A common problem with which patients go to medical institutions is inflammation of the cheek on the inside. At first glance, this problem may seem trivial and does not require help. In fact, this is not true, there can be many reasons for swelling in the mouth, and ignoring the symptoms can lead to serious complications.
Many people believe that teeth are the only cause of cheek inflammation. But there are many reasons for the occurrence of this disease; below we will consider them all in detail.
Dental causes of inflammation
Regarding the occurrence of swelling from the teeth, there are several problems in the mouth that can provoke it:
- removal of a tooth;
- gum disease;
- cutting through the figure eight;
- periodontitis.
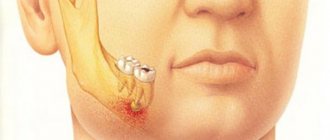
One of the reasons is infection of the tooth root and bone. This complication occurs when the nerves are removed, but the canals are not washed and cleaned well enough. As a result, pathogenic microorganisms remain in the pulp chamber and inflammation appears. Usually this pathology is sluggish, but when the immune system is weakened, the inflammatory process actively progresses and spreads to the bone, gum, and cheek. Popularly this is called gumboil. Failure to provide assistance in this situation can have serious consequences (development of phlegmon, sepsis).
Another factor that provokes inflammation of the oral cavity is the eruption of the impacted figure eight.
Swelling also appears after tooth extraction. This most often occurs after intervention on the lower jaw.
The cheek can also become inflamed due to gum pathology, such as periodontitis, gingivitis. These two problems arise in most cases in the presence of dental plaque. Stones and plaque accumulate pathogens that provoke tooth inflammation. In a more advanced form, they can cause periodontal disease.
Why is it necessary to treat a scar?
Mucosal tissue recovers much easier and faster than the epithelium on the skin. Therefore, the postoperative scar on the gum in most cases heals imperceptibly and practically without traces. If a granuloma or lump has formed near a tooth, a noticeable scar may remain. You should immediately contact your dentist or therapist if alarming symptoms appear:
- temperature rises to 38–40°;
- the gums swell, itch and burn;
- a tugging pain appears inside the roots of the teeth;
- the seal turns white and may acquire a yellow tint.
These are signs of accumulation of pus and exudate in periodontal tissues. It can enter the body through the circulatory or lymphatic system and accumulate in the kidneys, liver or heart. The problem is fraught with sepsis or inflammation of internal organs.
Infectious and colds
The cause of the changes may be an infectious disease such as mumps. This pathology is characterized by inflammation of one or more salivary glands, which causes swelling.
Lymphadenitis can also provoke inflammation of the cheek. In this condition, the cervical, parotid and submandibular lymph nodes become enlarged. This can be an independent illness, triggered by an infection, but most often it occurs as a complication after illnesses in the ENT organs (reactive lymphadenitis).
A pathology such as sinusitis can also cause swelling. The inflammation usually spreads to the cheek and under the eye.
This also includes infectious mononucleosis, diphtheria, tuberculosis, but these diseases are very rare.
Oral fissure.
A fissure is a gap-like defect in the epithelium (epidermis) lining the tongue, lips and skin around the mouth. The presence of a crack is not only a sign of pathology, but can also be a normal variant. Natural cracks, such as in a folded tongue, can become inflamed when food debris and pathogenic microorganisms stagnate in them, which is also facilitated by dry mouth and dehydration. Examples of pathological cracks include cracks in angular and exfoliative cheilitis.
Various surgical manipulations on the mucous membrane are carried out quite often in dental practice. After removing pus or an inflamed root, sometimes a scar remains on the gum. Normally, after a few weeks it should resolve and become completely invisible. But there are situations in which the tissue becomes denser, causing a feeling of stretching and discomfort.
Disease of the salivary glands and nerves
Most often, inflammation of the salivary ducts and glands occurs as a result of a pathological process on the gums. But it could also be a separate disease. The cause is stones in the ducts, various neoplasms in the system (cysts, tumors).
Swelling of the mucous membrane also occurs due to inflammation of the nerves. In this case, numbness, “lumbago”, and pain radiating to the ear may be bothersome.
In both the first and second cases, there will be clearly defined hyperemia along the nerve or salivary duct.
Types of Scar Tissue
There are two main types of scars: hypertrophic and keloid. The first ones are slightly increased in size, but gradually “deflate” and cause practically no discomfort to the patient. Over time, they resolve and become noticeably pale. The second type is considered more problematic for humans. Its characteristic features:
- a dense white scar appears on the gum, which can follow the outline of the seam;
- a person feels constant squeezing or stretching;
- Some patients lose sensitivity at the incision site;
- The color of the scar may change to dark red or bluish.
If such tissue has formed during the healing process, it may contain very thin capillaries. Sometimes the area bleeds and becomes very painful when brushed with a toothbrush or touched with the tongue. If after removal of the fistula or drainage there is a deep scar in the gum, the photo will resemble a small dense tumor. If you do not treat this problem, the scar will turn into a painful atrophic one and it will be too difficult to remove it.
Other pathologies
Not least in terms of frequency of occurrence is traumatization. Swelling can cause soft tissue bruises, joint dislocations, and jaw fractures.
Inflammation can cause various types of allergic manifestations, if the body is immune to a certain product. One of the most striking examples is stomatitis; it affects the tongue, gums, and cheeks.
More rare, but the most dangerous, are tumors of the oral mucosa. This disease certainly cannot be ignored.
How to remove a scar on a gum
If a serious complication begins, the dentist has to re-open the painful scar. He removes all granular tissue, leaving drainage for several days to remove ichor and pus. To relieve the burning sensation, a person can take painkillers such as Nurofen, Ibuklin or Ketanov. To prevent the infection from spreading further, treatment is supplemented with antibiotics against streptococci and staphylococci:
- Lincomycin;
- Doxycycline;
- Clarithromycin;
- Sulceph.
If the situation threatens to damage the jaw bone, an antibiotic is injected into the gums. The patient must follow all the specialist’s recommendations and properly care for the oral cavity during the healing period:
- rinse the mucous membranes daily with antiseptic solutions (Malavit, Chlorhexidine or Furacilin);
- treat the scar on the gum with wound-healing ointments Solcoseryl or Metrogyl Denta, an alcohol solution of Ingalipt;
- wipe the seam with hydrogen peroxide;
- Apply a cotton swab dipped in aloe juice and sea buckthorn oil to the wound.
We invite you to familiarize yourself with Inflammation under the tongue: causes, treatment of inflammation of the gland under the tongue
At home, it is recommended to supplement the treatment with simple folk recipes. In the evening, the affected area can be rinsed with a warm decoction of chamomile, calendula and sage. A good anti-inflammatory effect is provided by propolis tincture, which dries the seam and helps it heal faster.
Symptoms of cheek inflammation
Depending on the etiology, the complex of symptoms may vary somewhat. The main thing that all diseases have in common is:
- swelling on the cheek;
- inflammation of the mucous membrane in the oral cavity;
- violation of facial movements;
- pain in the area of pathology.
It is simply impossible not to notice such symptoms; the disease cannot be ignored. The reason to fly to the doctor urgently is the presence of the following signs:
- fever;
- general weakness;
- loss of appetite;
- bad breath;
- numbness and sagging of the cheek;
- a sharp increase and pain of the tumor;
- toothache, especially when chewing;
- purulent discharge from the gums;
- difficulty opening the mouth.
Granuloma in the scar on the gum
Sometimes a small lump appears at the surgical site. The patient feels its mobility well and can move it by pressing the tongue. The scar on the gum seems to rise from the inside and resembles a convex tubercle. These are symptoms of a serious complication - granulomas. The disease causes various bacteria and microorganisms to enter the wound. The reasons are always related to poor hygiene:
- the patient did not properly treat the oral cavity after applying and removing sutures;
- the dentist used unsterile instruments or threads.
We invite you to familiarize yourself with Laryngeal cancer.
Causes, symptoms, diagnosis and treatment of the disease The granuloma on the gum itself consists of phagocyte cells that surround the site of infection, preventing it from spreading to neighboring tissues. It occurs more often in people who have viral or bacterial diseases, rheumatism, tuberculosis or syphilis.
Causes of pathology
Basically, stomatitis on the inside of the cheek is caused by the following factors.
- Pathogenic microorganisms. Ulcers occur at the site of penetration of bacteria, viruses, fungi and other harmful microorganisms into microcracks in the mucous membrane. In fact, opportunistic flora is always present inside a person’s mouth, but manifests itself only in the presence of favorable conditions (reduced immunity, damage to mucous tissues, exacerbation of systemic diseases, etc.).\
- Diet. An unbalanced menu leads to a deficiency of vitamins, minerals and antioxidants, which increases the risk of microbial growth.
- Oral injuries. Any violation of the integrity of the mucous membrane (burn, rough food, hard bristles of a toothbrush, household item, tooth fragment, etc.) increases the risk of ulcer formation.
- Violation of hygiene rules. Insufficient care of teeth and gums, poor cleaning and processing of products, poor hand washing, etc. can also increase the risk of stomatitis on the cheek.
In this case, pathology can also be caused by too intensive brushing of teeth, the use of pastes with sodium lauryl sulfate, as a result of which the production of saliva, a natural antiseptic of the oral cavity, is disrupted.Most often this cause is present in children.
- Dental manipulations. It has been noted that the disease develops more often in patients who have recently had braces, dentures, plates, mouth guards or implants installed.
- Taking medications. Some drugs (for example, diuretics) disrupt the natural microflora of the mucous membrane and lead to the proliferation of opportunistic microflora. They can also reduce salivation and increase dryness of the buccal mucosa, which will lead to the appearance of microcracks.
- Bad habits. Alcohol and smoking lead to disruption of tissue trophism, chemical and thermal burns of the mucous membrane, which reduces local immunity.
- Systemic diseases in acute and chronic form. Any diseases, especially those associated with ENT organs (tonsillitis, tonsillitis, etc.) lead to weakened immunity and an increased risk of secondary infection.
- Malignant processes of ENT organs . Often, patients with cancer pathologies develop stomatitis in parallel.
- Ionizing radiation, chemotherapy, radiation sickness. As a result of these processes, the immune system is greatly weakened and tissues become thinner; this is one of the causes of stomatitis in the mouth.
- Parasites. In rare cases, parasitic infestation in advanced form can also cause ulcers on mucous surfaces.
- Dehydration. Against the backdrop of a prolonged lack of fluid, the mucous membranes dry out, which provides soil for the proliferation of pathogens.
- HIV infections. In patients with HIV and AIDS, the risk of candidiasis, herpes and stomatitis increases significantly.
- Endocrine pathologies. When hormonal imbalances occur (including during pregnancy or menopause), ulcerative lesions occur more often. Pathology can also be triggered by treatment with aerosol hormonal drugs, for example, for bronchial asthma.
- Diabetes. People with an advanced form of the disease or poor compensation often develop a complication in the form of aphthous stomatitis.
- Anemia. Disturbances in blood flow and blood structure can also provoke autoimmune forms of stomatitis on the buccal mucosa.
Photo - aphthous stomatitis inside the cheek
The mechanism of formation of bubbles in the mouth
A blister on the inside of the cheek is a hematoma, or bruise. It is a small, from a few millimeters to a couple of centimeters, rounded formation. The internal exudate is serous or bloody, depending on the extent of the injury. In the first case, the blister is gray-white, in the second it is red, with a possible bluish tint.
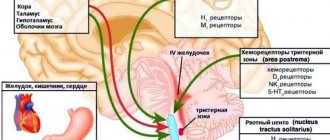
Blood blisters appear due to injuries to the mucous membrane. Their formation is a natural reaction of the immune system to an irritant. It consists in:
- Activation of the body's defense mechanisms in response to an irritant. Agranulocytes arrive at the site of the lesion: leukocytes and monocytes. The latter, when leaving the blood into the tissues, are converted into macrophages. These cells capture the pathogen, neutralize it, and then die.
- The death of agranulocytes leads to their release to the site of injury. This process is a signal of injury to the body. After which it begins to release histamine, bradykinin and serotonin into the affected area. They sharply increase the permeability of blood vessels.
- A spasm occurs at the site of injury. The blood flow becomes difficult, after which the vessels relax and the blood accumulated during the narrowing enters the injured area. It moves quickly and under pressure. As a result, the upper layer of the epithelium peels off and a blister filled with bloody contents forms.
Blood blisters appear due to injuries to the mucous membrane.
Important! The red or white growth is not dangerous. It is virtually painless and heals within a week. The only discomfort is associated with inconvenience when chewing and talking.
Types of stomatitis on the cheek
The disease is a kind of protective reaction of the immune system to various irritants (infection, allergen, virus, bacteria, fungus, etc.). The provoking factor may be the region of residence (poor ecology, water), chronic and systemic diseases (reduce immunity), autoimmune processes (attack by lymphocytes of the body’s own cells), etc.
Depending on the causes of occurrence, the following types of stomatitis on the cheek are distinguished.
- Mechanical or traumatic. Wounds are formed as a result of damage to the mucous surface (biting, bruising, blow, cut, puncture). Often, the sore develops after a trip to the dentist, when, under the influence of anesthesia, the patient (most often a child) unknowingly chews the inside of the cheek, which leads to multiple injuries on the inside of the cheek. Sometimes wounds are caused by fragments of teeth after a filling, as well as against the background of untreated caries or malocclusion. Mechanical stomatitis also includes one that was caused by a chemical burn: mouthwash concentrate, specific food or drinks, etc. Ulcers can also be the result of a thermal burn: eating too hot or cold food, damage to the mucous membrane under the influence of cigarette or hookah smoke . Small children can injure the mucous membranes with uneven edges of objects and toys that are pulled into the mouth.
- Fungal (candida). Ulcerative processes on the cheeks can be the result of the activity of fungi of the genus Candida, which often occurs against the background of decreased immunity, as well as in case of abuse of sweet carbohydrate foods. Diabetics and patients undergoing antibiotic treatment are at risk for candidal stomatitis. Candidal stomatitis also often occurs in children with infection from the mother. (see photo below)
- Aphthous. The pathogenesis of this species has not yet been studied. There is an assumption that the provoking factor is an adenovirus or autoimmune processes.
- Herpetic. It occurs against the background of the herpes virus, which is very volatile and is easily transmitted by airborne droplets. Also, this virus lives in the body of every person and is activated when immunity decreases.
- Bacterial. The culprits of this type of stomatitis are streptococci and staphylococci, which penetrate the mucous membrane through wounds or scratches. The likelihood of infection always increases with weak immunity.
- Enteroviral stomatitis. A specific type of disease that is caused by an enterovirus, transmitted through food, household items and water.
- Allergic. In this case, stomatitis on the cheek occurs due to an autoimmune reaction when the body perceives histamine as a foreign agent.
Photo-candidal stomatitis on the cheek
Video:
My mouth is full of trouble: stomatitis. Live healthy! 08/06/2018