Knowledge about microbes seems necessary to us only at school age, in biology lessons. However, for preschool children this information is no less important . Children often neglect brushing their teeth and washing their hands, but these hygiene rules are extremely important for health. Before telling anything to children, let's remember what germs are.
What are they, bacteria and microbes?
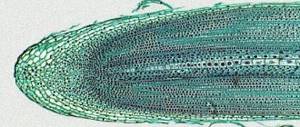
These are small creatures: it is impossible to see them with the naked eye. Examine surrounding objects for the presence of microbes on them under a microscope. Microbes live everywhere. They move with the help of flagella or tails, and in the water they bounce like balls. Animals and people are also carriers of germs: on their hands, unwashed vegetables and fruits, and wool.
Microbes feed on everything that is around. If you see mold on a piece of bread, it means that microbes have settled on it. Microorganisms can be breeding grounds for disease: these are viruses. To recover and get rid of multiplied microbes, a person is forced to take medications. To fight germs, it is imperative to practice good hygiene.
However, keep in mind: a dry and boring story about bacteria is unlikely to impress a child. He will listen to everything, but, most likely, he will continue to neglect his health. Poems, videos, photographs, pictures will help children present information about microbes in a bright and interesting way.
Benefits of dental treatment under a microscope
Dental treatment using a microscope has the following advantages:
- The ability to see details hidden to the naked eye;
- Quick and accurate detection of enamel fractures and cracks, the first signs of caries;
- Minimizing damage to healthy tissue when preparing carious cavities;
- Enlarging the local area of the surgical field allows one to observe not only the oral cavity, but also to examine an individual tooth in detail;
- Improved lighting. Light is locally directed to the location of magnification. The backlight can be halogen, LED or xenon. Each type has its own advantages when performing different tasks;
- Better visibility of root canals during endodontic treatment, reducing the likelihood of perforation and facilitating unfilling and removal of broken instruments;
- Detailed visualization of anatomical structures during implant treatment;
- Monitoring and assessment of the condition of soft tissues;
- Detection of areas of loose filling during diagnostics and restorations;
- The ability to photograph and videotape the treatment without interrupting it. These materials are provided to the patient for his better understanding of the problem with which he consulted the doctor and the results of treatment;
- Detailed recording of diagnostic results and treatment process;
- Photo and video materials obtained during treatment can be used not only to achieve understanding between the doctor and the patient, but also for consultations with colleagues, presentations at scientific conferences, teaching students, and participation in research.
Aids for studying the topic
To ensure that children are impressed by your story, show them pictures, photographs or a video film. These materials are prepared under a microscope. Scientists use a microscope to study the activity of microbes.
Cards: what should a child know about germs?
Pictures and photos show microbes magnified millions of times by a microscope. Poems about hygiene rules can accompany your story. You can download pictures, photos and poems for children on our website.
What can you see in a photo of bacteria?
If you take a quick look at the main search results for photos of bacteria, you will see a lot of interesting things. Among them, you can choose those that are frequent “visitors” of our hands.
You can pick up photographs taken with electron microscopes, in which bacteria look like multi-colored plush toys and cause sincere affection.
Such photos give an idea of the general structure of a certain type of bacterium, the location of flagella, the shape of the bacterial cell, and even the possible configurations of bacterial colonies. In addition, these photos are a very convincing demonstration of the relationship between the sizes of objects of the material world familiar to humans and living organisms - representatives of the microworld. The hairs on your hands look like giant pillars under an electron microscope, and the tiny balls and sticks sown between these pillars are those famous formidable bacteria.
Although some bacteria are the owners of some color (for example, photosynthetic bacteria always have a certain multi-colored pigment: either green, or red, or yellow, or several different ones at once), but these colors are not as saturated as electronic photographs sometimes show. Most often, bacteria in photographs taken with an electron microscope are specially colored by researchers. There are certain methods for staining bacteria, including the common Gram stain method.
In addition to coloring the bacteria themselves, photos are often also subject to artistic processing, as a result of which it is difficult to conduct any research on their basis, but you can get a lot of positive impressions by admiring the skill and ingenuity of nature.
Video
An interesting cartoon or video film, which contains a photo under a microscope, will quickly and clearly show the baby the danger of microbes. Here are some of the good and useful cartoons that you can watch on our website.
Lessons from Aunt Owl
This cartoon is a wonderful fairy tale about microbes and their effect on the human body. The information is presented in an accessible manner, without unnecessary terminology, and is aimed specifically at children of preschool or primary school age. The cartoon is accompanied by simple and at the same time understandable poems, and the main character - Aunt Owl's assistant - examines harmful bacteria under a microscope, where the microbes appear as if they were alive. You can watch the cartoon here:
Why brush your teeth?
This video film explains in detail why you wash your hands and brush your teeth, how a person feels taste, how the digestion process occurs, etc. Boring scientific information is presented in the form of characters who represent microbes, impulses entering the human brain and responsible for taste, etc. Thanks to such a non-standard presentation of the material, the child will be able to literally visually imagine not only what microbes are (this topic is secondary in the cartoon), but also generally understand how the human body works. You can watch the cartoon here:
Mitya and the microbus
The next cartoon called “Mitya and the Microbe” is more suitable for preschoolers. This video film tells about the boy Mitya, who, like all children, neglected hygiene methods. The cartoon has an interesting plot about beneficial bacteria and microbes fighting among themselves. Microorganisms are presented in the form of small people, which seem to be observed under a microscope. It's a puppet cartoon, but that doesn't make it any less interesting to watch. The characters in it sing funny songs, simple and instructive. You can watch or download the video film here:
Arkady Parovozov
This is a video film made on the basis of computer graphics. It is a story about a girl Masha who ate an unwashed tomato with germs. As a result, she developed a fever and a stomach ache. But a certain Arkady Parovozov, a kind of Superman, comes to the rescue, drives away the germs and returns Masha to good health. This is not to say that the cartoon is drawn perfectly. The figures are rather schematic, and all attention is directed to the poems about microbes, which the author of the video reads off-screen. You can watch the cartoon here:
Tooth enamel. Its microscopic and ultramicroscopic structure, physicochemical properties.
Formed by: enamel prisms, interprismatic substances, covered with cuticle. The thickest layer of enamel is in the area of the tubercles. Towards the cervical region, the thickness of the enamel gradually decreases. 96% of the enamel consists of inorganic compounds (hydroxyapatite, fluorapatite, carbonate apatite), 4% is an organic base and water. Organic substances are represented by proteins (53%), lipids (42%), and traces of carbohydrates were also detected. The cells that form enamel are enameloblasts; they arise as a result of the transformation of pre-enameloblasts, which differentiate from the cells of the inner enamel epithelium. Enamel is formed by enamel prisms and interprismatic substance. The main structural and functional units of enamel are enamel prisms. They pass through the thickness of the enamel radially, mainly perpendicular to the enamel-dentin border, curved in the shape of the letter S. Enamel prisms are arranged in bunches, 10-20 prisms each. In the neck area, the prisms are positioned horizontally. The cross-sectional shape of the prisms is oval, polygonal, more often arched (in the form of a keyhole). Enamel prisms consist of densely packed and ordered hydroxyapatite crystals. On the surface of the enamel there is a cuticle with a thickness of 0.6-1.5 microns, it represents a structureless organic shell, which is subsequently preserved only on the lateral surfaces of the tooth crown. The enamel cuticle consists of an internal glycoprotein layer (primary cuticle, Nasmyth's membrane) - the last secretory the product of ameloblasts, and the inner layer formed from the reduced epithelium of the enamel organ - the secondary cuticle; on most of the tooth the cuticle is erased; Pellicle - an organic film of precipitates of organic substances of saliva; forms within a few hours after brushing your teeth; dental plaque - is formed as a result of the colonization of the pellicle by microorganisms within 1 – 2 days; tartar - mineralized dental plaque; forms within about a week and a half.
48.Dentin, its microscopic and ultramicroscopic characteristics.
Dentin is the calcified tissue of the tooth, forming its main mass and definition. Its shape. Considered as specialized bone tissue. In the crown area it is covered with enamel, in the root - with cement. Primary dentin. It is formed during the period of tooth formation and eruption, making up the main part of this tissue. It is deposited by odontoblasts at an average speed of 4-8 µm/day, periods of their activity alternate with periods of rest. This periodicity is reflected by the presence of growth lines in dentin. Types of growth lines: Owen's contour lines - directed perpendicular to the dentinal tubules. Ebner's growth lines are located with a periodicity of 20 microns. Between the Ebner lines, with a periodicity of 4 microns, there are lines corresponding to the daily rhythm of dentin deposition. Ebner lines correspond to a 5-day cycle. Secondary dentin (physiological). It is formed after tooth eruption and is a continuation of primary dentin. The rate of deposition of secondary dentin is less than that of primary dentin. As a result of its deposition, the contours of the tooth chamber are smoothed. Tertiary dentin (replacement). It is formed in response to irritating factors only by those odontoblasts that respond to irritation.
49.Cement, its location and histophysiology. Cement is referred to as the supporting apparatus of the tooth. Included in the periodontium.
Cementum is one of the mineralized tissues of the tooth. The main function is participation in the formation of the supporting apparatus of the tooth. The thickness is minimal in the area of the tooth neck and maximum in the root area.
There are acellular and cellular cementum.
Acellular (primary) does not contain cells and consists of calcified intercellular substance, which includes collagen fibers and ground substance. Cementoblasts, which synthesize the components of the intercellular substance during the formation of this type of cement, move outward, towards the periodontium, where the vessels are located. Primary cementum is slowly deposited as teeth erupt and covers the 2/3 of the root surface closest to the neck.
Cellular cement (secondary) is formed after tooth eruption in the apical third of the root and in the area of bifurcation of the roots of multi-rooted teeth. Cellular cement is located on top of acellular cement or is directly adjacent to dentin. In secondary cementum, cementocytes are immured in calcified intercellular substance.
The cells have a flattened shape and lie in cavities (lacunae). The structure of cementocytes is similar to osteocytes of bone tissue. But, unlike bone, cement does not contain blood vessels, and its nutrition is diffuse from the periodontal vessels.
№50
According to the morphological structure, the pulp is represented by loose connective tissue, which contains many cells, intercellular substance, blood vessels and nerve fibers. Its peculiarity is that, along with cellular elements, it contains a large amount of gelatinous ground substance. The fibers are represented by collagen and reticular (argyrophilic), elastic fibers were not detected in the pulp. The main cellular elements of the pulp are odontoblasts, fibroblasts, poorly differentiated cells (stellate, pericytes), sedentary macrophagocytes and others. These cells are distributed unevenly in the pulp, forming a certain pattern. Conventionally, this allows us to distinguish three layers in it: the odontoblast layer, or peripheral, subodontoblastic, or cambial, central. Each of them performs a specific physiological function or exhibits one or another reaction during the development of various processes. 1 - primary dentin; 2 - secondary dentin; 3 - predentin; 4 - layer of odontoblasts; 5 - subodontoblastic layer; 6 - central layer. In the peripheral layer of the pulp, which is directly adjacent to the dentin, odontoblasts are located in several rows. These are highly specialized pear-shaped cells with dark, basophilic cytoplasm. The cell body is rich in cellular organelles: a well-developed intracellular mesh apparatus, a lamellar complex - the Golgi apparatus, numerous mitochondria, the nucleus contains a lot of chromatin and several nucleoli. Towards the apex of the tooth root, the size of cells and the number of rows of odontoblasts in the peripheral layer of the pulp decrease. The subodontoblastic layer consists of small, poorly differentiated stellate cells, from the body of which numerous processes extend, which are closely intertwined. The cells are located directly under the odontoblasts, connect with their elongated body and processes to the odontoblasts and enter the spaces between them. The cells of this layer have the ability, if necessary, to transform into odontoblasts. The central layer of the pulp contains cells such as fibroblasts, which are spindle-shaped. For pulp cells of the fibroblast type, a characteristic functional feature is their differentiation into specific pulp cells, preodontoblasts and odontoblasts. In addition to fibroblasts, this layer contains a large number of sedentary macrophagocytes (histiocytes). The presence of these reticuloendothelial cells in the pulp provides its protective role. Both the subodontoblastic and central layers of the pulp contain a large number of adventitial cells
№52
The cuticle covers the surface of the enamel of teeth after their eruption in the form of a thin shell consisting of two layers and designated as primary and secondary cuticle. Primary cuticle
- an internal thin (about 0.5-1.5 μm) homogeneous layer of glycoproteins, which is the last secretory product of enameloblasts.
The secondary cuticle
is formed by the outer (about 10 µm) layer of the reduced epithelium of the enamel organ. After teething, the cuticle is erased and can partially remain on the proximal surfaces.
Unlike the cuticle, tooth pellicle and dental plaque can form on the surface of the enamel throughout life. Pellicle is an acquired thin organic film that is formed from salivary glycoproteins on the surface of the tooth. The thickness of the pellicle is 1-4 microns. It is a structureless formation that does not contain bacteria and is tightly fixed to the surface of the tooth. The formation of acquired pellicle is influenced by the pH of saliva. The pellicle is formed within 20-30 minutes and its formation begins with the adsorption of specific salivary proteins on enamel hydroxyapatites. Ionic bonds and hydrophobic interactions are formed between the enamel surface and the deposited proteins. Tartar Calcium phosphate crystals are deposited within dental plaque and bind closely to the enamel surface.
The process of deposition of inorganic substances in dental plaque takes about 12 days and after mineralization, the stone is no longer so easily removed by mechanical action or flow of saliva. Bacteria continue to accumulate on the surface of the resulting tartar, promoting its growth. Depending on the location on the surface of the tooth, supra- and subgingival tartar are distinguished. The composition of supra- and subgingival dental calculus is similar, but they differ in the sources of phosphorus-calcium compounds. They enter supragingival tartar from saliva, and subgingival tartar from gingival fluid. Inorganic substances in tartar are associated with proteins, the amount of which is 0.1-2.5% and depends on the type of tartar. The largest amount of protein (2.5%) is present in light supragingival calculus. In dark supragingival calculus, the protein content is reduced to 0.5%, and in subgingival calculus it is only 0.1-0.3%. In addition to proteins, various amino acids are found in tartar. Residues of alanine, leucine, glycine, glutamic and aspartic acids, as well as proline, lysine, serine and threonine are detected in the greatest quantities. Glutamate and aspartate are able to bind Ca2+ ions, and serine, threonine and lysine residues - PO43-, which is very important for the initiation of plaque mineralization and further formation of tartar. No. 51
The periodontium is a complex of tissues that surround the tooth and ensure its fixation in the jaw bones. This complex includes the gum, periodontal ligament connecting the tooth root to the bone socket, bone tissue of the alveolar processes and cementum of the tooth root. Gums . The mucous membrane is represented by two layers: flat stratified highly keratinized epithelium and the lamina propria. There are no glands, lymph nodes and submucosal layer. The mucous membrane fuses with the periosteum of the jaw bone. In the area of the horny ridges of the upper jaw, the stratum corneum of the epithelium reaches its greatest development in ruminants. The main plate is rich in elastic fibers and blood vessels. The main structures of the tooth are: dentin, enamel, cement, pulp. The tooth cavity and the root canal are filled with pulp in the form of fine fibrous connective tissue. Its surface layer contains several rows of cells of mesenchymal origin. They are called odontoblasts and have a pear-shaped shape, basophilic fine-grained cytoplasm, and a basally located nucleus. A long process extends from the outer surface of the odontoblast. It penetrates into the dentin located outside the pulp and lies there in the dentinal tubule (Fig. 253). Odontoblasts are similar in structure and significance to osteoblasts of bone tissue. Thin collagen fibers pass between the odontoblasts, which become the collagen fibers of dentin. Deeper than the layer of differentiated odontoblasts lies a layer of poorly differentiated cells, from which odontoblasts develop. The next layer of pulp consists of loose connective tissue rich in blood vessels and nerve fibers. Dentin makes up the main part of the crown of the neck and root of the tooth. This is a type of bone tissue characterized by significant hardness. As the root of a developing tooth forms and cement is deposited on its surface, the periodontal ligament develops from the surrounding mesenchyme. It consists of wide bundles of collagen fibers, which are located in the form of a suspensory ligament between the cement covering the root of the tooth and the bone wall of its alveoli. The fibers at both ends are immersed in dense fabric. This indicates that the bone matrix of the alveoli, on the one hand, and the cementum matrix, on the other, are deposited around the previously existing collagen fibers. Nevertheless, the rate of collagen renewal in the periodontal ligament is exceptionally high, therefore, during life, significant restructuring of the ligament occurs, at least those parts of it that are not enclosed in dense tissue. Collagen fibers in the bundle run slightly wavy. due to this arrangement, the displacement of the tooth in the bone alveolus is very slight. The periodontal ligament contains a large number of nerve endings that are sensitive to pressure; thus, for example, foreign solids are easily detected in soft foods. The alveolar process is the part of the lower or upper jaw that extends from their bodies and surrounds the roots of the erupted teeth. There is no sharp boundary between the body of the jaw and its alveolar process. It develops along with jaw growth and teething, and after tooth loss it almost completely resolves. The alveolar process is formed by two walls - the outer (buccal or labial) and the inner (lingual). On the outside, the walls are formed by the so-called cortical plates, which are built from compact bone substance. Between the cortical plates of the alveolar process is the labial bone, formed by a system of intertwining bone beams. The spaces between the trabeculae of cancellous bone are filled with bone marrow. The cortical plate provides strength and protection to the underlying bone and serves as an attachment site for skeletal muscles. The cortical plate is denser in the lower jaw than in the upper jaw and has fewer openings for the passage of neurovascular bundles. At the edge of the alveolar process, the cortical plate passes into the wall of the dental alveolus (ethmoid bone), which is a relatively thin perforated plate adjacent to the root of the tooth. Through its numerous openings, blood vessels and nerves penetrate into the periodontium. The space between the two walls of the alveolar process is divided transversely by bony septa, resulting in the formation of a number of individual pits, or alveoli, in which the roots of the teeth are placed.
№53
The glands of the oral cavity include large salivary glands (submandibular, sublingual) and small glands of the hard and soft palate, as well as glands of the tongue. Based on the nature of the secretion that the glands secrete into the oral cavity, mucous, protein and mixed glands are distinguished. Mucous and mixed glands are present in the cheeks and lips. In the area of the hard and soft palate and uvula, mucous glands are secreted. The glands of the tongue are mixed, protein and mucous.
The parotid salivary gland (glandule parotis) is a paired organ located in the parotid-masticatory region of the head. This is a complex branched alveolar gland with a protein type of secretion. The mass of each gland is 20-30 g, the shape is polygonal, the dimensions are 5x4x3 cm. The connective tissue capsule forms an ingrowth into the organ, which divides the parenchyma of the gland into lobules. The terminal secretory sections are protein, in structure they resemble similar structural components of the submandibular salivary gland; in the center of the acinus there are secretory cells - serocytes; myoepithelial cells are located on the periphery; Externally, the acini is surrounded by a basement membrane. The system of excretory ducts of the parotid salivary gland includes insertion, divided, interlobular and common excretory ducts. The named structures do not differ significantly from similar formations of the submandibular gland. The common excretory duct of the parotid salivary gland passes through the buccal muscle and flows into the vestibule of the oral cavity on the inner surface of the cheek at the level of the upper molar.
№54
The glands of the oral cavity include large salivary glands (submandibular, sublingual) and small glands of the hard and soft palate, as well as glands of the tongue. Based on the nature of the secretion that the glands secrete into the oral cavity, mucous, protein and mixed glands are distinguished. Mucous and mixed glands are present in the cheeks and lips. In the area of the hard and soft palate and uvula, mucous glands are secreted. The glands of the tongue are mixed, protein and mucous.
The submandibular salivary glands (glandula submandibulars) are a paired organ located on the inner surface of the lower jaw. The mass of each gland is 10-15 g, the shape is oblate-ellipsoid, dimensions 4x2x1.5 cm. This is a complex alveolar-tubular branched gland with a protein-mucosal type of secretion. Connective tissue septa extend from the connective tissue capsule into the gland, dividing the parenchyma into lobules. The terminal secretory sections of the submandibular salivary gland are of two types - protein and mixed. Protein acini make up the vast majority of the parenchyma of the gland. Each protein acini is built with 10-15 serocytes; myoepithelial cells surrounded by a basement membrane are located on its periphery. Serocytes are conical cells with basophilic cytoplasm, a round nucleus, well-developed elements of the granular endoplasmic reticulum and the Golgi complex. Intercellular tubules are located between neighboring serocytes, which remove the products of the secretory activity of serocytes. Part of the secretion leaves the cells due to their apical surface. Myoepitheliocytes or basket-shaped cells have processes that cover the bases of serocytes. Contraction of the processes of myoepithelial cells promotes the removal of secretions from the terminal secretory sections into the system of excretory ducts.
№55
The glands of the oral cavity include large salivary glands (submandibular, sublingual) and small glands of the hard and soft palate, as well as glands of the tongue. Based on the nature of the secretion that the glands secrete into the oral cavity, mucous, protein and mixed glands are distinguished. Mucous and mixed glands are present in the cheeks and lips. In the area of the hard and soft palate and uvula, mucous glands are secreted. The glands of the tongue are mixed, protein and mucous.
The sublingual salivary gland (glandula sublingualis) is a paired organ of a flattened-elliptical shape, located under the mucous membrane of the lingual area, above the diaphragm of the mouth. The mass of each gland is about 5 g, dimensions - 2x1x0.7 cm. In structure, it is a complex branched alveolar-tubular gland with a mucous-protein type of secretion. Unlike the submandibular and parotid glands, the connective tissue capsule around the sublingual gland is poorly defined. The parenchyma of the gland is divided into segments by connective tissue septa. The terminal secretory sections of the sublingual salivary gland are formed mainly by mucocytes. A small part of the acini also contains Gianuzzi's protein crescents, the cells of which synthesize lysozyme, an enzyme that can dissolve the membrane of some types of bacteria. The base of the acini of the sublingual salivary gland is covered by processes of myoepithelial cells. The inserted and divided straits in the sublingual salivary gland are less developed compared to the parotid and submandibular glands. The excretory ducts of the sublingual salivary glands (straits of Rivinus) flow into the oral cavity at the ducts of the submandibular gland along the sublingual fold. When comparing the parotid, submandibular and sublingual salivary glands, one should pay attention to the uniformity of the structure of the acini of the parotid salivary gland (the presence in its composition of only proteinaceous final secretory sections), the presence of two types of acini (proteinaceous and mixed, with a predominance of proteinaceous) in the submandibular gland and two types of acini (mucous and mixed, with a predominance of mucous) in the sublingual salivary gland.
№56
The following layers of the esophageal wall are distinguished: adventitia, muscular layer, submucosal layer and mucous membrane. The most massive layer is the muscular layer (tunica muscularis), which consists of an outer layer of longitudinal fibers and an inner circular one. The layers are separated by a thin connective tissue layer. The intermuscular autonomic nerve plexus is also located here. Part of the muscle fibers of the esophagus that pass to the mediastinal pleura is called the pleuroesophageal muscle (m. pleurooesophageus). The muscles of the upper third of the P. are striated, and the lower third are smooth. The middle third of the P. contains mixed muscles. The movement of food masses through the esophagus occurs due to active peristaltic contractions of muscle fibers. The mucous membrane of the esophagus (tunica mucosa) is covered with multilayered squamous epithelium, extending from the pharynx. In adults, it consists of 20-25 cell layers 0.5-0.8 mm thick. The epithelium of the esophagus lies on thin fibrillar tissue, which is separated from the submucosal layer by a layer of muscle tissue (tunica muscularis mucosae). There are many mucous glands scattered throughout the mucous membrane. In the caudal part of P., in the mucous membrane itself, there are cardiac glands that produce pepsin. The submucosal layer (tela submucosa) consists of loose connective tissue penetrated by vessels and nerves. There are also many small glands and lymph nodes, especially in the ventral wall of the upper third of the P. The submucosal layer is the least extensible, which is important to consider when suturing the P. The outer connective tissue membrane (tunica adventitia) of the P. consists of intertwined bundles of collagen and elastic fibers and cellular elements. Penetrating between the muscle bundles, adventitia fibers penetrate other layers of the esophagus and form its frame. The most superficial layers of the adventitia, more loose, imperceptibly pass into the periadventitial tissue and connect with the fascial layers of the neck and posterior mediastinum. Fibrous fibers of the adventitia fix P. to the spine. Loose fiber separates P. and forms layers between the organs of the posterior mediastinum.
Germs in your mouth are normal
It is not surprising that from 200 to 500 species of a wide variety of microscopic creatures - fungi, bacteria, viruses, protozoa - are constantly “registered” in the mouth.
The oral cavity is an ideal place for them to live and reproduce - it is always warm, humid and there is something to eat.
Even with the most careful cleaning, some food remains in the fissures (natural crevices of the teeth), in the spaces between the gum and neck of the tooth, hollows, folds of the mucous membrane. That is why dentists advise, in addition to a toothbrush, to use dental floss and irrigators - devices that supply a stream of water under pressure and allow you to remove all foreign organic matter from your mouth as much as possible at home. But even a well-cleaned oral cavity contains billions of microorganisms, and this is normal.
Bacteria commonly found in root canals
The American Dental Association may state that bacteria found in root canal teeth are not capable of causing disease, but the bacteria in root canal teeth are not the same normal bacteria found in your mouth. Without oxygen and nutrients, harmless bacteria become highly toxic, capable of causing long-term infections, jaw loss and a variety of illnesses.
Hal Huggins, in his article on the dangers of root canals, shares the following information about the top 5 types of bacteria out of 53 commonly found in teeth with root canals.
- Capnocytophaga ochracea
: Found in brain abscesses associated with dental source infections. Causes diseases in the human central nervous system. Also associated with sepsis and meningitis. - Fusobacterium nucleatum
: Produces toxins that interfere with the division of fibroblast cells and disrupt tissue healing processes. Causes infections in the heart, joints, liver and spleen. - Gemella morbillorum
: Associated with acute infective endocarditis, septic arthritis, and meningitis. - Leptothrix buccalis
: Reduces the number of neutrophils (extremely important white blood cells), thus reducing the strength of the immune system. - Porphyromonas gingivalis
: Destroys red blood cells by making holes in them through porin proteins through which the cell contents flow out. Low red cell counts that do not recover after visits to the dentist are a common response to this exposure to this microorganism. Porphyromonas gingivalis also disrupts the integrity of the endothelial layer of blood vessels, leading to inflammation and bleeding in the inner lining of blood vessels.
According to Dr. Huggins, this is the main cause of atherogenesis leading to heart attacks. Porphyromonas gingivalis is capable of converting bacteria that are friendly to the body into pathogenic ones.
How does a pathogen destroy a tooth?
After eating carbohydrates, sugar breaks down in the mouth and fermentation processes begin. The pH value of the medium decreases from 6 to 4 pH, saliva becomes acidic within 5–15 minutes.
During the fermentation of various carbohydrates in dental plaque, lactic, propionic, butyric, pyruvic, formic and other complex acids are synthesized. Sucrose is actively fermented, while glucose and fructose ferment less intensively.
Acids dissolve tooth enamel and cement, resulting in their demineralization. Bacteria penetrate deeper and deeper and a carious cavity forms.
If the acidity of the environment remains high for several hours every day, the protective (buffering) qualities of saliva do not have time to recover. Tooth decay occurs quickly under these conditions.
Important! Sugar substitutes sorbitol, mannitol and xylitol are low cariogenic. Although they also penetrate into the plaque, the enzyme that converts them into fructose is weakly active
The upper part, protected by enamel, is destroyed in about 4 years. Dental cement is 2–2.5 times faster. In the case of cervical caries, the process will develop in 1.5–2 years.
The rate of development of pathology depends not only on external factors. Heredity and genetic characteristics of a person matter here.
Beneficial bacteria
The vast majority of them are creatures that live in symbiotic or mutualistic relationships with donor organisms (within which they live). Typically, such bacteria take on some of the functions that the host body is not capable of. An example is bacteria that live in the human digestive tract and process part of the food that the stomach itself is not able to cope with.
Some types of beneficial bacteria:
Escherichia coli (lat. Escherichia coli)
It is an integral part of the intestinal flora of humans and most animals. Its benefits are difficult to overestimate: it breaks down indigestible monosaccharides, promoting digestion; synthesizes vitamins K; prevents the development of pathogenic and pathogenic microorganisms in the intestines.
Macro photo: colony of Escherichia coli bacteria
Lactic acid bacteria (Lactococcus lactis, Lactobacillus acidophilus, etc.)
Representatives of this order are present in milk, dairy and fermented products, and at the same time are part of the intestinal and oral microflora. They are capable of fermenting carbohydrates and in particular lactose and producing lactic acid, which is the main source of carbohydrates for humans. By maintaining a constantly acidic environment, the growth of unfavorable bacteria is inhibited.
Bifidobacteria
Bifidobacteria have the most significant effect on infants and mammals, constituting up to 90% of their intestinal microflora. By producing lactic and acetic acids, they completely prevent the development of putrefactive and pathogenic microbes in the child’s body. In addition, bifidobacteria: promote the digestion of carbohydrates; provide protection of the intestinal barrier from the penetration of microbes and toxins into the internal environment of the body; synthesize various amino acids and proteins, vitamins K and B, useful acids; promote intestinal absorption of calcium, iron and vitamin D.
Causes of dental plaque formation
We mentioned earlier that the mechanism of plaque formation on teeth is supported by bacteria.
Let's see what are the reasons that predispose to the proliferation of bacteria in the oral cavity and, accordingly, lead to the formation and accumulation of dental plaque:
- Poor oral hygiene: the formation of an amorphous film on which bacteria adheres begins a few hours after brushing the teeth. For this reason, it is recommended to brush your teeth at least twice a day and especially after meals.
- Diet rich in sugars: Bacterial metabolism is based on the use of sugars. A diet rich in carbohydrates, simple sugars, alcoholic and carbonated drinks promotes the metabolism of bacteria, their accumulation and plaque formation.
- Not flossing: Not flossing enough is one of the causes of plaque buildup. A toothbrush is not able to reach all places, especially the interdental spaces where the largest number of bacteria accumulate.
- Avoiding mouth rinse: Mouth rinse should be used every time you wash your teeth to enhance the antibacterial effect obtained from the toothpaste and the mechanical action of the toothbrush.
- Dental Disclaimer: You should see your dentist at least once a year.
What are the possible consequences of dental plaque?
Preventing caries using bacteria
It turns out that bacteria can be not only enemies, but also allies in the fight against caries. Researchers in Japan came to this unexpected conclusion.
The microorganisms Streptococcus salivarius live on the surface of the tongue and oral mucosa. Their main mission is to prevent their “bad relatives” - Str. mutans.
Who knows, perhaps in the near future they will begin to add FruA protein to toothpastes for effective caries prevention.
Cariogenic bacteria are the main pests of our teeth. But they are far from the only ones. Be sure to familiarize yourself with other risk factors for tooth decay.
Bacteria of this disease
The cause of tooth decay is cariogenic bacteria. Some types of microflora have a destructive effect on the hard shells of teeth.
What microorganisms cause damage?
In the formation of pathology, the main role is played by bacteria and pathogens of the genus Streptococcus, species mutans, sanguis, sabrinus, viridans, salivarius, mitis and lactobacilli (Lactobacillus).
The bacteria Streptococcus mutans has the greatest destructive effect on teeth.
Dozens of species of other bacteria live in the mouth, the activity of which does not cause tooth decay. Some of them are enemies of streptococci, which cause caries, and destroy them.
The role of microbes in development or pathogenesis
Pathogenic microbes synthesize organic acids and other active compounds in the process of anaerobic glycolysis. These substances react with the enamel and cement of the tooth and destroy them. As a result, carious cavities are formed.
Under what conditions do bacteria develop in the oral cavity? There are several reasons for the active reproduction of cariogenic organisms on teeth:
- Imbalance of bacterial flora in the mouth.
- Diet with excess carbohydrates.
- Insufficient amount of saliva.
- Lack of fluoride in drinking water.
- Neglecting to brush your teeth, not using toothpicks and floss.
- Stress, decreased immunity.
How it happens
There are several key stages in its development:
Plaque forms. Staphylococci form deposits that firmly adhere to the surface of enamel and cement. The deposits consist of 10% bacteria, the remaining 90% are waste products of microflora. Most often, plaque appears in fissures - recesses in the upper part of the chewing teeth, in the lateral areas, and between them.
Photo 1. A thickened layer of plaque on the lower front teeth from the back.
- A plaque is formed from thickening plaque. Once it has reached the plaque stage, it cannot simply be brushed off. The acids underneath the plaque destroy (demineralize) the tooth tissue, and the dentist diagnoses tooth decay.
- Caries appears. Bacteria attack the hard shells of the tooth. They show brown and black pits, cracks, and grooves. The destruction process extends to dentin.
- The dentin becomes porous and fluid gets into it, which puts pressure on the tubules. The tooth aches when sweet, salty, cold or hot food enters the cavity. The carious cavity increases in size and reaches the root canal. The inflammatory process begins in the pulp. If the nerves are affected, severe toothache begins. And not only after eating, but also at rest.
If you endure the pain, the pulp dies, as do the nerve endings. The infection can spread to the periodontium, circulatory system and bone tissue.
Important! If a tooth is left untreated, caries will destroy it inside and out. Cysts and granulomas form around the destroyed root
How quickly can it form
In babies, it can appear less than a year after the eruption of a baby tooth. This happens if parents give their child sweets before bed and do not control the consumption of treats.
Photo 2. Cervical caries of baby front teeth in a child occurs due to poor nutrition.
If the baby often takes medications with sugar, for example, cough drops, expectorant and antipyretic syrups, children's vitamins, caries appears very quickly. The habit of treating yourself to sweets before bed is extremely harmful.