What is periodontal tooth
The periodontium is a connective ligament that secures the tooth in the jaw bone. It is also common to call periodontium the tissue that fills the space between the alveolar process and the cementum of the tooth root.
Functions of periodontium
The main function of periodontal tissue is to anchor the tooth in the jaw bone. Physiological tooth mobility increases due to age-related and pathological changes. The width of the periodontium at the neck of the tooth should be 0.3–4.8 mm, at the apex – 0.25 mm, and in the middle of the root – 0.2 mm. Typically, the width of the periodontal space in incisors is greater than in chewing molars. With increased load on the tooth, the width of the periodontium increases, thereby causing slight loosening of the tooth roots.
Due to the fact that there are many nerve fibers in the periodontal fissure, when there is increased pressure on the tooth, a person feels an external influence. Thanks to this reflex, early physiological tooth mobility is almost impossible. Based on this, we can say that the fabric is also responsible for the shock-absorbing task.
Other functions of the periodontium include:
- plastic – participation in tooth growth;
- trophic – providing nutrition to the pulp;
- barrier – protecting the root from infection.
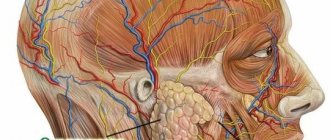
Anatomy
The histological structure of the periodontium includes the periosteum, alveolar tissue, periodontal ligament, gum and gingival sulcus.
- The periosteum is a dense tissue that is attached to the outer surface of the alveolar process.
- The alveolar process is a spongy bone penetrated by blood vessels and bone marrow.
- The periodontal ligament secures the teeth in the alveoli.
- The gums and gingival sulcus prevent pathogenic bacteria from penetrating into the periodontal gap.
A healthy periodontium is about 0.2 millimeters thick. It consists of elastic collagen fibers, between which are loose connective tissues.
The periodontium is literally permeated with blood vessels, which form the internal, middle and external plexuses and play the role of a kind of shock-absorbing pillow.
- The blood supply is successfully carried out by several longitudinal blood vessels.
- The lymphatic system is located along the small vessels.
- Innervation is carried out by two types of nerve endings - bushy and glomerular nerve endings of pulpal nerve fibers.
The structure of the periodontium
The structure of the periodontium includes collagen fibers, the beginning of which comes from the root cement, and the end from the alveolar process. Based on the location, the periodontium of a tooth can have a horizontal direction (at the apex of the interdental space) and an oblique course (at the apex of the tooth). Between the bundles of fibrous structures there are blood and lymphatic vessels. They deliver nutrients to the tooth tissue and gums.
Periodontal histology
The cellular composition of the periodontium includes:
- fibroblasts;
- macrophages;
- plasma cells;
- osteoblasts;
- osteoclasts.
Tissue histology shows that most of the periodontium is occupied by fibroblasts. It is these cells that make up the fibers of the ligament. During inflammatory processes, they participate in the regeneration of fibrous structures. In addition, histological examination of the tissue may reveal Malasse cells forming the epithelial lining of the cyst.
Periodontal fibers
The tissue fibers are composed of type 1 collagen protein. Collagen produced in fibroblasts is converted to tropocollagen. The resulting substance gives rise to fibrils, threads and bundles of periodontal tissue. Therefore, periodontal tissues have a fibrous structure. This structure gives the fibers flexible and elastic properties.
Anatomical and physiological features of periodontium
The anatomy of the periodontal ligament of the tooth indicates that the thickness of the tissue should not exceed 0.25 mm. However, this figure may change with increasing age and the presence of inflammatory and non-inflammatory gum diseases. Near the tooth germs, the thickness of the periodontium is much less - 0.1 - 0.15 mm, since the strength of the tissue is small compared to erupting teeth. Changes from the norm can be considered pathology.
The ligament itself consists of connective tissue and intercellular substance. It is in this substance that fibrous and collagen fibers are located. There are few elastic fibers in the connective tissue layers of the periodontal ligament, which allows this part of the tissue to resemble tendons. Elastic fibers are found most in the front teeth, and less in molars and premolars.
Innervation
The periodontium of the tooth is innervated by the facial arteries and the trigeminal nerve. The branches of the dental artery supply blood to the apexes of the root, and nutrition of the remaining parts of the tissue is provided by the interalveolar and gingival vessels. At the base of the periosteum, nerves, blood and lymphatic vessels enter the plexus. Through it, reflex impulses and biologically active substances pass into the pulp space.
The innervation of the periodontium may be impaired due to trigeminal neuralgia and serious facial injuries. In this case, emergency dental care is required.
PERIODONTIUM
Periodontium
(Greek peri around, about + odus, odontos tooth; syn.:
periodontal ligament, pericement
) - a connective tissue ligament that holds the root of the tooth in the dental alveolus of the jaw.
The periodontium develops simultaneously with the root of the tooth shortly before its eruption, i.e. in the postembryonic period. The development of the periodontium occurs due to the mesenchymal cells of the outer layer of the dental sac surrounding the tooth germ (see Teeth). The formed periodontium consists of bundles of collagen fibers stretched between the cementum of the tooth root and the bone walls of the dental alveoli. Bundles of P.'s collagen fibers have different arrangements. At the edges of the dental alveoli they have a mainly horizontal direction. Some of these fibers are woven into the gum, while others go around the neck of the tooth and form the so-called. circular ligament. This group also includes interdental fibers, which pass over the top of the interalveolar septum and connect adjacent teeth. In the lateral sections of the periodontal fissure, bundles of collagen fibers have a mainly oblique direction, and in the area of the apex of the tooth root they are located radially. In the spaces between the bundles of collagen fibers there are layers of loose connective tissue with individual elastic fibers, in which vessels and nerves pass. Among the bundles of P.'s collagen fibers, the so-called. oxytalan fibers, which in chemical composition occupy an intermediate position between collagen and elastic fibers.
The cervical part of the periodontal fissure is an area of accumulation of cells (fibroblasts, plasma and mast cells, osteoblasts, osteoclasts). Throughout the rest of the periodontal fissure, cells are grouped closer to the bone of the dental alveolus and to the cementum of the root. There are also small islands of epithelial cells (the so-called islands of Malasse), which are believed to represent the remains of the epithelial dental organ formed during the development of the tooth, and can serve as a source of development of the epithelial lining of dental granulomas and perihilar cysts (cystogranulomas).
Histochemical examination of the periodontium reveals a large amount of acidic glycosaminoglycans and high activity of redox enzymes in cellular elements.
Periodontal blood vessels form a rather dense network. They anastomose with the vessels of the gums and bone marrow spaces. Larger vessels are located in the recesses of the wall of the dental alveoli. In P., vascular glomeruli, as well as arteriovenous anastomoses, are described.
The periodontium contains many free bush-like nerve endings, which, apparently, are mechanoreceptors and record the degree of tension in the bundles of collagen fibers during the act of chewing. With age, P.'s fibers undergo partial destruction, especially in the cervical part, and the number of young cellular elements decreases.
Periodontium has a high regenerative ability. This allows, in case of P. injuries or complete dislocation of the tooth and rupture of the P. fibers, to implant the tooth into the dental alveolus (see Replantation). Among the pathological processes of P. there are inflammatory ones, including with the formation of dental granulomas near the roots of the brush (see Periodontitis), as well as periodontal disease (see).
Bibliography:
Gavrilov E.I. Biology of periodontal and dental pulp, M., 1969; Gemonov V.V. and Kozlovitser T.V. Fibrous structures of the periodontium, Dentistry, v. 53, no. 2, p. 9, 1974; Gemonov V.V., Giller L.I. and Kozlovitser T.V. On the issue of oxytalan fibers of the periodontium, in the book: Changes in periodontal tissues before and after prosthetics, ed. Sh. V. Bokanova and A. I. Voloshina, p. 57, M., 1972; Falin L. I. Histology and embryology of the oral cavity and teeth, M., 1963; Schumacher G.-H. u. Schmidt H. Anatomie und Biochemie der Zahne, B., 1972; Structural and chemical organization of teeth, ed. by AEW Miles, y. 1, NY - L., 1967.
BB Gemonov.
Periodontal diseases
The main disease occurring in periodontal tissue is called periodontitis. The disease is inflammatory in nature and is divided into:
- acute periodontitis: serous, purulent;
- chronic periodontitis: granulating, granulomatous and fibrous;
- aggravated periodontitis in chronic form.
With all types of disease, a cyst forms in the periosteum. Despite the fact that granulating and granulomatous periodontitis are included in the same group, they have differences in the manifestation of the disease. In the first case, the resulting cyst has a polygonal shape, and in the second – round. The sizes of the tumors also differ from each other.
Purulent periodontitis
The causes of periodontitis are different:
- gum injury;
- allergic reaction to drugs used in dental treatment;
- errors in tooth preparation and filling;
- errors in dental prosthetics.
The main cause of periodontal inflammation is infection. Bacteria penetrate into periodontal tissue through caries and its complications, as well as through inflamed areas of the gums.
Periodontal infections
With untreated caries, pathogenic microflora enters the tooth pulp. If the infection affects the pulp space so severely that it can no longer serve as a barrier to pathogens entering, then the inflammatory process penetrates deep into the ligament in a very short time. For this reason, the apex becomes inflamed, the dental nerve dies and decomposes, and a cyst with purulent contents begins to form in the bone.
The causative agents of periodontitis can be: staphylococci, streptococci, lactobacilli, actinomycetes and pneumococci.
Periodontium (periodontal ligament)
Periodontium (periodontium),
or pericement, somewhat conventionally called the ligament that holds the root of the tooth in the bony alveolus. The periodontium consists of a large number of thick bundles of collagen fibers located in the slit-like periodontal space. The width of this space averages 0.2-0.3 mm, but can shrink (in the absence of functional load) or increase (with strong occlusal loads on the tooth).
In the spaces between the bundles of collagen fibers of dense connective tissue in the periodontium there are layers of loose connective tissue (Fig. 44). About 60% of the volume of periodontal space is occupied by bundles of collagen fibers and 40% by loose connective tissue.
In the loose connective tissue, along with blood and lymphatic vessels, nerve elements, epithelial remains, or islands of Malasse (fragmentum epitheliale), can be located.
Cellular composition of periodontium
includes fibroblasts (the most common cells), cementoblasts (localized at the border with cement), osteoblasts (found at the border with the alveolar bone), macrophages, mast cells, all types of leukocytes, osteoclasts.
The number of fibroblasts in the periodontium is unusually large, their relative volume reaches 50%. At the ultrastructural level, numerous organelles are revealed in the cytoplasm of fibroblasts, providing a high intensity of collagen synthesis. Some cells of the fibroblastic series are myofibroblasts. They have a well-defined contractile apparatus. Myofibroblasts play an important role in tooth eruption. Fibroclasts contain lysosomes.
The periodontium also contains poorly differentiated cells of mesenchymal origin. They are located near blood vessels and serve as a source of renewal of some periodontal cells.
Basic substance of periodontium,
in which glycosaminoglycans, glycoproteins and a large amount of water are detected, it is a viscous gel.
Collagen fibers
They have a slightly wavy stroke, so they can elongate somewhat when stretched. Periodontal fibers are woven into the cement at one end and into the alveolar process of the bone at the other. Their terminal sections in both tissues are called perforating (Sharpey's) fibers.
Rice. 44. Histological specimen. Periodontium: 1 - bundles of collagen fibers; 2 - loose connective tissue; 3 - periodontal vessels
There are no mature elastic fibers in the periodontium of the tooth, but oxytalan fibers (immature elastic fibers) are detected.
In the periodontal fissure, thick bundles of collagen fibers have different directions: horizontal (at the edges of the alveoli), oblique (in the lateral parts of the fissure), radial (in the area of the tooth root) and arbitrary (in the area of the root apex). Based on the location of the attachment sites and the direction of the collagen fiber bundles, the following groups are distinguished:
1) alveolar ridge fibers
- connect the cervical surface of the tooth with the crest of the alveolar bone;
2) horizontal fibers
- located deeper than the fibers of the alveolar ridge, at the entrance to the periodontal space;
pass horizontally (at right angles to the surface of the tooth root and alveolar bone), form a circular ligament together with transseptal fibers
connecting adjacent teeth;
3) oblique fibers
- numerically predominant group, occupy the middle 2/3 of the periodontal
spaces connecting the root with the alveolar bone;
4) apical fibers
- diverge perpendicularly from the apical part of the root to the bottom of the alveoli;
5) interroot fibers
— in multi-rooted teeth, the root in the bifurcation area is connected to the crest of the interradicular septum.
The arrangement of periodontal fibers ensures that the forces acting on the tooth are distributed in the form of traction on the alveolar bone. So, collagen fibers ensure the main function of the periodontium - holding the tooth in the alveolus and distributing the chewing load.
The high rate of collagen renewal (2 times higher than in the gums and 4 times higher than in the skin) and the continuous restructuring of the periodontium contribute to the adaptation of the supporting apparatus of the tooth to changing loads. This explains the possibility of moving a tooth during orthodontic treatment without disrupting its connection with surrounding tissues.
Collagen synthesis requires a number of amino acids and vitamin C
etc. Lack of vitamin
C
in food leads to periodontal destruction and loosening of teeth (scurvy). But most often, periodontal destruction is associated with a chronic inflammatory process - periodontitis. The consequence of periodontitis is a progressive inflammatory process that affects the entire supporting apparatus of the tooth - the periodontium. Inflammatory-dystrophic periodontal disease (periodontitis) results in loosening and loss of teeth. Unfortunately, periodontitis affects a large portion of the population. When the inflammatory process spreads from the pulp to the periodontal area around the apex of the tooth, various types of periapical granulomas arise.
The periodontium is characterized by an intense blood supply. The sources of blood supply to the periodontium are the superior and inferior alveolar arteries, as well as the dental artery. Most of the arterial blood enters here through arterioles penetrating from the alveolar process through bone openings (perforating, or Volkmann, canals). In this case, the periodontium provides nutrition to the cement, which is devoid of blood vessels.
Periodontal vessels are connected to pulpal vessels (through accessory root openings), which is important for understanding possible routes of infection.
The periodontium is innervated by both afferent and efferent nerve fibers, forming a nerve plexus in the periodontal space. Nerve endings are predominantly mechanoreceptors and pain receptors.
The presence of a large number of receptor nerve endings allows us to consider the periodontium as a reflexogenic zone.
Epithelial remains (islets of Malasse), formed in the periodontium during the formation of the tooth root, are small accumulations of small epithelial cells with large nuclei surrounded by a basement membrane. As these structures grow, they can be a source of development of cysts and malignant tumors. At the same time, it is believed that the epithelial cells of the islets of Malasse are capable of producing some biologically active substances.
ANATOMIC AND PHYSIOLOGICAL FEATURES OF PERIODONTAL
The periodontium is a complex anatomical formation of connective tissue origin, located between the compact plate of the dental cell and the cementum of the tooth root (Fig.). Throughout its entire length, the periodontium is in direct connection with the jaw bone, through the apical foramen - with the dental pulp, and at the edges of the cell - with the gum and periosteum of the jaw.
The periodontium is first detected at the follicular stage of tooth development with the beginning of root formation and simultaneously develops with its growth and the formation of the cortical plate of the alveoli. Periodontal formation ends approximately a year after the end of development of the apex of the tooth root. On average, the thickness of the periodontium is 0.20-0.25 mm, but this value can change with age, tooth development, its function and, finally, as a result of the pathological process. In a formed, but not yet erupted tooth, the thickness of the periodontium is 2 times less (0.05-0.1 mm) than in a normally functioning tooth. With the loss of the antagonist, the width of the periodontal fissure decreases to 0.10-0.15 mm. In adulthood, the periodontal fissure becomes wider due to thickening of the periodontium. According to E.M. Gofung, the width of the periodontal fissure on the lower jaw is slightly smaller (0.15-0.22 mm) than on the upper jaw (0.20-0.25 mm). The width of the periodontal gap in human teeth varies even in its individual sections. In the middle third of the root, the periodontal fissure is narrowed and funnel-shaped expanded at the apex of the interalveolar septum and in the apical third due to micromovements of the tooth in the socket. Changes in periodontal thickness can be observed in connection with the pathological process. With increased load on the tooth, thickening (hypertrophy) of the periodontium and changes in the bone structure of the socket occur, which can lead to expansion of the periodontal gap. With cement hypertrophy (hypercementosis), the contours and size of the periodontal gap may also change. The consequence of the inflammatory process may be resorption of not only the walls of the socket, but also the cement of the root. The periodontium is formed by connective tissue, in which intercellular substance is distinguished; it contains fibrous collagen fibers and layers of loose connective tissue, penetrated by blood and lymphatic vessels and nerves. In the root apex region there is less fibrous tissue, but more loose connective tissue. The periodontium contains a small amount of thin argyrophilic fibers. Collagen fibers are formed from polypeptide molecules, which is responsible for the cross-striations of collagen fibrils, detected under an electron microscope. Fibrous fibers are folded into thick bundles, reaching 5-10 microns in diameter. The fibrous bundles of the periodontium are woven into the cementum of the tooth root at one end and pass into its fibrous structures, and at the other end into the bone tissue of the alveoli, providing a close connection between the periodontium and the surrounding tissues. At the alveolar wall, the collagen bundles are coarser than at the root cementum, where they form a delicate network. Collagen fibers of different parts of the periodontium differ in their direction and thickness of the bundles they form. The most powerful group consists of the so-called transseptal fibers. These are bundles of fibers running horizontally and connecting adjacent teeth. The bundles of fibers that make up this group are thick and fit tightly to each other. There is almost no layer of loose connective tissue between them. Above the transseptal group are bundles of collagen fibers that make up the lamina propria of the gums. Some of these fibers, acquiring an oblique direction, enter the cement. Directly around the neck of the teeth, intersecting with the transseptal group, there runs a relatively small group of fibers with a circular arrangement, called the circular ligament. Fibers of this group can break up into separate bundles. Starting from the top of the alveolar ridge and further along the entire periodontium, there are bundles of fibers that have an oblique direction, i.e., running at an angle to the longitudinal axis of the tooth. The places where fibrous bundles enter the bone of the socket are located above the places where these bundles enter the root cement. The bundles of fibrous collagen fibers located in this way tightly fix the tooth in the dental cell, the tooth seems to hang in the alveolus (Fig. 8.2). The functional orientation of periodontal fibers, like the trabeculae of the cancellous jaw bone, begins before they are included in the function during tooth eruption. In the apical part of the root, as in the cervical region of the periodontium, a certain number of fibrous bundles run in the radial direction, which prevents and limits the lateral movements of the tooth (Fig. 8.3). The vertical arrangement of collagen fibers to the bottom of the alveoli in the apical part of the periodontium prevents the tooth from moving out of the socket. The bundles of fibers running from the cement to the alveolar bone are connected to each other by numerous lateral anastomoses. These anastomoses can be considered as a kind of additional distributors of chewing load throughout the periodontium. Taking into account the difference in the direction and organization of collagen fiber bundles, they should be classified as follows: transseptal fibers; loose gum fibers (coming from the neck of the tooth and woven into the connective tissue of the gums); circular fibers (covering the neck of the tooth); alveolar ridge fibers (passing from the top of the alveolar ridges to the cement of the neck (tooth); oblique fibers; a group of apical fibers. Although the above groups of fibers can be traced in the periodontium of all teeth, nevertheless, the periodontium of functionally different teeth differs in structure. So, for teeth of the frontal group (incisors, canines) it is characteristic that the bundles of fibers that make up the periodontal tissue are relatively thin. This especially applies to the circular group covering the area of the tooth neck. The group of oblique fibers is divided into separate fragments by triangular spaces filled with loose connective tissue. Angle of inclination of these fibers is approximately 40-45° in the vestibular part of the periodontal fissure and 35° in the oral part. It should be noted that the angle of inclination of the fibers also varies in different parts of the periodontal fissure. In the periodontal area immediately following the neck of the tooth, the angle of inclination of the fibers fluctuates (25-35°).Below this level, the inclination of the fibers increases to 45-50°. And finally, in the periapical region, some of the fiber bundles, as noted above, take on an almost vertical direction. It should be noted that the group of underlying fibers in the anterior teeth is relatively small. Here one can observe a rather dense plexus of argyrophilic fibers. In the periodontium of small molars (group of premolars), bundles of collagen fibers thicken. This applies to both the circular and transseptal groups. The fibers going to the bucco-lingual direction are more clearly expressed here. The angle of inclination of the fibers of the oblique group was 20-25° in the cervical region, then increasing to 50-60°. In the group of fibers underlying the root apex, a cross-shaped weave is clearly visible. The periodontium of large molars (molars) is characterized by the presence of powerful transseptal and circular fibers, as well as thick bundles in the apical region of the periodontium, which seem to create a litter for the root apex. Also noteworthy are the well-developed bundles of fibers running in the horizontal direction and connecting the crest of the alveolar process with the cementum of the tooth root. The angle of inclination of the obliquely located fibers also increases more gradually from 20° in the cervical region to 40° in the middle sections of the root length. Particular attention should be paid to the fibers in the bifurcation area of multi-rooted teeth. The upper part of these fibers, connecting the crest of the alveolar septum with the cementum of the roots in the bifurcation region, resembles the alveolar ridge fibers in location. In addition, above the apex of the alveolar septum there are fibers running in a horizontal direction and seemingly connecting the roots of the teeth. These fibers form particularly complex weaves in teeth that have three roots. Below these fibers follow oblique fibers, basically repeating the direction of the fibers of the opposite sections of the periodontal fissure. The periodontium of teeth contains elastic fibers, but they are few. These are mainly thin fibers located between the bundles of collagen fibers of the periodontal ligament. It should be noted that these elastic elements are more often found in the periodontium of incisors and canines among the fibers of the cervical group. One of the features of periodontium is the presence of a significant amount of oxytalan fibers, so named for their resistance to acids. They are a permanent component of periodontal connective tissue. Their distribution is also uneven; they are more often found in the fibers of the cervical group and in the periapical region. Periodontal oxytalan fibers are a type of elastic fiber. The content of oxytal fibers and their thickness increase in the periodontium of teeth experiencing increased functional load. Oxytalan fibrils form a dense network that is woven between collagen fibers. Oxytalan fibers, connecting with periodontal blood vessels, form oxytalan-vascular structures. It has been established that, along with the plastic function, the oxytalan system is part of the periodontal receptor mechanism, which controls vascular tone. In the periodontium of teeth, especially multi-rooted ones, there are argyrophilic fibers, which morphologically are very similar to the argyrophilic fibers of reticular tissue. These fibers are most often detected in periodontal areas communicating with the medullary spaces of the jaw. Between the connective fibers in the periodontium there are cellular elements - fibroblasts with an oval nucleus and light cytoplasm, in loose connective tissue - mast cells and histiocytes (wandering cells) with a more brightly colored small nucleus and granular cytoplasm. Near the vessels and capillaries of the periodontium, perivascular adventitial histiocytes and mast cells are found. Mast cells have both a round and elongated shape. It has been established that the granularity of mast cells includes heparin and histamine, which are involved in the regulation of the permeability of the main substance of periodontal connective tissue. Plasma cells are mainly localized in the cervical region. They have a round shape with a sharply basophilic cytoplasm, a round nucleus and a characteristic arrangement of chromatin clumps. In the areas of the periodontium adjacent to the root cement, there are cementocytes - cells that have a plastic function in the construction of secondary (cellular) cement, and in the areas adjacent to the alveolus, there are osteoblasts - builders of the alveolar bone tissue. However, the set of cellular elements in different areas of the periodontium is different. A larger number of young, poorly differentiated cells are characteristic of the periapical and cervical zones of the periodontium, and in multi-rooted teeth, such an area is also the periodontium in the area of root bifurcation. In the middle sections of the periodontal fissure, more mature forms of fibroblasts predominate. It is characteristic that the number of plasma cells and mast cells is subject to the same fluctuations. In addition to these cells of connective tissue origin, epithelial formations are located closer to the cement - the so-called epithelial remains (relictum epitheliale). It is widely believed that these epithelial formations are the remnants of tooth-forming epithelium, which remains in the periodontium of the teeth throughout life. Domestic authors have proven the heterogeneity of the origin of these epithelial elements: in the periapical part of the tooth root they are remnants (islands, nests) of the perihilar epithelial sheath, and in the area of the tooth neck - remnants of the dental plate. The places of greatest localization of epithelial cells are the cervical and periapical parts of the periodontium. Here the largest complexes of these cells are revealed. The shapes and sizes of accumulations of epithelial cells are different. In some cases they look like a small group of cells, in others they look like short strands. It is very characteristic that the content of these epithelial remains is subject to pronounced age-related fluctuations. The largest amount of epithelial remains is found in the periodontium of people aged 10-20 years. A significant number of these cells are contained in the periodontium of people aged 21–30 years. At the same time, in the periodontium of people over 50 years of age, their number noticeably decreases. At the same time, the morphological structure of the residues themselves changes. In young people, larger epithelial complexes with fairly clear nuclear structures are observed, while in older people, these cells have a narrow rim of cytoplasm and a pyknotic dark-colored nucleus. The content of epithelial nests is reduced in the periodontium of teeth bearing a functionally increased load. Many authors argue that the epithelium of these nests, under certain conditions, can lead to the appearance of both benign (cystogranulomas, cysts) and malignant (cancerous) neoplasms.