, including pathogenic ones, which cause gingivitis.
In addition, changes in hormonal levels during puberty or during pregnancy, as well as taking certain medications, for example, Nifedipine, Cyclosporine, immunosuppressants, can cause changes in the gingival margin - hypertrophic gingivitis. Exposure to external damaging factors also leads to gum damage: mechanical trauma, radiation, chemical or thermal burns.
Diagnosis of ulcerative gingivitis
Diagnosis is not particularly difficult due to the very characteristic clinical course of the disease and the visible changes that occur in the patient’s oral cavity. Ulcerative gingivitis, the treatment of which requires an integrated approach, does not require special diagnostic methods, but involves examining the patient to identify common diseases.
The patient is prescribed general blood and urine tests, in which some changes in the leukocyte formula may be observed, as well as an increase in the erythrocyte sedimentation rate. It is worth noting that at the onset of the disease, clinical indicators may be normal or differ slightly from it.
A differential diagnosis of ulcerative gingivitis with necrotic lesions and inflammatory processes that occur in the gums with various autoimmune diseases and HIV infection is required.
Treatment
The course of therapy consists of the following stages:
- cleansing _ Cleaning your mouth of bacteria is the first stage of treatment. Plaque is removed from tooth enamel;
- anti-inflammatory method . Rinsing eliminates bacteria and dirt. This procedure is carried out every time after eating. The following agents are used for rinsing: Furacilin, Chlorhexidine and Furamistin. Herbal remedies are also used: tincture of chamomile, calendula, arnica flowers, and so on;
- repeated inspection . After the symptoms have reduced, thanks to the above therapy, the doctor re-examines the oral cavity. If necessary, prescribe one of the courses of treatment;
- surgical interventions . If there are necrotic areas on the gums, then surgical intervention is performed. This method of therapy is also appropriate for hypertrophic gingivitis;
- orthodontist _ If after an illness there are signs of deformation of the dentition, in this case treatment by a specialized orthodontist is recommended.
Treatment of necrotizing gingivitis involves taking antihistamines and a diet rich in easily digestible protein. Doctors also prescribe vitamins and immune-supporting medications.