Traumatic factor
Blood from the tonsils is observed after exposure of the mucous membrane to chemicals, after which ulcerative defects form on the surface. The wounds are formed quite deep and widespread. It is not always possible to wash away the chemical with water, so the doctor carries out procedures to neutralize the chemical reaction.
When going to the hospital, the patient should indicate the type of chemical agent, which will greatly facilitate the provision of care and prevent serious complications.
The healing process of wounds takes a long time, so the tonsils may sometimes bleed.
In case of a thermal burn, gargle with warm water.
Cold water is contraindicated for thermal burns, as bubbles appear, which, when opened, can cause bleeding wounds.
Mechanical trauma can lead to damage to larger vessels with the development of bleeding. If the injury was caused by a sharp object that damaged the tonsil, if possible, you should not remove it from the tonsil yourself - this will increase the bleeding. In this case, you need to wait for the ambulance team.
Day of surgery
The doctor decides how exactly the operation will take place. Typically, the entire tonsils are removed. Partial tonsillectomy can be performed in cases of severe hypertrophy of lymphoid tissue.
6 hours before the procedure, the patient is asked to stop eating, drinking dairy products and juices. You can’t even drink water for 4 hours.
Tonsil removal in adults is usually performed under local anesthesia. Half an hour before surgery, the patient is given an intramuscular injection with a sedative, then an anesthetic, lidocaine, is injected into the tissue around the tonsil.
In the operating room, the patient is seated in a chair. Inflamed organs are removed through the mouth. No incisions are made on the neck or chin.
Tonsillectomy options:
Traditional operation. Tonsils are removed using traditional surgical instruments - scissors, scalpel and snare.
Pros: the method is time-tested and well proven.
Cons: long rehabilitation period.
Infrared laser surgery. Lymphoid tissue is excised with a laser.
Pros: almost complete absence of swelling and pain after the procedure, ease of implementation, the operation can be performed even on an outpatient basis.
Cons: there is a risk of burns to healthy tissue surrounding the tonsil.
Using an ultrasonic scalpel. Ultrasound heats the tissue to 80 degrees and cuts off the tonsils along with the capsule.
Pros: minimal damage to adjacent tissues, rapid healing.
Cons: there is a risk of bleeding after surgery.
Bipolar radiofrequency ablation (collaboration). The tonsils are cut off with a cold radio knife, without heating the tissue. The technology allows you to remove the entire tonsil or just part of it.
Pros: no pain after surgery, short recovery period, low complication rate.
Cons: performed only under general anesthesia.
The entire operation takes no more than 30 minutes. After its completion, the patient is taken to the ward, where he is placed on his right side. An ice pack is applied to the neck. You are asked to spit saliva into a special container or onto a diaper. During the day (and during collocation - no more than 5 hours), the patient is not allowed to eat, drink or gargle. If you are very thirsty, you can take a few sips of cool water.
Frequent complaints after surgery are sore throat, nausea, dizziness. Sometimes bleeding may occur.
Depending on the method of tonsillectomy, the patient is discharged home on days 2–10. Sore throat persists for 10–14 days. On the 5th–7th day it sharply intensifies, which is associated with the removal of crusts from the walls of the pharynx. Then gradually the pain disappears.
To relieve suffering, the patient is given intramuscular injections of analgesics. Antibiotics are indicated for several days after surgery.
Infectious causes
Most often, the tonsils are affected by an infectious factor, which leads to their bleeding. Diphtheria is an infectious disease caused by the Lefller bacillus. After infection, the rods multiply and release toxins. Externally, this is manifested by the appearance of a yellow coating on the surface of the tonsils in the form of films.
Catarrhal symptoms develop quickly, the person is worried about malaise, hectic hyperthermia, pain in the throat and difficulty swallowing. The tonsils become swollen and increase in volume. Regional lymph nodes become somewhat denser, enlarged and painful on palpation.
The danger of diphtheria lies in the high risk of covering the surface of the trachea and bronchi with a fibrin film, which can lead to asphyxia due to obstruction of the lumen of the respiratory tract.
The person notices a hoarseness of voice, a rough cough gives way to a barking, then a silent cough. Noisy breathing can be heard remotely. When trying to remove the film from the tonsil, blood may bleed. In this regard, it is not recommended to remove plaque yourself.
Tonsillitis develops acutely with the appearance of severe pain in the throat, fever and malaise. There are several types of pathology. With catarrhal, lacunar or follicular forms, bleeding is not observed. Even when opening small abscesses, the appearance of blood is not observed.
The cause of sore throat is pathogenic microbes, mainly of the streptococcal type. When pathogenic microorganisms penetrate the tonsils, the disease usually does not develop. However, when negative factors influence the body, which lead to immunodeficiency (general hypothermia, exacerbation of chronic diseases), microbes are activated.
Sore throats often occur in people with chronic sinusitis, pharyngitis and neglected carious teeth, as infectious pathogens accumulate in them.
Sore throat is a contagious disease, so in the acute period you should avoid contact with other people, especially children, or use protective equipment (mask, separate utensils).
Primary tonsillitis develops immediately after infection and activation of streptococcal microorganisms.
| Form of tonsillitis | Clinical symptoms |
| Fibrinous-membranous (diphtheroid) | This form of sore throat is characterized by the appearance of a yellowish filmy coating on the surface of the tonsils. Regional lymph nodes enlarge, become denser and painful when palpated. The fibrinous-membranous course of the disease is observed during the transition from the lacunar form or as an independent type with the appearance of a film in the first hours of the disease. The person notes an acute onset, febrile hyperthermia, severe chills and severe symptoms of intoxication. |
| Phlegmonous with the formation of intratonsillar abscess | It is quite rare; unilateral lesions are often recorded. The occurrence of an abscess is associated with purulent melting of the tonsil tissue. It is enlarged in volume, with a tense surface, and is sharply painful when touched. Regional lymph nodes are enlarged and cause sharp pain when palpated. A person is also worried about severe pain in the throat, hectic hyperthermia, headache and severe signs of intoxication. The tonsil may burst with a significant increase in purulent contents. If a tonsil bursts and bleeding occurs, you should immediately consult a doctor. Pharyngoscopy reveals an asymmetric pharynx (displacement of the uvula and tonsils to the healthy side). The mobility of the soft palate is sharply limited. |
| Necrotic | Intoxication is pronounced. The patient complains of hectic fever that cannot be reduced, dizziness, confusion, drowsiness, vomiting and headache. The affected areas of the tonsils are covered with an uneven, dull, gray-green coating that extends to the posterior pharyngeal wall. When the films are impregnated with fibrin, they become dense, and after their removal a bleeding wound remains. When necrotic tissue is rejected, a defect with uneven edges, bottom and a diameter of up to 2 cm remains. |
| Ulcerative film | Symptomatically, the disease is manifested by discomfort in the pharynx, difficulty swallowing, the presence of a foreign object in the throat, increased salivation and a putrid odor. Necrotic masses with an ulcerative defect appear on the tonsil. Regional lymph nodes are enlarged on one side. The temperature remains normal. |
In addition, the tonsils can bleed during secondary tonsillitis, when damage to the tonsils occurs as a complication of the underlying disease. Such diseases include syphilis with the formation of erosion on the tonsil, tularemia with fibrinous films that are difficult to separate, leukemia with sloughing plaques and enteroviral infection with ulcerative lesions of the tonsils.
It is no secret that in the autumn-winter period people often suffer from upper respiratory tract diseases. However, a common cold can cause very serious throat problems. If treatment is not started in time, one of the complications may be severe inflammation of the tonsils, accompanied by the release of blood from these organs. What to do if your throat is very inflamed and your tonsils are bleeding? Firstly, do not panic, because blood on the tonsils is not a death sentence. And secondly, immediately contact a doctor to find out the causes of such symptoms, make a diagnosis and prescribe the correct course of treatment.
Important! Under no circumstances should you self-medicate, seek help from traditional healers, or hope that everything will go away on its own. Diseases in which blood discharge from the tonsils is observed require proper comprehensive treatment.
Reasons for the appearance of blood on the tonsils IMPORTANT TO KNOW!
The only remedy for phlegm that is truly effective and helps almost immediately
At first glance, it seems that respiratory diseases do not pose a particular danger and are easily treatable, but in fact, even a common cold can cause complications. As a rule, the main “blow” falls on the tonsils - an inflammatory process begins in them, which is accompanied by pain and discomfort in the throat. In rare cases, bloody discharge is observed when coughing or visual examination of the oral cavity. If you notice that your tonsils are bleeding, you should immediately consult an otolaryngologist.
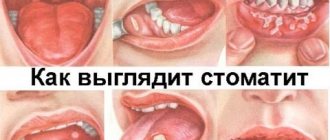
Symptoms of tonsillitis
Black tonsils may indicate the development of purulent tonsillitis, which, in turn, has several forms:
• Lacunar – with the appearance of purulent contents and plaque.
• Follicular – in which the follicles become inflamed. They also begin to form pus.
• Fibrinous, when white-yellow purulent islands form on the tonsils themselves and next to them, quickly merging into a film.
• Phlegmous with the formation of a purulent abscess.
• Ulcerative-necrotic, characterized by the formation of a black-green plaque.
The last form is an extreme one, when angina can lead to the formation of cysts with hemorrhagic contents.
There are cases when these cysts become the cause of malignant tumors. To prevent this from happening, the disease must be treated in time.
In addition, the appearance of ulcers can lead to surgery to remove the tonsils. Only then will the upper respiratory tract be more susceptible to infections.
A serious consequence is the development of phlegmon of the throat with subsequent blood poisoning. Photos of a sore throat are presented in the article.
Why do tonsils bleed?
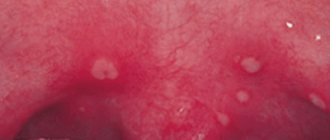
The tonsils consist of rather delicate lymphoid tissue, which has a pink color and a smooth surface. They are quite easy to damage, which will subsequently lead to inflammation and bleeding - this can be triggered by traumatic factors or advanced infectious diseases. Traumatic factors include:
- Exposure to chemicals. They cause an ulcerative defect on the mucous membrane, resulting in the formation of rather large and deep wounds. Before starting treatment, the doctor must neutralize the chemical reaction, otherwise the lesions will increase in size.
- Thermal burn. The thermal effect itself will not provoke bleeding, but if the patient decides to neutralize the effects with cold water, blisters will appear, after opening which may cause bleeding from the tonsils.
- Mechanical injury. Most often, the tonsils are damaged by solid food and sharp objects, incl. fish bone. The tonsils begin to bleed only in the case of a deep injury in which large vessels are affected. It is not recommended to remove the object from the organ yourself - you need to wait for an ambulance.
As for infectious diseases, the appearance of bloody discharge from the tonsils is often associated with diphtheria. It is provoked by the Lefller bacillus, which, when it enters the body, begins to actively multiply and produce toxins, as evidenced by yellow plaque on the tonsils. If left untreated, a fibrin film forms on the tonsils, and when removed, bloody discharge is visible.
Most often, blood appears on the tonsils in advanced forms of angina:
- Dephtheroid or fibrous film. It is characterized by the appearance of a yellow filmy plaque and enlarged lymph nodes, which become painful and dense.
- Phlegmonous with abscess formation. This form of the disease is extremely rare. An abscess is formed due to purulent melting of the tissue of one of the tonsils. The amount of purulent contents gradually increases, so the tonsil also increases in size, and under certain circumstances it will burst.
- Necrotic. With this type of angina, severe intoxication of the whole body is observed, which is accompanied by fever, high temperature that cannot be reduced, headache, dizziness and vomiting. Upon visual inspection, a gray-green film is visible, when removed, blood flows from the tonsil.
Having discovered any formations on the tonsils, you should not rush to eliminate them yourself, because there is a high probability that such manipulations will provoke bleeding.
Diagnosis and treatment
To establish the correct diagnosis, it is necessary to conduct tests and examine the patient. First of all, the doctor examines the oropharynx using a pharyngoscope, then, by palpation, determines the condition of the lymph nodes.
When the tonsils bleed, the reasons often lie in infection, and to determine its type it is necessary to take a smear from their surface.
Additionally, you need to examine your urine and blood - in case of exacerbation, the analysis will reveal an increased ESR and an increased number of leukocytes. After clarifying the full clinical picture, the doctor will prescribe appropriate therapy.
Treatment must be comprehensive, because it is necessary not only to eliminate the symptoms, but also to get rid of the root cause of the pathology. Since the disease is caused by an infection, a course of antibiotics is prescribed to combat it. The duration of treatment is at least 10 days, and treatment must be continued even after the symptoms disappear. Additionally, rinses and inhalations are prescribed, the effect of which is aimed at suppressing the inflammatory process and pain, as well as eliminating plaque from the tonsils. To carry them out, special solutions or herbal decoctions are used, which are not difficult to prepare at home.
Throughout the treatment, the patient must remain in bed and minimize contact with people, so as not to further injure the inflamed tonsils.
It is also important to monitor your diet - fried, spicy and salty foods are prohibited. Food should be soft or ground to make swallowing easier. As for the temperature of food and drinks, it should be moderate, approximately 50°C.
The healing process is negatively affected by tobacco smoke, so smokers will have to abstain from this addiction, or better yet, get rid of it altogether. When smoking, the mucous membrane is irritated, and toxins settle on its surface, which interferes with normal tissue restoration. A similar situation arises when drinking alcoholic beverages - they put additional stress on the inflamed tonsils, which often leads to aggravation of the disease.
The procedure for washing the tonsils: when is it effective and how to do it correctly
The tonsils are mainly affected during the development of purulent tonsillitis. These pathologies are provoked by bacterial pathogens, which are activated when the human immune system weakens. The main method of treating such conditions is treatment with antibiotics with additional rinsing of the tonsils, which will reduce the required course of drugs, and therefore partially neutralize their side effects on the body. Most often, the procedure is performed for chronic forms of tonsillitis. The tonsils are designed in such a way that they have many depressions, lacunae, where the remains of dead epithelium and leukocytes collect and foci of suppuration are formed. Also, food debris lingers there, creating favorable conditions for the proliferation of pathogenic bacteria. Washing is carried out for cleansing. To do this yourself, you need to know how to rinse your tonsils.