Drugs used in injection form
Symptomatic and pathogenetic therapy for inflammation of pulmonary tissues includes, in addition to the antibacterial group of pharmacological drugs, also other drugs that can be administered by injection.
However, drugs that directly relate to cough are not used in the form of injections; more often they are introduced into the body by inhalation or orally. These injectable drugs include the following:
- nonsteroidal anti-inflammatory drugs, otherwise known as NSAIDs;
- antiviral medications;
- adaptogens and immunomodulators.
Among NSAIDs, the following drugs are most often used in the treatment of pneumonia:
- Diclofenac - intramuscular injections;
- Nimesil - oral administration for mild pain;
- Analgin with Diphenhydramine, as a lytic mixture for intramuscular administration.
NSAIDs are prescribed as drugs that have an antipyretic effect and anti-inflammatory effect in pneumonia. As part of the treatment of pneumonia in patients of the pediatric age group, Paracetamol with Ibuprofen are used, as they are recognized as the safest.
Nimesil can be used for severe pain syndrome.
Antiviral drugs - interferons and interferon inducers are prescribed for the following diseases:
- viral pneumonia;
- pneumonia of a viral-bacterial nature;
- chlamydial pneumonia;
- pneumonia caused by mycoplasmas;
- ARVI;
- diseases caused by cytomegalovirus.
Antiviral drugs include the following:
- Viferon;
- Grippferon;
- Genferon.
Among the interferon inducers, Cycloferon is prescribed.
There have been no pharmacological studies that could be called authoritative regarding the degree of positive effects of immunomodulators and adaptogens in inflammatory processes of lung tissue. But, they are also prescribed as part of the treatment of pneumonia.
It is generally accepted that aloe extract in ampoules intended for intramuscular administration promotes more rapid healing and restoration of full functionality of lung tissue after inflammation.
What drug is used for pneumonia and in what cases?
There are some basic schemes that are used when prescribing and using certain drugs.
In general, drugs for pneumonia are prescribed as follows and are used in the dosages discussed in the table:
| Drugs that can be prescribed for pneumonia | |
| Drug group | How to use |
| Nonsteroidal anti-inflammatory drugs | Diclofenac is prescribed for severe pain due to pneumonia, as well as for temperatures that exceed 39 degrees. Adults are prescribed 75 mg/day, administered intramuscularly for 5 days. |
| Interferon inducer | Cycloferon is prescribed for pneumonia associated with ARVI, herpes, chlamydia, CMV. Adults are given 10 injections of 0.25 g intramuscularly or intravenously. In childhood, 6-10 mg/kg is indicated, also 10 injections by intramuscular or intravenous administration. |
| Immunomodulator | Imunofan is prescribed for pneumonia that occurs against the background of acute respiratory viral infection, mycoplasma or chlamydial infection, or sepsis. Adults are required to administer 1 time every 3 days, 8 injections are indicated. A single dosage is 50 mcg, that is, 1 ampoule. |
| Adaptogen | Aloe extract is prescribed for any form of pneumonia, with the exception of severe cases. 1 ampoule is used, 1 time per 1 day, the course is 10 injections. |
| Immunomodulator | Polyoxidonium is prescribed for pneumonia caused by acute respiratory viral infections, immunodeficiency, and bronchial obstruction. Administered intramuscularly or intravenously to adults, 6 mg/kg, the powder dissolves in saline or water. 3 are introduced in a row, then an interval of 1 day. A total of 10 injections are required. In childhood, it is administered intranasally from 6 months. |
It is prohibited to independently prescribe any drug to yourself, since their uncontrolled use can lead to a variety of negative consequences, especially for antibacterial and antiviral drugs and NSAIDs.
A specialist will tell you what injections are given for pneumonia. Self-prescription of such medications is unacceptable. The cost of such an impact can be high – at a minimum, a worsening of the patient’s condition caused by inadequate therapy.
The main methods of treatment with the drug cefotaxime for pneumonia
Cefotaxime is a cephalosporin antibacterial drug that belongs to the third generation of drugs.
Most often, tetracyclines or macrolides are chosen for the treatment of chlamydial or mycoplasma pneumonia. Treatment of pneumococcal pneumonia, especially when the pathogenic flora is resistant, with antibacterial agents remains open.
Many experts consider it advisable to prescribe cephalosporins for the treatment of pneumonia - Ceftriaxone and Cefotaxime.
Medicinal properties
A fairly effective and relatively inexpensive drug for the treatment of pulmonary inflammation. The course of treatment of community-acquired infections with antibiotics is prescribed on an individual basis.
It is believed that Cefotaxime is one of the few safe antibacterial agents that, if necessary, can be used even by newborns. As a rule, Cefotaxime is introduced into the patient's body by injection.
Cefotaxime for inflammatory processes in the bronchopulmonary system is effective in cases where the causative agents of pneumonia are the following microorganisms:
- meningococci;
- gonococci;
- streptococci;
- hemophilus influenzae;
- proteus;
- Morganella.
The advantage of Cefotaxime over other drugs with a similar mechanism of action:
- does not have a harmful effect on the liver;
- does not produce bilirubin;
- therapeutic functions are performed in a short time.
In addition, the drug combines well with the use of other medications, and also does not have a harmful effect on the functioning of the gastrointestinal tract, which is typical for other antibacterial agents.
Reference! The therapeutic effectiveness of the drug is so high that it copes even with infections caused by viral pathogens.
The medicine is excreted in the urine after an average of 10 hours, while a small percentage of the active substance is excreted along with bile. The release form of Cefotaxime is glass bottles of 1 g.
Dosage for adults and children
The dosage of the drug depends on how much the inflammatory process has spread in the lungs. If the degree of damage is moderate, it is recommended to take up to 2 grams of the drug once every 12 hours.
Each package contains an insert sheet, which allows you to get acquainted in detail with the methods by which the medicine can be prepared, and, as a rule, calculate the dosage of the drug.
For intravenous administration, it is necessary to dilute 1 gram of powder; the drug must be administered slowly - about 5 minutes. For injection into the muscle, the dosage is the same; the medicinal powder must be diluted in a 1% solution of lidocaine.
When administered by drip, up to 2 grams of powder are diluted in 100 ml of saline or glucose solution (5%). In this case, the product is infused within an hour.
Cefotaxime, if necessary, can be used in infants, as well as in newborns and those born prematurely. The drug is administered intravenously at 50 mg per 1 kg of weight.
IMPORTANT! The course of treatment is prescribed only by a competent doctor, since unauthorized treatment with antibacterial drugs can be fraught with serious complications.
For children over 2 years of age, the drug is administered at a dosage of 50-180 mg per kilogram. If a child is diagnosed with an acute infection, the dosage may be increased to 200 mg per kilogram of weight. 12 grams per day is the maximum dose of the drug in the treatment of children.
Peculiarities
In the first days of treatment, diarrhea may occur, in which case the drug should be discontinued. If patients have atypical allergic reactions to a group of penicillin antibiotics, they may also develop an allergy to cephalosporins.
If long-term use of an antibiotic is necessary, it is necessary to donate blood for control after 10 days. In some cases, during treatment with Cefotaxime, a false positive reaction to the Coombs test and glucose is observed.
While taking Cefotaxime, alcoholic beverages should be strictly prohibited, since in combination with alcohol the drug can provoke tachycardia, nausea, headache, decreased blood pressure, shortness of breath, and stomach cramps.
Despite the minimal impact of the drug on the gastrointestinal tract, during treatment it is recommended to eat fermented milk products containing live bacteria.
During pregnancy and lactation
During the period of bearing a baby, the use of Cefotaxime is allowed, however, it is worth remembering that in the 1st trimester any antibacterial agent is contraindicated, since it is during this period that the formation of fetal systems and organs occurs.
Naturally, the need to take Cefotaxime in the 2nd and 3rd trimester should be determined by the attending physician.
In the course of numerous laboratory tests, experts came to the conclusion that the drug under discussion belongs to category B, that is, drugs that are approved for use during pregnancy.
It must be said that Cefotaxime passes into breast milk, so if treatment with this drug is necessary during lactation, breastfeeding should be discontinued. This is due to the fact that the concentration of the active substance in breast milk will have a negative effect on the fragile microflora of the infant.
Contraindications
The drug is contraindicated in:
- allergic manifestations and intolerance to the active substance or components of the drug;
- in the 1st trimester of pregnancy;
- bleeding;
- acute form of colitis;
- enterocolitis.
The drug should be prescribed with caution to patients with severe kidney and liver diseases.
Side effects
As for the side effects that can be caused by Cefotaxime, they are as follows:
- allergies – rash, fever, angioedema;
- pain in the epigastric region, vomiting, bowel dysfunction, colitis, jaundice;
- changes in blood composition are possible;
- headache;
- unpleasant and painful sensations at the site of skin puncture;
- interstitial nephritis;
- hemolytic type anemia.
If adverse reactions occur, you must stop taking the drug and inform your doctor.
Overdose
An overdose of a drug may manifest itself:
- tremor of the limbs;
- convulsions;
- feverish condition;
- temporary loss or partial decrease in hearing;
- impaired coordination of movements;
- With kidney disease, encephalopathy may develop.
Such symptoms require immediate medical attention.
Combination with other drugs
Unlike similar antibacterial drugs, Cefotaxime reacts quite calmly when combined with other drugs. However, this case also has its own characteristics.
The prescription of potentially nephrotoxic drugs - aminoglycosides, Furosemide - should be accompanied by monitoring of kidney function, since a nephrotoxic effect is possible.
Under no circumstances should Cefotaxime be mixed with other drugs in the same dropper or syringe.
Since the drug suppresses the activity of intestinal flora and interferes with the normal synthesis of vitamin K, it is not recommended to be used simultaneously with drugs that reduce platelet aggregation. In this regard, the drug should not be used together with anticoagulant drugs, since the effect of the latter will be enhanced.
If Cefotaxime is used simultaneously with drugs that affect tubular secretion, the concentration of the antibiotic in the blood will increase. Probenecid helps slow down the removal of the antibacterial agent from the body.
Analogs
Analogs of Cefotaxime are presented in a fairly wide list, the most common of them are given below:
- Clofaran;
- Cefosin;
- Cefantral.
As for oral forms, there are none, since the drug is available only in the form of injections, but there are drugs that have a similar mechanism of action:
- Pantsef;
- Suprax;
- Ixim Lupine;
- Zinnat;
- Aksosef.
Check out visually about antibiotics in the treatment of pneumonia in the video below:
Cefotaxime is considered a very effective new generation antibacterial agent, and in a short time allows you to get rid of infectious lung lesions.
In this regard, specialists quite often prescribe this drug for pneumonia, and it must be said that this choice is not always made rationally.
It is advisable to avoid taking such strong drugs, especially in childhood and old age, and if possible, use less serious treatments, since the stronger the drug used, the worse it affects the functioning of the immune system.
Source: https://med-kurator.com/organy-dyhaniya/pnevmoniya/antibiotiki/tsefotaksim.html
Lung damage by coronavirus
The family of coronaviruses has been known to science for >50 years and consists of 43 types of RNA-containing strains. The culprit of the current epidemic is a new strain of coronavirus SARS-CoV-2. The virus differs from its “closest relatives” in its high rates of contagiousness and virulence, that is, its ability to be transmitted and spread within the body. The crown-shaped spikes located on the surface of the microorganism contain the coding protein Spike, which mimics beneficial proteins. Invasion of the virus into human cells does not occur through the membrane, but through transmembrane receptors that do not differentiate the Spike protein as an agent foreign to the body.
The receptors themselves anchor the protein to the membrane, and SARS-CoV-2 pushes its RNA into the cytoplasm of cells for further replication. The coronavirus manages to deceive the immune system and occupy the upper respiratory tract. At the next stage, the virions move into the lower respiratory tract. Diffuse inflammatory damage to the alveoli develops, in which, instead of air, exudate saturated with viral proteins accumulates, preventing the gas exchange of oxygen and carbon dioxide. Against the background of a weakened immune system due to a viral infection, opportunistic staphylococci are activated. Through damage to cell membranes, bacteria penetrate into the lung tissue, aggravating the course of the infection. Thus, the development of covid pneumonia occurs in stages:
- Coronavirus infection.
- Increased permeability of cell membranes, and invasion of virions into the lungs.
- Accumulation of fluid in the alveoli.
- Attachment of a bacterial infection.
Due to gas exchange disrupted by bacterial-viral invasion, acute respiratory distress syndrome (ARDS) and respiratory failure develop. In addition to severe pulmonary disease, patients experience autoimmune reactions. The immune system does not differentiate its cells from infectious agents, and begins to destroy the body to which it belongs.
Choice of antibiotic for pneumonia, bronchitis, sinusitis
Acute rhinitis (runny nose) involving the sinuses (rhinosinusitis) is the most common infection in humans. In most cases it is caused by viruses. Therefore, it is not recommended to take antibiotics for acute rhinosinusitis in the first 7 days of illness. Symptomatic remedies, decongestants (drops and sprays for the common cold) are used.
Antibiotics are prescribed in the following situations:
- ineffectiveness of other remedies during the week;
- severe course of the disease (purulent discharge, pain in the facial area, or when chewing);
- exacerbation of chronic sinusitis;
- complications of the disease.
For rhinosinusitis, amoxicillin or its combination with clavulanic acid is prescribed. If these drugs are ineffective within 7 days, it is recommended to use cephalosporins of the II – III generations.
Acute bronchitis is most often caused by viruses. Antibiotics for bronchitis are prescribed only in the following situations:
- purulent sputum;
- increased volume of expectorated sputum;
- the appearance and increase of shortness of breath;
- increasing intoxication - deterioration of condition, headache, nausea, fever.
The drugs of choice are amoxicillin or its combination with clavulanic acid; cephalosporins of the second and third generations are used less frequently.
Antibiotics for pneumonia are prescribed to the vast majority of patients. In people under 60 years of age, preference is given to amoxicillin, and if they are intolerant or suspected of having a mycoplasma or chlamydial nature of the pathology, macrolides are preferred. In patients over 60 years of age, inhibitor-protected penicillins or cefuroxime are prescribed. During hospitalization, treatment is recommended to begin with intramuscular or intravenous administration of these drugs.
For exacerbation of COPD, amoxicillin in combination with clavulanic acid, macrolides, and second-generation cephalosporins are usually prescribed.
In more severe cases of bacterial pneumonia, severe purulent processes in the bronchi, modern antibiotics are prescribed - respiratory fluoroquinolones or carbapenems. If a patient is diagnosed with nosocomial pneumonia, aminoglycosides, third generation cephalosporins can be prescribed, and for anaerobic flora - metronidazole.
Below we will look at the main groups of antibiotics used for pneumonia, indicate their international and trade names, as well as the main side effects and contraindications.
How long does it take to treat pneumonia?
Before you find out how much pneumonia is treated in adults and children, you need to understand that this pathology greatly affects the lungs and soft tissues of the organ. Inflammation and tissue destruction occurs. A person of any age and social status can become infected.
Attention! Self-medication is excluded. This can lead to even more health problems and early death.
There are points that affect the duration of treatment for pneumonia. Here are the main ones:
- the nature of the pathogen;
- general health and age of the patient;
- correct diagnosis, establishment of the degree of pathology, the complexity of its course;
- prescribing effective medications;
- reaction to antibacterial therapy;
- the presence of concomitant diseases, including chronic ones.
It is important to know not only how much pneumonia is treated in children and adults, but also that the effectiveness of therapy must be determined. Here are the main criteria for the adequacy of treatment:
- negative dynamics on an x-ray;
- body temperature no more than 37.5 °C;
- absence of respiratory failure, purulent sputum;
- the volume of blood leukocytes is up to 10x109/l.
Many people want to know whether sick leave is issued for pneumonia and for how many days. Here a lot depends on the severity of the condition in which the person is. Thus, the document can be provided for a period of 17 to 28 days. In particularly difficult cases, treatment is extended for 1.5 months or more.
Pneumonia is caused by rotavirus infection, fungi or bacteria. Consequently, the disease is transmitted by airborne droplets, so sick leave for pneumonia is mandatory. It is important to isolate a person from society.
Duration of treatment for pneumonia in hospital
Pneumonia of moderate, severe and severe forms with complications (septic shock, sepsis, abscess) is treated only in a hospital setting. The patient is given IVs and given injections. The course lasts on average from 16 to 28 days. Additional treatment at home is possible.
Attention! A treatment regimen for pneumonia (pneumonia) should be developed by a highly specialized pulmonologist. The recovery period largely depends on this.
Duration of treatment for pneumonia on an outpatient basis
Many people want to know what pneumonia is and how long it can be treated at home. Such therapy is possible only for mild forms of the disease. In this case, the course takes 14-16 days.
It is important that relatives surround the patient with care. More often, oral medications, ointments, breathing exercises, and sometimes injections are prescribed.
Attention! The doctor will advise on all important issues.
Duration of antibiotic use
Many people want to know how long it takes to treat pneumonia with antibiotics. Most patients take such medications for 7 days. The exact period depends on the severity of the pathology. For a moderate form, therapy can last 10 days, for a severe form - 20 days.
The nature of the pathogen is of great importance. When the disease occurs under the influence of pneumococcus, you need to take antibiotics for 5 days. For legionella and staphylococcal forms, these drugs must be taken within 21 days. The course can last up to 42 days for Pseudomonas aeruginosa or enterobacteria, and up to 56 days for lung abscess.
Groups of patients with pneumonia and treatment
According to the modern classification, pneumonia can be hospital-acquired, which a person received while in the hospital, and non-hospital, which is much more common.
It is very important to inoculate the pathogen; based on the information received, a medicine is prescribed, and the sensitivity of the microorganisms is determined
However, it will take at least 2 days to get answers to your questions. Naturally, doctors don’t have that much time; pills are prescribed empirically, or at random. But for more correct prescription, all patients should be divided into 4 groups, each with its own drugs.
First group
This group includes people whose pneumonia is not severe, and there are no concomitant pathologies or additional risk factors. When determining the pathogen, it is difficult to obtain a result, but a person can be treated on an outpatient basis, in a clinic. The causative agents may be:
- streptococcus;
- mycoplasma;
- Klebsiella
In this regard, broad-spectrum drugs are prescribed. This group includes:
- aminopenicillins, of which amoxicillin is a representative;
- macrolides, which make up azithromycin, josamycin, clarithromycin.
If it is not possible to take the medicine described above for one reason or another, taking second-line drugs is indicated. These include respiratory fluoroquinolones, of which ciprofloxacin is a prominent representative. This drug can be produced under different names and is contained in tablets “Tsiprolet”, “Tsiprinol”, “Tsiprobay”; moxifloxacin is also used in the form of the drug “Avelox”.
In the case when the previously used amoxicillin does not have a positive result for 2-3 days, the inflammation does not go away, it should be replaced with a macrolide. The dosage of tablets is selected by the doctor individually.
Second group of patients
This category includes patients who have mild pneumonia, but have severe concomitant pathology. This may include COPD (chronic obstructive pulmonary disease), diabetes mellitus, heart failure, kidney failure, cancer, chronic liver disease, cerebral vascular pathology, and mental disorders.
With this type of pneumonia, the most likely cause may be streptococcus, and in elderly people, E. coli and Klebsiella. Crops may also be pointless. But against the background of reduced immunity, the health condition may worsen and the person may end up in the department.
In this situation, the doctor decides which tablets to use. The drugs of choice in this situation are protected aminopenicillins. Representatives of this group are:
- Augmentin;
- Flemoklav solutab;
- Amoxil-K.
Also, for pneumonia in this category of patients, second generation cephalosporins are used - cefuroxime in the form of drugs Axef, Zinnat, Zinacef, Cefutil. If the treatment is ineffective, third or fourth generation fluoroquinolones are indicated.
In cases where the tablets do not have a positive effect for pneumonia, intramuscular administration of third-generation cephalosporin antibiotics in the form of the drug Ceftriaxone is indicated.
In a situation where protected aminopenicillins are not effective, tablets of the macrolide group are prescribed or all are replaced with fluoroquinolones.
Patients of the third group
In this category, pneumonia has a moderate course. In this variant, the causative agent is not only streptococcus, but also Haemophilus influenzae, chlamydia, Legionella, Escherichia coli, and Klebsiella. In some cases, the pathogen is not one, but is combined with others, forming a mixed or mixed infection.
Fourth group
In this category of patients, the inflammatory process in the lungs is severe and is accompanied by severe intoxication. The pathogens in this category are considered to be microorganisms that were described earlier, but Staphylococcus aureus, Mycoplasma or Pseudomonas aeruginosa can additionally join. The person should be hospitalized in a department, most often in intensive care.
The duration of treatment is from 3 to 10 days; in especially severe cases, inflammation in the lungs is treated for 3 weeks.
Treatment of patients with non-severe pneumonia
Usually, with bronchitis and pneumonia of this severity, the patient is on sick leave and follows the doctor’s recommendations at home. Pneumonia can usually be cured with oral medications without the use of injectable forms, that is, in tablets, capsules, suspensions.
Patients over 60 years of age receive one of the β-lactam antibiotics as treatment:
| Active substance | Method of application, price |
Penicillins:
| Amoxicillin (tablets): 0.5 g. x 2 times a day orally for 14 days. 39-70 rub. |
| Flemoxin Solutab (tablets): 0.5 g. x 2 times a day orally for 14 days. 390-530 rub. | |
Amosin:
| |
Macrolides:
| Azitral (capsules): 0.25/0.5 g. once a day before or 2 hours after meals. 280-330 rub. |
Sumamed:
| |
Azitrox:
| |
| Klacid:
|
| Clarithromycin Teva (tablets): 0.25 g. twice a day for 1 week. 380-530 rub. | |
| Fromilid (tablets): 0.5 g. twice a day for a course of 2 weeks. 290-680 rub. |
For patients 60 years of age and older, protected penicillins and fluoroquinolones are suitable in combination with concomitant pathology (or without it):
| Active substance | Method of application, price |
Protected penicillins:
| Amoxiclav:
|
Augmentin:
| |
| Flemoclav Solutab (tablets): 1 tablet (500+125 mg, respectively) three times a day or 1 tablet (875+125 mg, respectively) twice a day, without chewing at the beginning of meals, for a course of 2 weeks. 300-450 rub. | |
Respiratory fluoroquinolones:
| Tavanik (tablets): 0.25 g. x 2 tablets x 2 times a day or 0.5 g. x 1 tablet x 1 time per day, washed down with water, course 2 weeks. 460-1000 rub. |
| Floracid (tablets): 0.5 g. twice a day, without chewing, between meals. 300-800 rub. | |
| Avelox (tablets): 0.4 g. x 1 time per day, without chewing, course 2 weeks. 220-380 rub. |
| Moflaxia (tablets): the dosage regimen is similar. 320-350 rub. |
Respiratory fluoroquinolones remain the best antibiotics for pneumonia at the 2nd stage of its treatment. They are connected if there are no signs of effectiveness of the first drug used. Representatives of this group are distinguished by a greater spectrum of action and less resistance of microbes. However, each case is individual.
What antibiotics are used for pneumonia?
As mentioned above, antibiotics for pneumonia are initially prescribed from the general spectrum or, as they are called, first line, and after receiving all the necessary examination results, the last generation. The variety of drugs available today allows you to choose the appropriate medication for each individual case. This choice is influenced by many factors: from the age of the patient and his individual characteristics of the body to the nature of the manifestation of the disease and the source of its occurrence.
Antibiotics for pneumonia in adults
The choice of groups of antibiotics for pneumonia is determined taking into account the individual characteristics of the organism
There are several main groups of antibiotics for pneumonia in adults. The choice of a drug of one group or another is made by a doctor:
- Amoxicillin. Medicines: Amoxicillin, Flemoxin Solutab, Ospamox. Used for uncomplicated variants of the disease. The course usually lasts at least 10-12 days. These drugs are powerless against bacteria that produce beta-lactamase;
- Amoxicillin in combination with clavulanic acid. Medicines: Amoxiclav, Augmentin. This group contains low-toxic antibiotics that can resist the destructive effects of beta-lactamase. This property ensures the presence of clavulanic acid in them;
- Macrolides. Drugs: Erythromycin, Azithromycin, Sumamed, Macropen. They are a good replacement for the penicillin series. Particularly effective for the manifestation of atypical pneumonia caused by the bacteria chlamydia, mycoplasma, and legionella. They are also characterized by low toxicity;
- Cephalospirins. Drugs: Cephabol, Ceftriaxone, Cefizolin, Suprax. This list of medications is used for pneumonia caused by streptococci, pneumococci or enterobacteria. But Clessibela and E. coli have good resistance to them;
- Fluoroquinolones. Drugs: Levofloxacin, Sparfloxacin. These medications have a strong effect on pneumococci.
Since in the treatment of pneumonia, in some cases, several antibiotics may be prescribed at once, it is important to monitor their compatibility.
Antibiotics for pneumonia in children
Antibiotics for pneumonia for children should also be started as soon as the disease is diagnosed. Despite the fact that it is desirable for a child’s body not to come into frequent contact with antibiotics, in this case there is no alternative. But the acceptable list of drugs is shorter than for adults.
For children, antibiotics for pneumonia are prescribed immediately after diagnosis.
Children are usually prescribed natural and synthetic penicillin antibiotics. Among them are drugs such as Augmentin, Amoxiclav, Ampicillin, Flemoxin Solutab, Cefix. All of them are allowed for use in children due to their low toxicity. The dosage in this case is determined taking into account the child’s body weight, and the method of administration is determined by the patient’s age and the severity of the disease. Treatment is often prescribed with intramuscular injections of anti-inflammatory antibiotics, and as soon as positive dynamics appear, the injections are replaced with tablets.
Pharmacological groups
For infectious and inflammatory processes, antimicrobial agents are used:
- Bactericidal action aimed at eradicating the pathogen.
- Bacteriostatic – blocking the production of proteins and DNA replication of pathogens.
Medicines are grouped by pharmacodynamics and similar chemical structure. General contraindications for use are renal and hepatic decompensation, perinatal and lactation periods in women, allergies.
For antibacterial therapy of the respiratory system, six main pharmacological groups are indicated:
- Penicillins (natural and semi-synthetic). Long-term use of natural first-generation penicillins has led to the development of resistance and adaptation of pathogens to Penicillin, Benzylpenicillin, Bicillin. The bactericidal properties of semisynthetic penicillins are used in the treatment of ambulatory pneumonia caused by gram-positive bacteria and certain strains of gram-negative pathogens. New penicillins are recognized as the most effective antibiotics for pneumonia in children. In pediatrics, the drugs of choice are Flemoxin, Mezlocillin, Amoxicillin (for children). Strict contraindications for use are the parallel course of aspirin-induced bronchial asthma, Filatov's disease (infectious mononucleosis) and lymphocytic leukemia.
- Cephalosporins . They represent five generations of the closest “relatives” of penicillins. The bactericidal effect of generation I and II is limited due to resistance to β-lactamases (enzymes produced by microbes). Medicines are considered outdated and are rarely used in clinical practice. III and IV generations of cephalosporins destroy pneumococci, staphylococci, Pseudomonas aeruginosa and Haemophilus influenzae, Proteus. Prescribed for aspiration, nosocomial infection of unilateral and bilateral type, of moderate severity. The fifth generation of cephalosporins kills Klebsiella pathogens, bacterial infections gram (+) and gram (-).
- Macrolides . Bacteriostatics of natural and semi-synthetic origin, with a complex chemical structure. In concentrated doses, the bacteriostatic effect is replaced by a bactericidal one. They stop the growth and reproduction of mycoplasma prokaryotes, protozoan intracellular parasites, bacterial strains gram (+) and gram (-). At the same time, they exhibit moderate immunomodulatory activity. Used for outpatient pneumonia of moderate and severe course with bilateral, total damage to the lung tissue. Currently, macrolides are considered the most effective antibiotics for pneumonia in adults. Contraindicated for children under six months of age. Some tablets are approved for use in women during the perinatal period, but are prohibited during lactation.
- Fluoroquinolones . 100% synthetic drugs. There are no similar natural compounds. The most powerful bacteriostatics against gram (+) and gram (-) strains. Indicated for community-acquired inflammation of the respiratory system with a complicated course and moderate severity. The disadvantage of fluoroquinolones is an extensive list of contraindications, including childhood. The first generation of drugs is not used in pulmonology.
- Aminoglycosides . Natural and laboratory-generated compounds. Destroys gram-positive cocci, Klebsiella, enterococci. In pulmonology, the second generation of aminoglycosides is used to a limited extent in case of a total allergic reaction of the patient to antimicrobial drugs of other pharmacological groups. Aminoglycosides are characterized by nephrotoxicity and increased teratogenicity. Strictly contraindicated for renal pathologies and pregnancy.
- Carbapenems . They are used as a reserve for the most effective antibiotics of the latest generation for pneumonia in adults. Indicated for severe pulmonary pathologies (in-hospital and community-acquired origin), accompanied by the threat of respiratory failure and mortality.
Second-tier drugs:
- Monobactams. Synthetic compounds with a narrow spectrum of action against aerobic gram-negative microorganisms. They do not work against gram (+) strains. Prescribed for uncomplicated Klebsiella infection, for patients with hypersensitivity to cephalosporins, aminoglycosides, fluoroquinolones, macrolides. One drug used in clinical practice is Aztreonam.
- Lincosamides. Bacteriostatics of staphylococci, streptococci, complementing the main antibiotic therapy. Representatives of lincosamides are Lincomycin, Clindamycin.
- Tetracyclines. The bacteriostatic activity of Tetracycline and Doxycycline against prokaryotes is used in correlation with macrolides and cephalosporins for mycoplasma invasion.
Antibiotics are produced in the form of capsules, tablets, ampoules with a ready-made solution, suspensions, granules, and lyophilisate powder for the preparation of an injection solution. The dosage, regimen, and duration of administration are determined by a therapist or pulmonologist (according to the severity and nature of the inflammatory process).
Prescribed drugs
The list of effective drugs used for covid pneumonia includes:
- Sumamed (500 mg). Macrolide bacteriostatic with active azithromycin dihydrate. The standard regimen is taken once a day for three days. For coronavirus, the course of use is increased 2-3 times, with parallel administration of cephalosporin injections. The therapeutic concentration lasts up to 7 days after taking the last dose. Produced in Croatia. Structural substitutes are Serbian Hemomycin and Russian Azithromycin.
- Tavanic (500 mg). Representative of the group of respiratory fluoroquinolones based on levofloxacin. Quickly penetrates the affected lung tissue and stops the synthesis of bacterial proteins. Prescribed once a day, from 5 to 10 days. In clinical practice, coronavirus pneumonia is used to consolidate the antimicrobial effect after a shock course of basic antibiotics. Produced in Ukraine. Drugs identical in structure - Levofloxacin, Levoflox, Eleflox.
- Ceftriaxone. III generation cephalosporin with high bactericidal activity. Effectively eliminates pathogenic and conditionally pathogenic microorganisms. The recommended dose is two injections per day, at intervals of 12 hours, for 10-14 days. For severe infectious and inflammatory diseases, including COVID-19, the dosage or duration of the injection course may be increased. Manufactured by pharmaceutical companies in Russia, Ukraine, and India. Analogs for the active substance are Ceftriabol (Russian Federation), Rocephin (Switzerland), Lendatsin (Slovenia).
- Cefotaxime. Cephalosporin antibiotic made in India. Belongs to the III generation. In terms of pharmacodynamics, it differs little from Ceftriaxone. Method of administration: injection, twice a day. Russian products similar in chemical structure are Cefosin, Cephabol.
- Zinforo. The newest bactericidal cephalosporin antibiotic of the V generation. The active ingredient is ceftaroline fosamil. Supplemented with L-arginine (amino acid). In pulmonology it is used for the treatment of community-acquired and nosocomial pneumonia. It is administered infusionally, intravenously, in a hospital setting. The course of treatment takes 10-14 days. Country of origin: Great Britain.
What antibiotics should I take for coronavirus and pneumonia? Only those prescribed by the doctor! Covid pneumonia is an unpredictable infection that is life-threatening. Self-medication threatens fibrosis of the lung tissue, the development of ARDS, hypoxemia (oxygen deficiency), and death.
Category:
Articles
Posted by Andrey Titov
General practitioner, 10 years of experience. Education: 2005 St. Petersburg State Medical University named after. acad. I.P. Pavlova (medicine). 2012 St. Petersburg State Medical University named after. acad. I.P. Pavlova (general practitioner).
Antibiotic treatment of pneumonia in adults according to the type of pathogen
The most dangerous forms of lung damage are considered to be infections caused by streptococci and legionella (Legionella disease).
The mortality rate from these types of pneumonia is 48 percent of all registered deaths.
Antibiotics for pneumonia should be prescribed from the first day of diagnosis.
After receiving the results of bacteriological culture, the treatment regimen is adjusted taking into account the identified pathogen.
What drugs are prescribed to patients for various harmful agents?
| Type of pathogen (representative of pathogenic flora) | Antibiotics used for treatment |
| Haemophilus influenzae | "Amoxicillin", "Amoxiclav", "Aminopenicillin". |
| Legionella | Erythromycin, macrolides, fluoroquinolones, rifampicin. |
| Streptococcus | Benzylpenicillin, third generation cephalosporins (Ceftriaxone), aminopenicillin, macrolides |
| Klebsiella and Escherichia coli | Third generation cephalosporins |
| Staphylococcus | Oxacillin, aminopenicillin, first and second generation cephalosporins |
| Mycoplasma, chlamydia | Tetracycline, macrolides, fluoroquinolones |
The duration of treatment is 10-14 days - during this period, a sufficient amount of components with biological activity accumulates in the blood, and pathogenic flora is destroyed.
If there is no therapeutic effect, the drug is replaced on the 3-4th day of treatment (if necessary, the dose or dosage regimen is adjusted).
Antibacterial therapy of pneumonia in adults
The development of the inflammatory process is caused by microorganisms that make up the pathogenic flora (staphylococcus, mycoplasma, trichomonas, etc.), so treatment involves taking antibiotics.
In order for therapy to be effective, it is necessary to determine the type of pathogen and its sensitivity to various groups of antibacterial agents.
To do this, a laboratory test of the sputum is performed.
Bacteriological seeding allows us to identify which bacteria will begin to actively grow and form colonies.
The test takes at least 10 days to complete. A patient does not have that amount of time when diagnosing pneumonia.
Therefore, treatment begins with the use of broad-spectrum antibiotics.
The choice of drug depends on many factors, for example:
- the patient’s condition at the time of admission to the hospital;
- age;
- existing chronic diseases or previous infections (diabetes mellitus, tuberculosis, sepsis, etc.);
- bad habits (in particular, smoking), etc.
Antibiotics are prescribed for a period of at least 3-5 days - during this time the required concentration of active components is achieved in the blood, sufficient to destroy pathogenic flora.
Antibiotics for pneumonia: how to choose the best drug - Website about
Treatment of pneumonia is carried out mainly in a hospital setting. In some situations (for example, with the development of respiratory failure), resuscitation measures may be required, so staying at home after establishing and confirming the diagnosis is unacceptable, especially if we are talking about severe forms of pneumonia: bilateral, congestive, streptococcal or klebsiella. Antibiotics for pneumonia are the basic basis for treatment tactics for patients of any age and with any form of diagnosis. Selecting an effective drug for a pulmonary infection is a very difficult task, since all drugs have varying degrees of activity against harmful organisms (infectious agents). In some cases, you have to wait more than 10 days for the results of a special sensitivity test. Such a period can cost the patient his life, so it is important to know the basics of antibacterial therapy in order to provide the patient with the necessary assistance and begin treatment at the initial stage.
What antibiotics are effective for pneumonia? | Asthmania
Pneumonia is a disease that occurs as an inflammatory process localized in the lung tissue.
Methods of using antibiotics
For treatment of pneumonia with antibiotics to be successful , it is necessary to use them correctly. Antibacterial drugs are administered to adults in different ways: orally, intramuscularly, inhalation, intravenously.
For the treatment of pneumonia, antibiotics are administered to infants parenterally , bypassing the digestive system, otherwise the microflora of the stomach and intestines may have a detrimental effect. Antibacterial drugs are administered by injection or inhalation. The most important thing is that children under 6 months are treated in a hospital under 24-hour medical supervision.
For adults, different antibiotics for pneumonia are administered in different ways:
- If the disease is very severe, penicillin antibiotics are administered intravenously in the first two days, then intramuscularly. In this case, the transition from one form of drug administration to another is called a “stepped” course of treatment.
- Due to their low toxicity, cephalosporins can be administered intravenously and intramuscularly. They often replace penicillin if the patient is hypersensitive to this antibiotic.
- Macrolides do an excellent job against staphylococci, corynebacteria, streptococci and pneumococci. This drug continues to act even after its withdrawal, having sufficiently accumulated in the lung tissues.
- In the hospital, if the causative agent of pneumonia has not been identified, aminoglycosides and fluoroquinyls are used, both individually and in combination with each other. The effect will be the same.
If pneumonia occurs in mild or moderate form without complications, the correctly chosen antibacterial drug helps to completely recover from this disease in 10 days. Pneumonia caused by mycoplasma, legionella or chlamydia is treated for about a month until complete recovery.
Is Ceftriaxone always possible for coronavirus and pneumonia?
Ceftriaxone for coronavirus is indicated for signs of bacterial pneumonia:
- chest pain on one side;
- asymmetrical wheezing;
- discharge of yellowish sputum;
- enlarged lymph nodes;
- In the blood test, leukocytes are elevated, there is a shift in the leukocyte formula to the left, high ESR and procalcitonin.
The antibiotic is not suitable for treatment at home (for mild forms of coronavirus); it is not prescribed for prophylactic purposes. Therefore, there is no point in administering it without a doctor’s prescription, this can only worsen the condition, lead to a more severe course of pneumonia; with unreasonable use, resistance to Ceftriaxone develops, and then it does not help when really necessary.
The medication is not recommended for patients when there is reason to assume that this drug is ineffective:
- less than 3 months before the illness there was already a course of treatment with Ceftriaxone;
- chronic inflammatory processes in the bronchi and lungs;
- recent injury, surgery;
- stay in nursing homes, closed boarding schools;
- the presence of a permanent catheter in a vein (for example, when an artificial kidney is connected to the machine).
For these groups of patients, other treatment regimens are chosen. Ceftriaxone may be discontinued after sputum culture results are obtained if the infectious agent is found to be resistant to this antibiotic.
Restrictions for use include:
- renal and/or liver failure;
- nonspecific ulcerative colitis;
- exacerbation of inflammation in the organs of the digestive system, especially the biliary tract and intestines.
An absolute contraindication includes an allergy to this antibiotic or another from the group of cephalosporins (for example, Cefotaxime, Cephalexin) or the penicillin series (a cross-allergic reaction is possible).
When is it prescribed?
As mentioned above, Augmentin is used in the treatment of various bacterial infectious diseases, a huge proportion of which are respiratory tract diseases. This drug successfully helps in the fight against bronchitis, laryngitis, and tracheitis. It is also taken in the treatment of one of the most dangerous diseases, the name of which is pneumonia.
If left untreated, pneumonia can lead to death, since it does not have a chronic form. While people did not know about the existence of antibiotics, pneumonia took many lives. But thanks to antibacterial agents, it is now possible to cure almost all types of pneumonia and, in most cases, avoid any complications. Both adults and children can take Augmentin for pneumonia.
Bacteria that can provoke an inflammatory process in the tissues of the lungs in the vast majority of cases enter the human body through airborne droplets, sometimes through the blood. It should be noted that pneumonia rarely appears on its own; it usually occurs as a complication in a chain of respiratory diseases or develops against a background of weakened immunity or general weakness of the body caused by other diseases.
In its most complex form, pneumonia occurs in older people and young children. Very often, Augmentin is prescribed to children with pneumonia by doctors.
As a rule, pneumonia makes itself felt with a dry cough that turns into a wet one, elevated body temperature, weakness and pain in the chest. Therefore, when these symptoms appear, it is necessary to undergo an examination in order to begin treatment in a timely manner. Pneumonia is diagnosed using X-ray examination.
Pneumonia is most often caused by streptococci, which are effectively combated by antibiotics of the aminopenicillin group. They are the easiest for humans in terms of their toxic effects on the body, but at the same time they are very effective. They are also capable of killing pneumococci, which also often provoke pneumonia. It is not difficult to cure pneumonia with Augmentin if the disease is diagnosed at an early stage.
The drug Augmentin also belongs to the aminopenicillin group of antibiotics. As mentioned, this medicine is a combination of amoxicillin and clavulanic acid. The second component does not allow beta-lactamases to influence the first, thus, it retains its maximum effectiveness in the fight against pathogenic bacteria. Medicines containing clavulanic acid are usually necessary for patients already undergoing antibiotic therapy. Pneumonia can be treated well with this substance.
How does Augmentin work on the body? The amoxicillin it contains destroys the cell walls of pathogenic microorganisms, thus destroying bacteria and eliminating diseases such as pneumonia.
Respiratory fluoroquinolones are the most effective antibiotics for pneumonia
Antibiotics from the fluoroquinolone group are very often used in medicine. A special subgroup of these drugs has been created, which is especially active against pathogens of respiratory tract infections. These are respiratory fluoroquinolones:
- levofloxacin (Ashlev, Glevo, Ivacin, Lebel, Levoximed, Levolet R, Levostar, Levotek, Levoflox, Levofloxabol, Leobeg, Leflobakt Forte, Lefoksin, Maklevo, Od-Levox, Remedia, Signicef, Tavanik, Tanflomed, Flexid, Floracid, Hyleflox, Ecolevid, Eleflox);
- moxifloxacin (Avelox, Aquamox, Alvelon-MF, Megaflox, Moximac, Moxin, Moxispenser, Plevilox, Simoflox, Ultramox, Hynemox).
These antibiotics act on most pathogens of bronchopulmonary diseases. They are available in tablet form and also for intravenous use. These drugs are prescribed once a day for acute sinusitis, exacerbation of bronchitis or community-acquired pneumonia, but only if other drugs are ineffective. This is due to the need to maintain the sensitivity of microorganisms to powerful antibiotics, without “shooting sparrows with a cannon.”
These drugs are highly effective, but their list of possible side effects is more extensive:
- candidiasis;
- inhibition of hematopoiesis, anemia, bleeding;
- skin rash and itching;
- increased blood lipid levels;
- anxiety, agitation;
- dizziness, sensory disturbances, headache;
- deterioration of vision and hearing;
- heart rhythm disturbances;
- nausea, diarrhea, vomiting, abdominal pain;
- pain in muscles and joints;
- decreased blood pressure;
- swelling;
- convulsions and others.
Respiratory fluoroquinolones should not be used in patients with prolongation of the QT interval on the ECG, which may cause life-threatening arrhythmias. Other contraindications:
- previous treatment with quinolones that caused tendon damage;
- rare pulse, shortness of breath, edema, previous arrhythmias with clinical manifestations;
- simultaneous use of drugs that prolong the QT interval (this is indicated in the instructions for use of such a drug);
- low potassium content in the blood (prolonged vomiting, diarrhea, taking large doses of diuretics);
- severe liver disease;
- lactose or glucose-galactose intolerance;
- pregnancy, breastfeeding period, children under 18 years of age;
- individual intolerance.
Dosage regimen
Adults and children (the child’s body weight must be at least 40 kg);
- Treatment option No. 1 250 mg 1 tablet 3 times a day;
- Treatment option No. 2 500 mg 1 tablet 3 times a day;
- Treatment option No. 3 875 mg 1 tablet 2 times a day.
Children over 3 months old , weighing less than 40 kg
This category of patients should take the drug in the form of a suspension. It is available in two forms: 125 mg and 200 mg. It must be diluted in a special container included in the preparation with warm water and taken at the risk of a measuring cap:
- 125/31.25 mg – every eight hours, 3 times a day;
- 200/28.5 mg – every twelve hours, 2 times a day.
IMPORTANT! Before taking antibiotics, it is recommended to consult with your pediatrician.
Children under 3 months are prescribed a 125 mg suspension, taken 2 times a day, dissolved in the same way.
In case of phenylketonuria, taking suspensions is prohibited; accordingly, you need to choose a different antibiotic.
After opening, store the suspension in the refrigerator for no more than a week.
For people with kidney disease, the calculation is made depending on the creatinine clearance; the calculation is carried out by the doctor based on analyzes - the rate of filtration of a certain volume by the glomeruli.
- Above 30 ml – the dosage is the same as above;
- From 10 to 30 ml - take 1 tablet 250/125 or 500/125 twice a day;
- If less than 10 ml - 250/125 or 500/125 once a day.
What antibiotics to take for pneumonia
More often, doctors prescribe antibiotics for pneumonia in adults from the following effective drug groups:
- Penicillins: Carbenicillin, Augmentin, Amoxiclav, Ampicillin, Piperacillin.
- Cephalosporins: Ceftriaxone, Cephalexin, Cefuroxime.
- Macrolides: Clarithromycin, Erythromycin, Azithromycin.
- Aminoglycosides: Streptomycin, Gentamicin, Tobramycin.
- Fluoroquinolones: Ciprofloxacin, Ofloxacin.
Each of these groups differs from the others in the breadth of its range of applications, duration and strength of exposure, and side effects. To compare drugs, see the table:
| Group | Name of drugs | Features of application |
| Cephalosporins | Cefotaxime, Ceftriaxone | They treat uncomplicated pneumonia caused by strepto- and pneumococci, enterobacteria, but are powerless against Klebsiella and Escherichia coli. The appointment of this group occurs with proven sensitivity of microbes to the drug, with contraindications to macrolides. |
| Macrolides | Erythromycin, Azithromycin, Clarithromycin, Midecamycin | First-line drugs in the presence of contraindications to the penicillin group. They successfully treat atypical pneumonia and pneumonia associated with acute respiratory infections. Medicines affect mycoplasmas, chlamydia, legionella, hemophilus influenzae, but practically do not kill staphylococci and streptococci. |
| Semi-synthetic penicillins | Oxacillin, Amoxiclav, Ampicillin, Flemoklav | Prescribed for proven sensitivity to microorganisms - Haemophilus influenzae, pneumococci. The drugs are used to treat mild pneumonia caused by viruses and bacteria. |
| Carbapenems | Meropenem, Imipenem | They act on bacteria resistant to cephalosporins, eliminate complex forms of diseases and sepsis. |
| Fluoroquinolones (quinolones, fluoroquinols) | Levofloxacin, Moxifloxacin, Sparfloxacin | Affects pneumococci. |
| Monobactams | Aztreons | The drugs are similar in action to penicillins and cephalosporins and have an excellent effect on gram-negative microorganisms. |
When prescribing antibiotics for the treatment of pneumonia in adults, doctors should pay attention to the compatibility of the drugs. For example, you cannot take medications of the same group at the same time or combine Neomycin with Monomycin and Streptomycin
At the initial stage, before obtaining the results of a bacteriological study, broad-spectrum drugs are used; they are taken as continuous therapy for three days. Then the pulmonologist may decide to change the medication.
In severe cases, a combination of Levofloxacin and Tavanic, Ceftriaxone and Fortum, Sumamed and Fortum is recommended for adults. If patients are under 60 years of age and have mild pneumonia, then they take Tavanic or Avelox for five days, Doxycycline for up to two weeks, Amoxiclav, Augmentin for 14 days. Antibacterial agents should not be prescribed independently, especially for older people.
Why does the drug not help with sore throat?
Ceftriaxone does not help with angina if the microbes that cause the disease are not sensitive to it: viruses, fungi, mycoplasmas, chlamydia. There is also a form of the disease (Simanovsky-Plaut-Vincent), when the source of infection is one’s own bacteria, which normally live in the oral cavity. Due to low immunity, exhaustion, and lack of vitamins, they turn into pathogens.
In all these cases, it is necessary to conduct a mucus analysis (scraping from the tonsils) with culture and determination of sensitivity to medications, as well as a blood test. Based on the diagnostic results, the treatment regimen is changed.
The second group of reasons is associated with errors in the treatment itself:
- different intervals between injections;
- skipping an injection;
- early cessation of drug administration;
- incorrectly calculated dose (usually during self-medication);
- long-term storage of the prepared solution before injection;
- using an expired drug;
- The patient had previously been treated incorrectly with this antibiotic.
Throat swab
All this leads to the development of microbial resistance to Ceftriaxone, even if they were sensitive to it before treatment. Such patients are prescribed a different antibiotic. The low effectiveness of any antibacterial therapy can also be explained by the presence of associated factors:
- low immunity;
- previous chemotherapy or radiation treatment;
- exhaustion;
- hypovitaminosis;
- smoking;
- lack of bed rest;
- allergy to antibiotic.
In all cases, complex treatment will be required, possibly in a hospital setting.
We recommend reading about the rules for using Ceftriaxone for pneumonia. From the article you will learn about how Ceftriaxone works for pneumonia, the regimen and course of treatment, contraindications and side effects.
And here is more information about Ceftriaxone analogues.
Ceftriaxone helps with angina, but only if the pathogen is sensitive to it. Improper use of the drug contributes to the acquisition of bacterial resistance to the antibiotic and a decrease in the effectiveness of treatment.
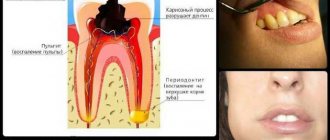
Features of the disease
This disease can occur without pronounced clinical symptoms.
In patients it can be suspected based on the following signs:
- one feels lethargy, weakness, and general malaise;
- often suffer from headaches;
- there is a complete or partial loss of appetite;
- shortness of breath is observed (if it rapidly increases, then the patient’s lungs become stagnant, or intoxication develops);
- a cough appears, which may initially be unobtrusive, but painful (the accumulated sputum cannot be released and because of this, the likelihood of obstruction in the respiratory tract increases).
What is pneumonia
Pneumonia is inflammation of the lungs. It occurs due to infection in the body and is very difficult . Its symptoms are:
- Dyspnea.
- General weakness.
- Intoxication of the body, accompanied by vomiting.
- High body temperature (above 38 degrees), which lasts for several days.
- Cough with phlegm or blood.
- Headache.
To make a correct diagnosis, it is necessary to donate blood, sputum for laboratory tests, and take a chest x-ray. If the diagnosis is correct, the doctor prescribes antibiotic treatment. For pneumonia, this is the surest treatment. Antibiotics for pneumonia help eliminate the source of inflammation .
The use of antimicrobial drugs is necessary to prevent the development of pathogens, bacteria, rods, viruses and to minimize the risk of complications. If you do not start treatment in a timely manner, you may miss time. Because of this, subsequent treatment can take a very long time, and in some cases, delay can be fatal.
Symptoms
The manifestations of pneumonia are quite varied. Nowadays, the asymptomatic course of the disease is very common, when the temperature does not rise, there is no cough, there is no sputum. Therefore, such pneumonia begins to be treated late, and this is fraught with the development of serious complications.
Main symptoms of pneumonia:
- Temperature rises to thirty-seven to thirty-nine and a half degrees.
- Dyspnea.
- Runny nose.
- Constant cough with sputum production.
- Chills.
- Colds that last more than a week, especially when improvement is followed by a sharp deterioration in condition.
- There is no decrease in temperature after taking Paracetamol.
Pneumonia is characterized by chest pain when taking a deep breath. Usually it appears in the place where the main focus of inflammation is located.
It is worth noting that coughing is not a characteristic sign of pneumonia, since the infection may be located away from the main respiratory tract. Sometimes skin color may change, headache, or fever may appear.