Why does the disease occur?
People first started talking about this pathology 150 years ago; during this period, erosive changes in the oral mucosa, localized at the border of the soft and hard palate, were considered a disease of the poor. At that time, the causes of this disease in children were considered to be malnutrition, environmental problems, and poor oral hygiene. Over time, Bednar's aphthae began to be viewed as a consequence of traumatic injury to the oral mucosa with subsequent infection.
There are not many reasons for the appearance of aphthae in infants:
- traumatic factor during breastfeeding (in particular, the mother’s hardened nipple);
- consequence of trauma during childbirth;
- inappropriate size of pacifiers;
- frequent use of non-orthodontic pacifiers.
In older children, aphthae in the oral cavity occurs:
- in case of violation of basic rules of personal hygiene;
- against the background of an unbalanced diet, poor nutrition;
- Often the causes of the disease are hormonal imbalance and vitamin deficiency;
- some children suffer from the bad habit of biting their nails or putting foreign objects into their mouths, causing infection with them;
- in case of immune failure.
Using dirty pacifiers, toys, and the habit of putting your fingers in your mouth are common causes of ulcers on the oral mucosa.
Important! Some doctors associate the appearance of Bednar's aphthae in the mouth with congenital heart disease.
Afty Bednar
In children in the first months of life, traumatic erosions on the palate are observed, known as Bednar's aft. Bednar's aphthae most often occur in weakened children who are bottle-fed, suffer from congenital heart defects, or have suffered from any illness in the first months of life.
Hypotrophy is the background against which minor tissue trauma by a long horn or while wiping the child’s mouth is sufficient to disrupt the epithelial cover. Clinic
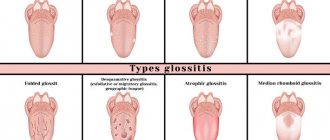
Erosions are often located symmetrically at the border of the hard and soft palate, respectively, projecting onto the mucous membrane of the hook of the pterygoid process of the main bone. The defeat can also be one-sided. The shape of the erosions is round, less often oval, the boundaries are clear, the surrounding mucous membrane is slightly hyperemic, which indicates a state of hypergia. The surface of the erosions is covered with a loose fibrinous coating, sometimes clear, brighter in color than the surrounding mucous membrane of the palate.
The size of the erosions ranges from a few millimeters to extensive lesions that merge with each other and form a butterfly-shaped lesion. When a secondary infection occurs, erosions can turn into ulcers and even cause perforation of the palate. Bednar's aphthae can also occur in children who are breastfeeding if the mother's nipple is very rough, for example after irradiation with quartz. Erosion in this case is located along the midline of the palate.
The child becomes restless. Having started to actively suck, he stops sucking after a few seconds with crying, which is usually the reason for contacting a doctor. Treatment of traumatic injuries comes down to eliminating the cause. Prematurely erupted baby teeth should be removed because their structure is defective. They quickly wear off and, in addition to trauma to the mucous membrane, can cause odontogenic infection. When removing such teeth, you should be aware of the possibility of heavy bleeding. With Bednar's aphthae, it is necessary, first of all, to establish feeding of the child: natural through a pad (if the mother's nipples are rough) or artificial through a short horn made of hard rubber, which would not stretch out when sucking and would not reach the eroded surface.
To treat the oral cavity of a child suffering from canker sores, weak antiseptic solutions (0.25% chloramine solution, 3% hydrogen peroxide solution) should be used; vigorous wiping of the mouth and the use of cauterizing substances are unacceptable.
It should be borne in mind that Bednar's aphthae heal very slowly - over several weeks or even months. Thermal injuries in children are rare, but are possible when eating hot food, especially milk and broth.
The mucous membrane of the lips, the tip of the tongue, and the anterior part of the hard palate is mainly affected. It becomes swollen, hyperemic, and painful when touched. Less commonly, superficial intraepithelial vesicles form, which immediately burst. Upon examination in this case, fragments of white epithelium are visible on a hyperemic base.
“Childhood Dentistry”, A.A. Kolesov
Lesions of the oral mucosa associated with taking drugs
Many medicinal substances, including antibiotics, sulfonamides, pyramidone, heavy metal salts, novocaine, iodine, phenol, etc. can cause side effects, which are collectively called “drug disease”. In 17% of patients, it also manifests itself in the oral cavity. The pathogenesis of such stomatitis can be different. The toxic effect of drugs is due to their chemical structure. Thus, streptomycin causes damage to the auditory...
Hypovitaminosis
Often, various diseases in children are accompanied by metabolic disorders, including disturbances in the metabolism of vitamins, which leads to their deficiency. Nutritional hypovitaminosis is currently rare and manifests itself mainly with a monotonous dietary diet. Polyhypovitaminosis usually occurs, but there are diseases in which deficiency of any one or group of vitamins predominates. Metabolic disorders associated with...
Endocrine diseases
Endocrine diseases in children lead to disruption of many vital functions, and against this background, some changes are detected in the oral mucosa. In diabetes mellitus, in addition to the characteristic periodontopathies, dryness, a burning sensation and bright hyperemia of the mucous membrane of the lips, cheeks and especially the tongue are noted. With myxedema, the mucous membrane is pale, significant swelling causes the appearance of deep tooth marks on...
Cardiovascular diseases
In case of cardiovascular diseases, the condition of the oral cavity largely depends on the compensation of existing circulatory disorders. With severe hypoxia, the mucous membrane and lips are cyanotic; with congestion in the systemic circulation, swelling of the oral mucosa is pronounced. Particularly severe lesions occur in cases of circulatory failure of II-III degree. A sharp disruption of tissue trophism in such children leads to the development of severe...
Blood diseases
With impaired erythropoiesis and the development of various types of anemia, the mucous membrane of the oral cavity, especially the tongue and gums, is very pale. No other characteristic changes are observed in children, but all diseases of the mucous membrane caused by another cause have a sluggish, long-term course. In case of impaired leukopoiesis, acute and chronic leukemia in most children at different periods of the development of the disease, especially with ...
Development mechanism
How to treat aphthous stomatitis in children
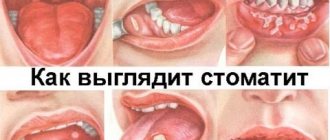
Children's oral mucosa is extremely sensitive to any aggressive influence of external aggressive factors. Any mechanical irritation can become a trigger that will lead to the appearance of ulcers. Thus, the affected cells are slowly restored, as a result of which numerous erosions (aphthae) form on the mucous membrane.
It is noteworthy that with a prolonged course (no treatment), a secondary infection can join the ulcers. In this case, the bottom of the aphthae becomes covered with white fibrin, and then with a thick yellow coating. The area of the ulcerative lesion naturally increases, and the regeneration process slows down even more.
Symptoms and diagnosis
The classic manifestation of the disease (shown in the photo above) is ulcerative formations on the oral mucosa, which are “attached” to the border of the soft and hard palate. The aphthae have a characteristic oval shape and are located symmetrically in relation to each other. The affected areas are covered with a dense yellow coating.
If a child’s immune system is weakened, such formations can significantly increase in size, acquire an irregular shape, and occupy almost the entire palate. In this case, the growth of aphthae is accompanied by the appearance of a pronounced pain syndrome - the child becomes whiny, restless, and the treatment process is complicated.
Timely seeking help from a dentist will not only detect the disease, but also prevent it from becoming chronic.
The appropriate diagnosis is made by a pediatrician based on an analysis of the clinical picture of the disease; if necessary, a smear is taken from the mucous membrane (to determine the type of bacterial infection).
Important! Without fail, a specialist differentiates the disease from aphthous stomatitis, a common childhood disease in which erosions are located in the vestibule of the oral cavity.
Diagnosis and treatment of Bednar's aphthae
When diagnosing, the main role is played by anamnesis and objective examination. The diagnosis is made based on the characteristic clinical picture. Bednar's aphtha has similar symptoms to chronic recurrent aphthous stomatitis. However, the latter, as a rule, develops in older children, has no relationship with a traumatic factor, and the lesions are located in the vestibule of the oral cavity. It is also necessary to carry out differential diagnosis with such infectious diseases as herpetic sore throat, diphtheria of the pharynx, tuberculosis and syphilis. In order to clarify the diagnosis, a laboratory examination of a smear from erosion and serodiagnosis are carried out.
The main goal of treatment is to eliminate the traumatic factor. When breastfeeding, it is recommended to use special breast pads to prevent contact of the oral mucosa with the rough skin of the nipple. For artificial feeding, you need to choose the right nipple - it should not be too long or hard.
Drug treatment includes sequential treatment of the oral cavity. The first stage is the cleansing of erosive surfaces from plaque using artificial lysozyme and proteolytic enzymes (trypsin, chymotrypsin). Then the mucous membrane is treated with local antiseptics and herbal decoctions (chamomile, sage, St. John's wort) to prevent infection and keratoplastics (rosehip oil, sea buckthorn) to accelerate regeneration. To reduce pain, you can use local anesthetics (anesthetic ointment, lidocaine).
How to deal with the disease
The main problem in treating Bednar's aphthae is that long-term medication is required for visible improvement. In general, treatment of the disease takes place in several successive stages:
- affected areas of the mucous membrane are treated with solutions of Trypsin and Lysozyme;
- compresses are recommended for infants, and rinsing the mouth with decoctions of medicinal plants (St. John's wort, chamomile, sage) for older children.
- The resulting ulcers are lubricated with sea buckthorn oil and Solcoseryl.
- If there is pain, patients are prescribed systemic painkillers (Kamistad).
The described actions are repeated for several days in a row, after which the child is re-examined by a specialist. It is noteworthy that the duration of the course of treatment can range from several days to 2 weeks - it all depends on the characteristics of the baby’s immune system, the reaction of his body to certain drugs, and the degree of damage to the mucous membrane by aphthae.
Obviously, eliminating the traumatic factor is of no small importance. If the child continues to use dirty pacifiers, toys, or put foreign objects in his mouth, no drug treatment will lead to the expected result.
To avoid the addition of a bacterial infection, erosive lesions of the mucous membrane are treated with local antiseptics so that the cells regenerate faster - they are lubricated with keratoplastic compounds
Possible complications and prognosis
If you seek medical help in a timely manner, drug control against Bednar's aphthae in most cases leads to a complete cure. In another situation, this pathology can develop into a chronic recurrent form; ulcers on the palate will bother the baby several times a year with the slightest traumatic injury to the oral mucosa. In addition, ulcers are the “entry gate” for any infections. Accordingly, if they are not treated in time, the child may become a “victim” of sore throat, diphtheria and many other infectious diseases.
Prevention
To prevent the appearance of Bednar's afte on the oral mucosa, it is necessary to strictly observe the rules of personal hygiene of the child, monitor the cleanliness of pacifiers and toys. Young mothers should carefully monitor the condition of the skin of the nipple (during breastfeeding) - it can become rough as a result of certain physiotherapeutic procedures and become a traumatic factor that will contribute to the formation of ulcers on the baby’s mucous membrane.
Older children should once and for all get rid of the bad habit of biting their nails and putting foreign objects into their mouths. To strengthen the immune system, you should take vitamin and mineral complexes every six months (as recommended by your doctor).
Forecast and prevention of Bednar's aphthae
With timely treatment, the prognosis of the disease is favorable. However, healing of erosive defects can take several weeks or even months, preventing normal feeding and the supply of nutrients to the body in the required volume. Careful pediatric monitoring is required here.
Prevention of neonatal aphtha involves educational work among parents. It is necessary to choose the right pacifier, carefully follow the rules of breastfeeding and artificial feeding, treat the mammary glands in a timely manner and prevent the skin of the nipples from becoming rough. In older children, it is important to carefully monitor their behavior and prevent them from developing the habit of putting foreign objects in their mouth.