In endodontic treatment, disinfection of the tooth canals is of key importance. It includes disinfection - the destruction of active microorganisms that cause the disease (pulpitis or periodontitis), and sterilization - a state of complete absence of any bacteria in the root system, including the physiological microflora of the oral cavity.
Root canal irrigation or rinsing with chemical solutions is the most common way to achieve disinfection. The widespread use of this method in dentistry is determined by:
- ease of execution;
- accessibility for every clinic due to the absence of the need for expensive equipment;
- low cost and good results.
The need and importance of sterilization
Sterilization of the root system is a key aspect of endodontic treatment.
It eliminates the cause of the disease - bacteria that entered with saliva through the carious cavity into the tubules of the tooth. Symptomatic therapy for pulpitis (painkillers, anti-inflammatory drugs) only temporarily reduces the manifestations of the disease, after which the acute stage becomes chronic. The microorganisms will continue to multiply in the dental neurovascular bundle and after some time (from 2 weeks to 6 months depending on the state of the patient’s immune system) will cause a relapse of the disease.
With periodontitis, the action of bacteria spreads to the surrounding tissues - the ligamentous apparatus of the tooth, gums, and bone tissue of the jaw. Prescribing antibacterial therapy without disinfection and sterilization of the canals will reduce the population of pathological microflora, but will not completely destroy it. The remaining microorganisms will continue to reproduce. A repeated exacerbation will occur with a decrease in immunity (hypothermia, respiratory disease).
Channel Processing Techniques
Endodontic disinfection methods
There are several methods of endodontic disinfection:
- Chemical by irrigating (rinsing or irrigating) the canals with antiseptic solutions. In dentistry, sodium hypochlorite and chlorhexidine 2% are considered the most effective for root canal treatment.
- Physical sterilization . To carry it out, you need an ultrasonic tip, an endochuck (adapter) and special files.
- Laser disinfection . It is expensive, rarely performed, and has limited indications (allergy to antiseptics).
Hydrogen peroxide
A 3-5% solution of hydrogen peroxide is widely used in endodontics, either alone or in combination with other irrigants, such as sodium hypochlorite. Hydrogen peroxide has an antimicrobial effect, although it is lower than that of hypochlorite. The combination of these solutions manifests itself in the formation of oxygen bubbles, an increase in histolytic activity and a whitening effect.
Research has confirmed that the destruction of Enterococcus faecalis using a combination of hypochlorite and hydrogen peroxide is more effective than using them separately.
We invite you to familiarize yourself with Exercises for developing mobility of the lower jaw
Root canal treatment protocol: disinfection, sterilization, irrigation
How canals are treated in modern dentistry.
Protocol for root canal treatment using the “Step Back” technique
Pulp removal
The pulp is a connective tissue with vessels and nerves, in which 95% of microorganisms that cause inflammation actively reproduce. Extracting the pulp means eliminating most of the factors that caused the disease. A side effect of this stage is the gradual leaching of the organic part from the dentin, which provokes increased fragility of pulpless teeth.
To work at this stage, disposable sterile instruments are used - pulp extractors. They look like a needle with barbs at the end. The dentist places them in the tubules of the tooth (in the thickness of the connective tissue) and removes the neurovascular bundle.
Removing the smear layer
A small part of microorganisms from the pulp penetrates through the dentinal tubules to a thickness of 1-6 microns. Therefore, this part of the canal wall must also be removed by grinding it with H-files. These endodontic instruments are serrated on the working part and have increased flexibility, which prevents them from breaking during operation.
Expansion of the lumen
This stage is necessary for the possibility of further irrigation of the canals and their filling. A narrow canal is difficult to technically process and fill with gutta-percha pins. It is considered optimal to expand the file to 35-40 for incisors and canines and to 30-35 for molars and premolars.
K-Flexoreamer is used for primary treatment and expansion of root canals
Chemical and physical treatment
At this stage, mechanical removal of pulp and dentin particles formed after the root passes through the files occurs, as well as its irrigation and disinfection with antiseptic solutions. For work, special endodontic needles are used - instruments with a flexible tip and a side hole. These technical features allow you to rinse any hard-to-reach canal without causing injury to the periapical tissues or provoking their inflammation after filling.
Physical treatment can be carried out using ultrasonic tips. Low-frequency vibrations destroy the wall of bacteria, causing their death. This method is used in patients who are allergic to chemical antiseptics (hydrogen peroxide, sodium hypochlorite). To work, you need machine endofiles and an endochuck - an adapter for the tip.
Over the past 10 years, the laser method has been used for disinfection in dentistry. A photosensitizer (inactivated solution) is added to the root system and briefly irradiated. A chemical oxidative reaction is triggered, disrupting the integrity of the bacterial membrane.
Root canal irrigation protocols - classic and modified (action time - the duration of the solution after activation)
The laser method is expensive and is currently used to a limited extent - when disinfection is technically impossible (severely curved roots).
Drying cavities
This stage is of great importance for the subsequent stage (filling). Poor execution will lead to leaky filling of the root with paste and gutta-percha. In the resulting voids, after 2-3 weeks, microorganisms will begin to multiply and enter the canal with saliva.
Drying is carried out using sterile paper pins immediately after chemical or physical disinfection. After these two stages, the tooth is filled with therapeutic or permanent material.
Preparation and irrigation of the dental canal
A prerequisite for the procedure is preparation of the canal. During medical intervention, a cavity is formed, which is subjected to sterilization. Preparation involves partial removal of dental tissue, carried out mechanically, and allows you to solve the following problems:
- removal of pathological tissue from the root canal;
- providing an ideal environment for irrigation and sterilization;
- preservation of the natural anatomical structure of the canal;
- prevention of the spread of infectious pathologies;
- maximum possible preservation of the dentin layer.
After mechanical treatment, the doctor must evaluate the quality of the cleaning performed. If it meets the standards, you can move on to irrigation.
The number of solutions used for the procedure varies. Each composition has its own healing functions:
- water - used during mechanical cleaning, allowing you to rinse the oral cavity without causing a negative reaction in the body;
- sodium hypochlorite is a bactericidal composition that effectively removes bacteria and viral pathologies, and whitens enamel;
- hydrogen peroxide - used in combination with the previous solution, improving its disinfecting properties and increasing foaming;
- sodium dichloroisocyanurate – the antibacterial properties of the solution are higher than those of hypochlorite;
- acidic components - phosphoric and citric acid are not highly antiseptic, therefore they are used in combination with other compounds;
- chlorhexedine is the most effective agent against bacteria, but with low dissolving ability, which requires the additional use of hypochlorite.
Modern techniques are used for irrigation. Washing is carried out manually, using ultrasound, sound, laser or hydrodynamics. The most effective method is ultrasonication, during which an antiseptic solution is supplied into the cavity using ultrasound waves.
We suggest you familiarize yourself with it: It makes teeth cramp and makes you feel sick.
An important factor during the procedure is monitoring the temperature of the composition. Overheating of the irrigant causes a negative reaction in the body.
What is needed for sterilization to be effective?
Complete destruction of microorganisms present in the root tubules and periapical tissues is key to effective treatment and the absence of future inflammatory reactions. The following factors are important for high-quality sterilization.
Correct assessment by the doctor of the initially existing pathology
The dentist must correctly diagnose, determine possible complications during treatment and the likelihood of failure. There are clinical cases in which there are a number of negative factors that reduce the success of manipulation to zero. These include:
- pathological periodontal pockets;
- perforation or root fracture;
- vacuum in the area of tooth bifurcation.
The presence of any of these cases reduces the likelihood of effective disinfection of canals by at least 50%; a combination of 2 factors reduces all efforts to nothing.
The doctor also needs to distinguish pulpitis from periodontitis. The latter means infection of the peri-apical tissues of the tooth by pathological microflora, which reduces the effect of treatment.
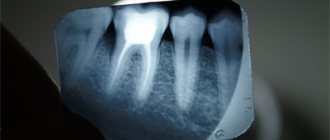
Shape and number of channels
The anatomical structure of the root system is of great importance for successful intervention. The presence of side branches, curved tubules, and their small diameter provoke failures during their passage. High-quality therapy in complex cases (for example, last molars) is not always possible even if the doctor follows all sterilization rules.
Grinding away the top infected layer of dentin
With periodontitis, microorganisms that multiply in the pulp partially penetrate through the dentinal tubules into the thickness of the tooth to a thickness of 2-5 microns. Therefore, to ensure successful treatment, it is necessary to remove this layer with endodontic instruments (H-files).
The correct choice of antiseptic treatment
It matters what irrigation solution is used:
- Distilled water - carries out only mechanical removal of pulp fragments and dentinal filings from the root. After treatment, microorganisms remain in quantities sufficient for reproduction and subsequent apical inflammation.
- Hydrogen peroxide - when interacting with capillary blood, it forms a foam that washes out part of the infected dentin. Antiseptic properties ensure the destruction of microbes by only 50%.
- A solution of 2% Chlorhexidine is a powerful disinfectant. After its use, the death of microflora in the canals varies from 78 to 100%¹, depending on the specific bacterial component.
- Sodium hypochlorite – when used correctly, reduces the risk of post-filling inflammation by 95%. For treatment, it is necessary to heat the solution to 40-45 degrees Celsius, and treat the roots for at least 2 minutes.
Using special instruments for sterilization
High-quality treatment involves the use of endodontic needles. They have a side opening on the working part, which helps to avoid trauma to the apical tissues, as well as reduce the risk of aseptic inflammation after the manipulations.
The correct sequence of manipulations during treatment
The dentist must strictly follow the root canal protocol. You cannot avoid any stage or swap them. For example, after washing with a solution, it is strictly forbidden to “refinish” the walls with endodontic instruments. In this case, microorganisms are carried from the file into the cavity, which means its infection and inflammation of the peri-root tissues in the future.
¹Cantatore, J. Root canal irrigation and its role in cleaning and sterilizing the root canal system Text. / Giuseppe Cantatore // Dentsply News. 2004. - No. 10. - P. 58 - 65.