Causes of desquamative glossitis
The exact cause of desquamative glossitis is still unclear. It is assumed that the basis of the disease is a violation of the processes of keratinization and changes in the dystrophic nature of the filiform papillae with the subsequent formation of focal rejection of the mucous membrane.
Since glossitis is divided into primary and secondary, there are two groups of causes.
Among the factors that provoke the development of primary glossitis include:
- Mechanical trauma that constantly affects the mucous membrane. The surface of the tongue can be damaged by chipped or fractured teeth, insufficiently ground fillings, incorrectly installed crowns, as well as other dental structures and devices. This group also includes injuries due to teething.
- Thermal burns that occur after drinking hot drinks.
- Chemical burns associated with exposure to irritants.
Factors that provoke the development of secondary glossitis include various diseases. Among them are:
- Inflammatory pathologies affecting the gastrointestinal tract. These are mainly chronic gastritis, esophagitis, and also the duodenum.
- Pathologies of the liver and gall bladder.
- Systemic collagenoses.
- Autoimmune processes.
- Diseases of the hematopoietic system.
- Autonomic-endocrine disorders.
- Chronic dermatitis, as well as skin diseases resistant to therapy.
- Insufficient levels of B vitamins, microelements and macroelements in the body, for example, folic and pantothenic acids.
Less commonly, the disease can develop against the background of infectious diseases. These include:
- Scarlet fever.
- Mycoses.
- Viral lesions.
- Worm infestation.
Changes in appearance depending on the disease
One of the common types is “geographical tongue,” in which its upper surface resembles a map with the borders of countries and continents. This is the most common form of glossitis, which does not manifest itself in any way and does not require medical intervention unless complications arise (numbness, burning). This form occurs in waves, provoked by rough or spicy food, and hormonal cyclic changes. But the loss of the pattern of the papillae may indicate the presence of hypo- or hyperacid gastritis (that is, with increased or decreased acidity of gastric secretions) - such symptoms are typical for patients with gastroesophageal reflux, when hydrochloric acid and bile are thrown from the stomach into the oral cavity.
"geographical language"
The second most common type of glossitis is a folded tongue. This is an independent type of glossitis. In this case, the back of the tongue seems to be riddled with deep cracks and it feels like there are folds in it. This form of glossitis sometimes accompanies neurological diseases (for example, Melkerson-Rosenthal syndrome) and is present in people with acromegaly (hormone-active pituitary tumor).
"folded tongue"
Also characteristic are manifestations of various anemias, which are reflected in the appearance of the organ: iron deficiency anemia can manifest itself as a burning sensation on the tip of the tongue, the appearance of cracks on it and an erased pattern of taste buds. Pernicious anemia (B12 deficiency), in which the tongue has a “varnished” appearance with a smooth, swollen surface, sometimes quite painful, with burning symptoms, is the main cause of Gunther-Miller glossitis.
"lacquered tongue"
A large group of pathological conditions of this organ are ENT-associated symptoms associated with chronic tonsillitis - here the symptoms are non-specific, ranging from a dirty coating on the tongue to manifestations of diphtheria with white masses that are difficult to remove.
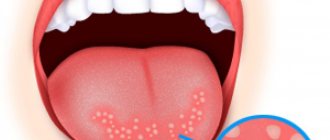
They also distinguish the formation of ulcers on the tongue - aphthous glossitis, which, as a rule, has a viral cause and goes away on its own. This is a recurrent disease, with more frequent episodes it is necessary to exclude pathology of the immune system.
When visiting a doctor, you will often notice pronounced teeth marks on the side of the tongue - a sign of long-term swelling. This occurs in patients with enterocolitis, kidney disease and cardiovascular diseases. The reason for this condition is water retention in the body.
teeth marks on the side of the tongue
In the presence of abundant white plaque, accompanied by pronounced redness of the oral mucosa, one should suspect a fungal infection, often of a candidal nature. In this case, HIV must be excluded. Also with HIV, “hairy leukoplakia” occurs, when the tongue appears to have white hairs on the side surface, similar to flames - this condition is specific to HIV.
"white hairy tongue"
It is worth noting the existence of a “black hairy tongue”, which is a symptom of gastrointestinal disorders, less commonly a fungus.
"black hairy tongue"
As you can see, our organ of taste reflects deep processes in the body, and it is difficult to single out one specialist responsible for its treatment. It is worth involving doctors of different spectrum in therapy, conducting studies based on data from smears and blood tests. But what general recommendations can we, as doctors, give to patients?
Classification of desquamative glossitis
In clinical practice, the disease occurs in three forms.
Table 1. Forms of desquamative glossitis.
| Form | Symptoms |
| Superficial | Spots and stripes form on the surface of the tongue, having a clear boundary, a shiny surface with a bright tint. They are surrounded by healthy mucous membrane along the periphery. Slight itching and burning may occur. |
| Hyperplastic | Hypertrophy of filiform papillae leads to the formation of compactions that have a whitish or yellow tint. The patient has a constant sensation of a foreign body in the oral cavity. |
| Lichenoid | The disease is characterized by an increase in fungiform papillae with constant migration of lesions. The most characteristic symptoms include a burning sensation. |
Burnt sugar for coughs - helps or not, reviews, how treatment is carried out
In addition, glossitis is divided into main types.
Causes of glossitis
Glossitis occurs under the influence of provoking factors. The most common of these is damage to the mucosa. Damage can occur due to the consumption of hard, spicy, hot foods. Often the tongue is injured by crowns, tooth fragments, braces or improperly made removable dentures. For infection to penetrate, a microscopic defect is sufficient, which does not cause discomfort and is visually invisible.
The source of infection in the oral cavity increases the likelihood of inflammation during injury. These include carious teeth, gum inflammation, stomatitis, and chronic tonsillitis. Failure to comply with hygiene rules, using someone else's utensils, toothbrushes, and dirty hands while eating increase the risk of infection entering the oral cavity. Children who can put dirty hands and foreign objects into their mouths are at particular risk.
Smoking and alcohol reduce local immunity and make the mucous membrane more vulnerable. In this group of patients, glossitis occurs more often than in other people.
Constant exposure to chemicals that destroy the mucous membrane eventually leads to chronic inflammation. Glossitis can even be caused by poor-quality toothpaste or mouthwash.
Dysbacteriosis, carriage of the herpes virus, reduced immunity are predisposing factors in the occurrence of glossitis.
Microbial
Dysbiotic inflammation of the tongue is most often provoked by exposure to opportunistic flora. As the pathological process progresses, pathogenic microorganisms join it, provoking the clinical picture of the disease.
Microbial glossitis develops against the background of infectious and inflammatory processes in the respiratory tract or digestive tract. Additional diagnostics reveal a decrease in blood flow in the vessels of the tongue, immunoglobulins responsible for local immunity, as well as a decrease in the keratinization index.
Candida
The secondary version of glossitis develops not only against the background of a violation of the microflora of the digestive tract, but also against chronic inflammation of the mouth, ears and nose. A decrease in local immunity provokes the addition of fungal flora, causing hypertrophic growth of the papillae.
The area of desquamation does not migrate, but the plaque becomes bright and white. Epithelial cells that are ready for lysis proliferate, and the resistance index decreases by more than 30%.
Diamond-shaped (median) glossitis
Most often, rhomboid glossitis is a congenital anomaly of the tongue as a result of disruption of fetal development processes. But it can also occur against the background of chronic diseases of the digestive system, especially with low acidity of gastric juice.
This form of glossitis is characterized by thickening of the epithelium and the appearance of a diamond-shaped lesion on the posterior third of the tongue in front of the circumvallate papillae along the midline of the tongue. The color of the affected area may be bluish-red. Rhomboid glossitis is a chronic disease and can torment a person for years with multiple relapses.
There are 3 forms of rhomboid glossitis:
- flat (smooth: the surface of the lesion is smooth, polished, there are no papillae of the tongue)
- warty (tubercular: the presence of lumpy dense outgrowths)
- papillomatous (hyperplastic: the presence of whitish-pink growths with a wide base and flattened apexes).
Treatment for rhomboid glossitis depends on its shape. For flat glossitis, treatment is usually not carried out. Warty and papillomatous glossitis are subject to surgical treatment. In this case, laser evaporation and tissue hair removal, as well as radiosurgery, are most often used.
Neurogenic
Glossitis of neurogenic origin, which has a secondary nature of development, most often occurs against the background of diseases affecting the nervous system. Among them are astheno-neurotic syndrome, phobias and fears, as well as neurasthenia of various origins. In severe cases, pathology is formed due to severe mental illness.
The disease is characterized by increased levels of norepinephrine, as well as impaired blood flow in the tongue due to narrowing of the capillaries. In addition to the excess number of sites ready for apoptosis, there is a decrease in saliva production. Due to mental disorders, cancer fear is formed.
Symptoms
In most cases, the disease develops acutely. The patient may not complain for a long time; they are only concerned about the change in the shape and appearance of the tongue. The first symptoms include the appearance of discomfort and burning in the mouth.
Less commonly, it is pain in the tongue and impaired sensitivity.
After a few days, a patch of various shapes forms on the tongue, which has a whitish-gray or pale pink tint. It protrudes above the surface, swells and peels off.
After rejection of the mucous membrane, a bright red lesion with a rim along the periphery and swelling is formed. After a few days, the epithelization process begins. If the provoking factor acted once (for example, high temperature) or was eliminated, the formation disappears without a trace.
Why does the tongue seem to be burned, causes and treatment?
With subsequent exposure to the provoking factor, lesions form in other parts of the tongue.
Until the moment of epithelialization, the patient notes pain that occurs when eating, discomfort, as well as a disturbance in taste perception. Due to severe swelling of the tongue, diction is impaired.
Peculiarities
Glossitis is an inflammatory disease that develops on the mucous membrane of the tongue. In this case, pathological changes in the mucous membrane occur, it takes on an unusual appearance, and sometimes this process is accompanied by unpleasant sensations.
Discomfort in the oral cavity is the first sign of the development of glossitis
As a rule, glossitis is not an independent disease, but one of the signs of serious disorders in the body. If we talk about Gunter's glossitis, it is one of the symptoms of anemia that occurs due to a lack of vitamin B12 and folic acid in the patient's body.
Changes in the mucous membrane of the tongue during the development of Gunter's glossitis acquire the following features:
- the surface of the tongue becomes very smooth, as if polished;
- the color of the mucous membrane becomes very bright, crimson;
- There may be a slight burning sensation in the mouth.
The papillae of the tongue, mainly in the root zone, become atrophic and smoothed. The mucous membrane of the tongue becomes covered with reddish areas of inflammation, located mainly along the edges and at the tip; aphthous rashes and cracks may appear. Similar changes can occur in the mucous membrane of the gums, cheeks, pharynx, soft palate, and even the esophagus.
In parallel, atrophy of the gastric mucosa is observed, which is most pronounced in the fundus area; the folds of this mucosa become smooth or not defined at all, the walls of the stomach become thinner, and polypous growths may appear on them.
Development occurs gradually; first, symptoms similar to the inflammatory process appear, the tongue becomes scalded or inflamed. Then atrophic processes occur on it, leading to changes in the mucosa, which can subsequently “spread” to the gums, cheeks and other mucous membranes of the mouth and esophagus.
Diagnosis of desquamative glossitis
Diagnosis of the disease begins with a survey of the patient, during which the doctor finds out complaints, data on previous diseases, medical history, dynamics of the pathological process, as well as the effectiveness of the treatment measures.
The oral cavity is examined, the condition of not only the tongue, but also the mucous membrane is assessed, as well as the nature of the saliva and smell. A careful examination of the teeth determines the presence of caries, dental implants, braces, and crowns.
Additional examination methods are prescribed:
- Oral smear using bacterioscopy, polymerase chain reaction, enzyme immunoassay. During the study, it is possible to identify pathogenic flora, specific pathogens, as well as fungi. Microscopy can detect epithelial cells in excess.
- Bacteriological culture of saliva or mucosal scraping. The analysis determines not only the pathogen, but also sensitivity to antibacterial agents. This makes therapy easier by preventing resistance to therapy.
- Ultrasound examination with Doppler scanning. Reduced blood flow in the capillaries by more than 30% indicates dystrophic changes.
Traditional recipes for the treatment of glossitis
Local treatment of the tongue with folk remedies is carried out with the following decoctions and tinctures:
- Chamomile: Chamomile decoction has a wound-healing effect and also disinfects pathological areas. To prepare, you need to pour 1 spoon of chamomile with a glass of boiling water and leave for no more than an hour. Use the prepared broth to rinse the mouth.
- Sage: a natural antiseptic, a decoction of which is well suited for the treatment of glossitis. Patients are recommended to rinse their mouths daily with sage decoction, after leaving it for about an hour.
- Coriander: a decoction of the plant is used as a rinse; it can be used in combination with other folk remedies to enhance the effect.
- Bedstraw: to prepare a decoction you need a standard dose of the plant - one spoon poured with a glass of boiling water. After the decoction is infused, a good natural antiseptic is obtained that promotes wound healing.
Advice! To increase efficiency, it is necessary to simultaneously apply several traditional medicine recipes. For example, rinse your mouth with chamomile and sage on one day, and on the second day prepare a decoction of coriander and basil.
Useful foods for glossitis
In addition to herbs, glossitis can be treated with certain foods: potatoes, horseradish, garlic. Potatoes have an enveloping effect, garlic is a natural antiseptic, and horseradish disinfects and kills some bacteria:
- Freshly squeezed horseradish juice should be diluted with water and boiled, then rinse your mouth with it.
- If your tongue is severely inflamed, it is recommended to hold potato juice in your mouth. You can also finely grate the vegetable and wrap it in gauze, then apply it to your tongue.
Treating inflammation of the tongue at home is ineffective if the cause is unknown. Therefore, you first need to get tested and get a treatment plan from a doctor. Even then, glossitis can be eliminated by combining medications and traditional medicine.
Treatment
Treatment of the disease begins with the joint work of the dentist, as well as related specialists, for example, an allergist, dermatologist, endocrinologist, gastroenterologist.
It is important for the patient to influence the cause of the disease while simultaneously taking symptomatic medications.
In case of pathologies of the oral cavity, it is recommended to sanitation of foci of chronic infection, for example, removal and filling of carious teeth. If implants, crowns or braces are installed incorrectly, they need to be replaced.
It is required to carry out daily oral hygiene with thorough cleaning and rinsing after eating food.
The patient is prescribed a gentle diet, which will reduce the severity of the inflammatory reaction, as well as the manifestations of dysbiosis. It is recommended to eat boiled or baked food. During an exacerbation of the disease, it should have a homogeneous structure and a comfortable temperature.
Of the medicines that are used to treat pathology, the following groups are used:
- Sedatives.
- Antihistamines.
- Vascular.
- Anti-inflammatory drugs.
- Vitamin and mineral complexes.
- Biostimulants.
- Immunomodulators.
Antibiotics and antifungal agents are selected taking into account sensitivity to the identified pathogens. The duration of treatment is determined by the attending physician based on the severity of the disease and the dynamics of the pathological process.
Throughout the entire treatment period, the mouth is rinsed with antiseptic solutions, for example, chlorhexidine or soda.
Unpleasant throat odor: main causes of the symptom
To relieve pain, apply a solution of lidocaine with glycerin or use pyromecaine. In rare cases, with severe pain, a novocaine blockade is placed in the hypoglossal nerve.
At the recovery stage, physiotherapeutic procedures are used, for example, electrophoresis with drugs, ultrasound or SMT therapy. This will improve microcirculation and speed up regenerative processes.
How plaque forms
The oral cavity is home to more than 300 different types of bacteria, which intertwine into complex structures and linger primarily on the surface of the tongue due to the structure of this muscular organ. Larger cells of yeast-like fungi may also be detected on the tongue.
The surface of the tongue is a multilayered thin epithelium that dies when damaged, forming many depressions and protrusions, and is renewed every three days.
The condition of the tongue mucosa is affected by:
- injuries - chemical, mechanical and thermal;
- composition of food (spices irritate the mucous membranes, etc.);
- toxic-allergic effects that can be caused by medications and other factors;
- bad habits;
- various chronic and infectious diseases.
Bacteria and fungi of the oral cavity concentrate and actively multiply on dead cells of the tongue, but the number of microorganisms can fluctuate even within the same topographic zone.
Removal of microorganisms from the surface of the tongue occurs when the cells of the outer layer are exfoliated under the influence of saliva flow, which contains antimicrobial substances, as well as due to the influence of phagocytic microorganisms (neutrophil granulocytes).
The front part of the tongue cleans itself with movements in the oral cavity, and the main part of the plaque is concentrated on the back part of the tongue, since it comes into contact only with the soft palate.
A significant amount of plaque is:
- a consequence of suppression of the activity of normal mechanisms for cleansing the surface of the tongue;
- a sign of a high risk of developing an infectious process, since microorganisms violate the integrity of the epithelium of the tongue and underlying tissues.
Consequences and complications
The chronic course of the disease, as well as frequent relapses, are observed in the absence of therapy, as well as its insufficient effect.
The most common complication is infection. The permanently preserved wound surface acts as an entrance gate. In addition, local immunity decreases, which provokes the growth of pathogenic flora.
In rare cases, atrophic processes in the papillae of the tongue are observed, which leads to disruption of various types of sensitivity.
Recommended video:
Forecast
With timely detection and treatment of desquamative glossitis, the prognosis of the disease is favorable. If the problem is associated with chronic pathologies and occurs in an advanced form, then the likelihood of complete recovery is reduced.
This type of pathology does not threaten the transformation of damaged cells into cancerous ones, but is dangerous due to frequent relapses.
When a problem occurs, there is rarely a clear symptomatic picture that causes the patient to seek professional help. In order to detect the disease in time, it is necessary to regularly examine the mucous membranes of the oral cavity and adhere to hygiene rules.
Forecast and prevention of desquamative glossitis
The disease does not pose a serious threat to the life and health of the patient. The risk of transition to a malignant process is minimal.
In most cases, the prognosis will be favorable, since the pathology can go away on its own. In the absence of therapy, frequent recurrence of the process is possible, which leads to the development of discomfort in the patient.
The main methods to prevent the development of the disease include:
- Timely treatment of identified pathologies. To do this, they correct hormonal levels, restore immunity, and also eliminate diseases of the gastrointestinal tract.
- Carrying out thorough and daily oral hygiene. In addition to brushing your teeth twice a day, you must use dental floss and rinse.
- Timely treatment of diseases of the respiratory and lymphoid system.
- Regular visits to the dentist for therapeutic and preventive purposes. This will allow you to avoid serious illnesses, as well as timely cure pathology in the early stages.
- Normalization of nutrition. To do this, it is important to normalize not only the regime, but also the quality of food consumed. The patient is recommended to adhere to a balanced menu with a moderate temperature regime and a sufficient content of vitamins and minerals. Products that may irritate the mucous membranes of the mouth and tongue are excluded. These include smoked, salted and spicy dishes.
- Elimination of bad habits. Complete cessation of smoking and alcohol consumption will reduce the risk of thermal and chemical burns, as well as restore local immunity.
Patients with signs of desquamative glossitis should seek medical attention. Early diagnosis and identification of the cause of the pathology allows for rapid recovery, reducing the risk of relapse.
Prevention
Glossitis is easier to prevent than to treat. In order to avoid this unpleasant disease you need to follow simple rules.
The first is oral hygiene. This principle applies to both children and adults. If you wash your hands before eating, brush your teeth regularly, do not use someone else’s toothbrushes, and regularly sanitize your mouth, then the risk of developing tongue inflammation is minimal.
Try to avoid damaging the mucous membrane. Avoid eating hard foods that can damage your tongue, such as chips. Hot foods also cause epithelial defects. Spicy foods have an irritating effect. Abuse of them significantly worsens the condition of the tongue mucosa and increases the risk of infection.
Nicotine not only irritates the mucous membrane, but also impairs microcirculation, which reduces the resistance of the epithelium to the effects of infectious agents. Inflammatory diseases of the oral cavity are more common in smokers than in patients who are not adherents of this addiction. Strong alcoholic drinks also have a negative effect on the mucous membranes.
If you have symptoms of glossitis, do not self-medicate, contact a dental clinic. A competent specialist will determine the cause of the disease and prescribe treatment that will help quickly get rid of unpleasant symptoms. Remember, if glossitis is not treated, the disease can lead to serious complications and irreversible consequences.