Pain after dental implantation, tooth implant hurts
During dental implantation, the trigeminal nerve and its branches, the alveolar nerve plexus, may be damaged as a result of:
- Screwing the implant into the canal where the trigeminal nerve or its branches lies;
- Inflammation in the implant area (infection and/or implant rejection).
Some pain during the implant healing process is normal. If the pain after dental implantation lasts too long, is very severe, or is accompanied by numbness of the lip or cheek, we can check the condition of the trigeminal nerve using electromyography and a neurological examination based on the characteristic loss of facial sensitivity and the spread of pain along the trigeminal nerve system.
The rejection reaction and inflammatory processes in the implant area are usually clearly visible with CORRECT X-ray examination and computed tomography.
Implants in the lower and upper jaw. Pain after dental implantation
There may be direct pressure from the implant on the nerve or inflammation in the implant area with tissue swelling, edema and subsequent pressure on the nerve.
The jaw hurts and clicks after prosthetics or dental treatment
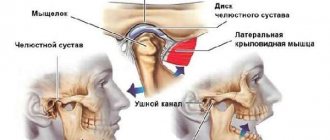
Dysfunction of the temporomandibular joint. The lower jaw is connected to the skull by two temporomandibular joints. Impairment of the function of these joints is possible after the installation of a denture, crown, bridge, any treatment or tooth extraction if this leads to malocclusion and/or damage to the temporomandibular joint. This is a typical complication after dental prosthetics. Read more about treating TMJ dysfunction here
Temporomandibular joint dysfunction
The green arrow indicates a healthy joint. The red arrow points to the joint that remains in the “open” position when the mouth is closed. This leads to wear and tear of the articular cartilage, pain and clicking when opening and closing the mouth. One of the reasons is the incorrect position of the upper right “eight” (tooth 1_8 lies horizontally).
How can we help you:
- Anti-inflammatory treatment will help relieve pain. If necessary, we inject anti-inflammatory medication directly into the lower jaw joint . This brings relief within a few minutes .
- Injection of botulinum toxin preparations (for example, Botox or Dysport) into spasmodic muscles. This is relevant in the case of an excessive increase in the tone of the masticatory muscles, if it is the muscles that are the “culprit” of dysfunction of the temporomandibular joint.
- Treatment by an osteopath. An osteopath works with the joints and muscles of the jaw using gentle manual techniques. This way you can solve a lot of problems that cannot be solved in classical dentistry. More about osteopathy
- Introduction of chondroprotectors (medicines for nutrition and restoration of cartilage) into the temporomandibular joint. Read more about cartilage restoration
Joint pathologies
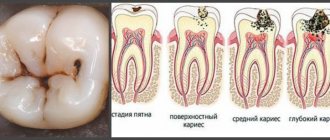
Inflammatory processes in the oral cavity, wisdom teeth caries, and pulpitis can make it painful to open your mouth. Not every dental pathology manifests itself with such symptoms.
Today, there are many different techniques to cope with caries, pulpitis and stomatitis.
The pain is due to the fact that the inflammatory process involves soft tissues located near the temporomandibular joint on the left or right.
For example, with inflammation of the hood of a wisdom tooth or pulpitis in the molars (back teeth, designated numbers 6 and 7 in dental practice).
The main localization of pain is the affected tooth or mucous membrane; when opening the mouth, talking and eating, the discomfort spreads to the lower jaw joint. Bad breath often occurs.
Treatment methods
Sick teeth should be treated in a dental office. Today, there are many different techniques to cope with caries, pulpitis and stomatitis. Most often, they resort to removing the affected part of the tooth and placing a filling.
Neurogenic pain, i.e. sensations caused by pathologies of the facial or trigeminal nerve often occur after hypothermia, head and face injuries. They are always accompanied by a number of additional symptoms, which makes it possible to determine nerve damage.
Pathologies of the joint not associated with injury - arthritis, dysfunction and others - cause disruption of the basic mechanisms of its operation, so the process of opening and closing the mouth becomes painful.
Sinusitis, maxillary sinus cyst, loss of sense of smell after visiting the dentist
The roots of the teeth of the upper jaw can normally be adjacent to the maxillary (maxillary) sinuses of the nose and even survive in them . Sinusitis, maxillary sinus cyst and loss of smell are possible when infection or filling material penetrates from the teeth into the paranasal sinuses. Unfortunately, this is not uncommon. Moreover, some cases of persistently recurrent sinusitis are associated with infection penetrating from the roots of the teeth . In this case, a possible symptom is a strong unpleasant odor from the nose and mouth.
Odontogenic sinusitis after treatment by a dentist
Odontogenic sinusitis (scheme). Teeth and maxillary sinus. On the left is the norm. On the right – the root of the “seven” (tooth 2_7) is destroyed, inflammation around the destroyed root, pus in the maxillary sinus.
Filling material in the maxillary sinus and sinusitis after filling the “six” canals (tooth 2_6). Pain in the left side of the face after visiting the dentist.
1 – roots of teeth, 2 – normal, air in the right maxillary sinus (front view, the air looks black in the picture), 3 – in the left maxillary sinus there is a fragment of filling material surrounded by an inflammatory shaft. The patient had been mistakenly receiving treatment for trigeminal neuralgia for a long time.
Cysts of the maxillary (maxillary) sinuses in diseases of the roots of the teeth.
1 – roots of the teeth, 2 – cysts of the maxillary sinuses, growing from the roots of the teeth (cysts are round “bubbles”, they look gray in the picture).
How can we help you:
- Let's find the source of pain after dental treatment;
- We will treat inflammatory processes, sinusitis, sinusitis and neurological complications; if necessary, your health will be taken care of jointly by a neurologist and an ENT doctor. Treatment of sinusitis without puncture
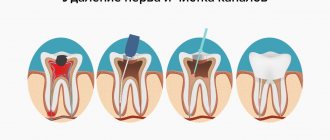
The most common types of pain relief in dentistry
Most often, in order to cure caries, pulpitis, periodontitis, remove a tooth or perform other dental procedures (for example, dental implantation), the doctor administers local anesthesia, namely a pain-relieving injection into the gum. If it is painful for the patient to inject into the gums, and he experiences discomfort during the injection process, the specialist pre-treats the gums with an aerosol or spray (application anesthesia), which reduces the sensitivity of the soft tissues.
Dentists mainly use types of conduction and infiltration anesthesia. With the help of local anesthetics, it is possible to achieve a minimal toxic effect on the patient’s body, because medications administered topically affect only the area of preparation.
The doctor applies infiltration anesthesia to the problem area (for example, near the root of a diseased tooth). After its introduction, neighboring areas retain their sensitivity. The guidewire is effective for carrying out larger-scale interventions, because it affects directly the branch of the nerve that is responsible for a certain area. After the administration of a conductive anesthetic, all periodontal tissues are literally “frozen.”
How long does an injection into the gum last? Infiltration – up to 2-3 hours, conductive – up to 8-10 hours.
Read the article on the topic: anesthesia in dentistry. Find out what modern methods of anesthesia allow you to avoid an injection into the gum.
Pain in the gums after visiting the dentist: normal or pathological
It is quite normal for the gums to hurt after the injection and after the anesthesia wears off, provided that the discomfort is not severe and is limited to a few days. After all, in order to administer the medicine, the doctor is forced to pierce the soft tissues using a special thin needle located on the syringe. This manipulation, although minimal, injures the mucous membrane. Therefore, pain for several hours or several days after the end of anesthesia can be considered normal.
On a note! Today, private dentistry is increasingly using carpule syringes, which have very thin needles and virtually eliminate injury to soft tissues.
If your gums continue to hurt for a long time after an anesthesia injection, and the discomfort intensifies or becomes unbearable, then you need to consult a dentist.
Nausea after anesthesia
Nausea is the most common side effect
The most common side effect after anesthesia. Occurs in every third case. Of course, with local (regional) anesthesia this complication is much less common.
There are some general principles to help reduce the likelihood of nausea after anesthesia:
- Don’t rush to get up after surgery, much less run somewhere. Your body does not know that you are an important busy person, it only understands that it was first stunned with chemicals, and now for some reason they are shaking it. As a result, you may vomit at the most inopportune moment;
- Do not drink or eat for 3 hours after surgery;
- If you are worried about severe pain (the anesthetic was titrated incorrectly, for example), then you should not endure it - tell the nurse or doctor, because may vomit from pain;
- If nausea occurs, try to breathe deeply and slowly. Saturating tissues with oxygen reduces the risk of nausea.
Causes of pain in the gums
An injection of anesthesia into the gums is a prerequisite for your peace of mind in the dentist's chair when treating diseases of the oral cavity. However, you must be prepared for the fact that in some cases, after treatment, pain may appear, which will indicate various pathologies. Let's look at each reason in detail.
Development of an infectious process in the soft tissues of the oral cavity
This can happen if the patient has a poor oral hygiene index, and there is a large number of sick, decayed teeth in the mouth that need to be removed. When the doctor injects an injection into the gum, a wound then forms on the soft tissues, which needs time to heal. If, during the healing period, pathogenic bacteria penetrate the wound, an inflammatory process begins, which can, if not consulted in a timely manner, be complicated by the occurrence of an abscess or purulent cyst. Inflammation can also penetrate deep into the soft tissues, spread to neighboring organs, and cause swelling of the face.
The infectious process can develop against the background of a weakened immune system in the patient, as well as due to a violation of the aseptic processing of instruments and the workplace in the dentist’s office.
Damage to nerve endings
An inexperienced doctor could touch and injure a nerve when administering an anesthetic. In this case, at first you may be bothered by numbness, and then pain will appear, which will be aching at first, and then unbearable - it may not go away for up to several months in a row, it will be difficult to relieve it with painkillers and syrups. Also, pain can radiate to other parts of the maxillofacial apparatus (eyelids, cheeks, temples, ears). Damage to the facial nerve may be indicated by difficulty opening the mouth and chewing food.
The possibility of touching a nerve most often occurs during the administration of conduction anesthesia.
Hematoma formation
The soft tissues and mucous membrane of the oral cavity are penetrated by blood vessels and capillaries; if the doctor inserts the needle carelessly or too quickly, the doctor could touch one of these vessels or capillaries. This in turn provokes their damage and the formation of a blood clot. Because blood cannot flow out, a hematoma forms under the mucosa, which puts pressure on the surrounding soft tissue, which causes pain.
Allergic reaction
Some patients have an individual reaction not only to the components that make up anesthetic drugs, but also to filling materials, to medications that the doctor uses in the process of work. This may cause irritation to the oral mucosa.
According to some studies, 1 allergies and side effects occur more often in patients with anesthetics that include novocaine, dicaine and anesthesin. But the likelihood of allergies when using drugs containing lidocaine, mepivacaine and articaine is much less.
Soft tissue necrosis
Necrosis is the death of living cells and tissues, provoked by a number of circumstances. This complication is quite rare. It may occur due to the fact that the doctor gave the injection traumatically, injected the anesthetic too quickly, due to which the blood vessels were compressed. The reason could be an incorrect calculation of the drug, leading to vasospasm - most often this reaction is caused by adrenaline. In a very rare case, the doctor mistakenly administered not an anesthetic, but, for example, calcium chloride or alcohol.
Sometimes the reason lies not in the lack of experience of the doctor, but in the state of health of the patient himself. A similar problem may arise in people with diabetes, because... their blood circulation is impaired. An infection could also be the cause.
How to treat swelling of the cheek?
Minor swelling that occurs immediately after the injection due to the introduction of a large volume of anesthetic will disappear on its own within 24 hours; you do not need to do anything special for this. Pain after subperiosteal administration of the drug usually subsides by 2-3 days and is completely eliminated by 4-5. To alleviate the condition, you can use simple analgesics or non-steroidal anti-inflammatory drugs in minimal effective dosages.
To relieve unpleasant symptoms, the dentist may prescribe NSAIDs.
If the initially swollen cheek continues to swell after visiting the dentist, the pain subsides, and the overall condition does not worsen, you should continue the treatment prescribed by the doctor for 2-3 days. If after this there is no clear improvement, you need to consult your doctor again to adjust the prescription.
At the slightest suspicion of acute inflammation (swelling, severe pain, local increase in temperature), you should contact a dental surgeon. If you detect it at the initial stage of diffuse edema, when there is still no cavity with pus, then there is a chance of avoiding surgery and getting by with taking antibiotics. If an abscess has already formed, the surgeon will make a small incision from the inside on the mucous membrane to release the pus and prescribe medication.
Self-medication for purulent complications is dangerous. With a successful combination of circumstances, the abscess will break through the mucous membrane into the oral cavity and recovery will occur. Much more often, the cavity with pus opens into the adjacent anatomical area, which leads to the spread of the process.
A girl applies an ice pack to a hematoma
A hematoma of the buccal area usually becomes noticeable after the end of the appointment, so the doctor has the opportunity to identify the complication and explain to the patient what to do in this situation. Within 5-6 hours after the appearance of the hematoma, cold is prescribed to the area of swelling, followed by ointments with absorbable and venotonic effects (Lioton-1000, Traumeel-S, bruise-off). Depending on the clinical situation, the doctor may recommend taking an antibiotic to prevent suppuration of the hematoma; you should not refuse this. There is no need to massage, warm, or even try to release the hematoma. This will lead to suppuration or new bleeding into the tissue.
(Ratings: 7 , average: 4.71 )
Symptoms that should alert you
Have you had an injection in your gums before having your teeth treated, and after treatment the discomfort increases day by day? Then you need to know that pain is not the only symptom that should alert you. Pay attention to a number of other alarming symptoms that may indicate pathology and require prompt consultation with a doctor:
- increase in local and general body temperature,
- burning and itching on the mucous membrane,
- the appearance of ulcers on the mucous membrane,
- swelling and hyperemia of the mucous membrane,
- facial asymmetry,
- the appearance of a cyst or flux,
- general weakness and loss of appetite,
- the appearance of bad breath,
- difficulty opening the mouth and chewing food,
- irradiation of pain to other parts of the maxillofacial apparatus.
“There was such a situation: the doctor touched a nerve. But only I didn’t have any pain in my gums, but on the contrary, everything became numb, so that I couldn’t feel the taste of food or anything at all, and my face was also distorted. I went to the doctor only a week after this, I was prescribed physiotherapy and pills to take. I finally got rid of the problem only after 5 weeks! And he only treated caries. So much for 21st century medicine!”
Alexander K, review from otzovik.com
Why does toothache radiate to the jaw after removal or treatment?
The causes of pain can be very diverse.
Soft tissues contain nerve endings. During the procedure, they stop signaling due to the effects of anesthesia. When its effect stops, the jaw begins to ache. Normally - up to four days.
After complex removal, pain continues for 7-10 days. If it hurts longer and the sensations intensify, it means something went wrong. There are several reasons for complications:
- Medical error. If you cut it out incorrectly with a drill, sharp bone edges remain sticking out, and the oral mucosa will be constantly irritated.
- Parts of the bone have not been removed from the socket, or a blood clot does not appear. Inflammation of the hole is possible.
- The doctor did not stitch up or prescribe an antibiotic.
Reference! It happens that in addition to a problematic tooth that requires removal, the patient also experiences purulent inflammation of the gums. In this case, the gum is cut and the pus is removed. After such a procedure, which was also accompanied by tooth extraction, the jaw will hurt severely and for a long time.
Pain in the lower jaw varies in nature and is not always associated with dental treatment. If the jaw on the lower left side hurts for a long time, a possible cause is the presence of arthritis, arthrosis or neuralgia.
A classic example of mild lymphadenitis is inflammation of the lymph nodes against the background of a dental problem. In this case, the treatment takes place in two stages: first, the tooth is treated, then the inflammation of the lymph node is relieved with the help of medications.
There are several reasons for this:
- dirty hands;
- periodontitis;
- injuries to the facial part of the head;
- the presence of inflammatory processes;
- after intervention for tooth extraction.
If the periosteum becomes ill, then the gums become swollen, swelling spreads to the entire face, pain radiates to the temple and neck - these are symptoms of gumboil, and immediate medical attention is required. A thorough inspection will be carried out there and the necessary measures will be taken.
If your jaw hurts when you press on a tooth underneath it, this is a sign of periodontitis. This diagnosis may also be accompanied by swelling of the face, swelling of the gums, gumboil, enlarged lymph nodes and body temperature. Causes of the disease: injury or allergy, poor quality oral treatment.
Attention! If periodontitis is suspected, seek qualified help immediately. The dentist will diagnose and prescribe therapy.
How to relieve pain: what you can do and what you can’t do
What can and should be done
If, after visiting the dentist and receiving an injection in the gums, pain appears that causes concern, then the following measures can be taken:
- sign up for an appointment with the doctor,
- alleviate your condition with painkillers and antipyretics (if your body temperature has increased), antihistamines (in case of allergies). For example, “Nise”, “Ketanov”, “Nurofen”, “Erius”. You can use any drugs that suit your indications and usually save you in such circumstances,
- carry out antiseptic treatment of the oral cavity using Miramistin, Chlorhexidine, soda-salt solution, decoction of pharmaceutical herbs (for example, chamomile and sage),
- rinse your mouth after every meal so that bacteria do not have the opportunity to cause an inflammatory process.
Read an article on the topic: what to do if your gums are swollen and painful.
What not to do
- do not eat “irritating” foods: ban hot and cold, salty and spicy, carbonated drinks and alcohol, solid foods,
- do not prescribe antibiotics on your own,
- you cannot stop performing oral hygiene with a toothbrush: if the injection site in the gum hurts very much, then try not to put pressure on this area and not injure it again, but you need to brush your teeth to remove plaque and bacteria from the oral cavity,
- stop smoking: exposure to nicotine and tar will impair blood circulation in the mucous membrane and also slow down the natural processes of regeneration of damaged tissues,
- Do not heat a swollen gum or cheek, because if there is inflammation, the infection will quickly spread to nearby areas, which will very quickly worsen your condition and be fraught with blood poisoning,
- Do not treat the wound with alcohol-containing preparations and garlic, because this can burn the delicate mucous membrane and aggravate the situation,
- do not touch the gums with your hands or foreign objects,
- Do not apply crushed tablets such as Aspirin or Analgin to the inflamed area.
Why does the gum above the denture hurt?
Prosthetics is the most popular service in dentistry.
Designs of various types are installed in the mouth of every second person over 40 years of age. Crowns and bridges are designed to restore the ability to chew and pronounce sounds clearly. With their help, the orthodontist removes serious bite defects and the consequences of traumatic tooth loss, and reduces the distance in the dentition. Modern materials are comfortable for everyday wear, so normally the client should not feel pressure or pain. Sign up for a free consultation:
The mucous membranes around the teeth are penetrated by a large number of nerve endings. They not only hold them in one position, but also distribute pressure during chewing and supply the enamel with nutrients and minerals. Therefore, inflammation is quickly transmitted to the roots and pulp, affecting neighboring molars. If the gums under the denture are very sore, the reason lies in the following disorders:
- Food debris constantly gets stuck between the crown and the mucosa, decomposes or turns into tartar.
- The manufactured structure is too rigid, poorly adjusted during fitting, or made with defects.
- The dentist incorrectly calculated the pressure points, which increase when chewing or clenching the jaws.
- When it comes into contact with the epithelium, the metal in the prosthesis oxidizes, giving an allergic reaction and causing irritation.
- Lack of the optimal amount of vitamins and microelements beneficial for the mucous membrane in the daily menu.
If the gums above the denture hurt badly, in 90% of cases the culprit is the accumulation of food plaque. The crowns on the upper jaw are the hardest to clean even with the most convenient brush. Food particles become the basis for the active proliferation of bacteria and fungus. This threatens a person with exacerbation of diseases of the mucous membranes and periodontium, provokes a putrid odor and spoils the structure.
Measures to help prevent complications from developing
First of all, it is important to find a professional doctor who will carry out all medical procedures carefully and efficiently. After all, with an experienced specialist, you don’t have to worry about whether it’s possible to give anesthesia injections into your gums, and the pain after treatment either won’t arise at all or won’t bother you for more than a few days. However, finding a good dentist is only half the battle. To avoid complications, try to follow simple rules.
Rule #1: Avoid eating food immediately after treatment procedures. It is recommended to have a snack only after 2-3 hours, otherwise you yourself may injure the mucous membrane or introduce bacteria and pieces of food into the wound that has not yet healed.
Rule No. 2: on the first day after treatment, refrain from eating spicy and hot foods, sunbathing and visiting steam rooms and saunas, because this can cause a rush of blood and swelling of the soft tissues.
Rule No. 3: For the first few days, perform oral hygiene very carefully and carefully to allow the soft tissues to heal.
1 Karpuk I.Yu. Allergic reaction to local anesthetics: diagnosis and prevention. Bulletin of Vitebsk State Medical University, 2009.
Why might there be pain after an anesthesia injection at the dentist?
Treatment and removal of teeth is an unpleasant and very painful procedure. To prevent a person from feeling pain during dental procedures, anesthesia is used. Today, tooth extraction, oral surgery and even simple treatment cannot be done without pain relief.
Anesthesia is an integral part of dental treatment; after a certain period of time, the unpleasant sensations disappear, the injection site stops hurting, and the patient continues to go about his business, forgetting about the problem. But for some people these feelings do not go away - their gums still hurt after the anesthesia injection.
In this case, a second visit to the doctor is inevitable.
Features of anesthesia
Anesthesia during dental treatment and other surgical interventions allows the patient not to feel pain, while the dentist can calmly carry out the manipulations associated with the treatment.
Today, special syringes with very thin needles are used for injections, which cause the least harm to soft tissues. The dentist irrigates the injection site with an aerosol anesthetic, so the injection is painless. But sometimes it happens that the jaw begins to hurt after anesthesia.
This effect can occur if the dentist gave the injection incorrectly.
For pain relief, dentists use conduction or infiltration methods, which affect a specific painful area, so anesthesia does not have a toxic effect on the entire body.
Conduction anesthesia is used for deeper medical operations; it affects the entire nerve, which is responsible for the immediate area of excitation. The gum is pierced directly into the area of branches of the branches of the trigeminal nerve.
Conductive anesthesia is practiced during the removal or treatment of molars, removal of the nerve trunk, and operations on the gums.
Infiltration anesthesia is done directly into the mucous membrane of the gums. The injection time is limited to one hour, so this anesthetic is used when cleaning dental canals.
Application anesthesia is used in the form of a gel or spray, which is applied to a small area in the form of applications.
Its duration of action is limited, so this anesthesia is used during simple dental operations or as an auxiliary anesthesia of the gums before piercing it with a needle.
Teeth hurt after dentures
Consultation:
Consultation:
Good afternoon. First of all, I want to say that you really need a good dentist. Because with neuralgic pain there is no temperature! Now let's figure it out. From your photo, the quality is very poor. Either this is a printout on paper of an image on a visiograph, or the terrible quality of the x-ray. If the first, then I need the original, recorded from the clinic’s computer. Because the printout produces such poor image sharpness. that there is nothing visible there. Secondly, it is necessary to take intraoral (small) photographs of the teeth that are bothering you. This is really necessary, since the images will give a complete picture of what is happening in the bone, especially in dynamics. If there are none, get it done at any clinic. It’s better to upload X-ray photos to us, as all patients do (if they don’t give you the pictures on disk), without reducing the size of the photo. Just like it is from the camera, it’s easier for me to process it later. After we get a good image, I will write to you what the problem is: what someone said about the cyst, if that is the case. then it can give all the symptoms that you described. And it needs to be treated as soon as possible, if it exists. Be sure to indicate which teeth hurt (as you think) so that I can navigate. Thank you very much for your help and advice. I'll try to post pictures as soon as possible. Here is a picture of the teeth that are bothering me. Unfortunately, our hospital does not have a computer and there is no way to post a picture with good quality. Please advise me on these pictures.
Well, I think I'm starting to understand what's going on here. I didn’t see anything criminal in the photo. Question about the photo - when did you take this photo? A couple of days ago or when the prosthetics were installed. If this is an old photo. then it is not informative, you will have to take a new fresh photo. Now it shows that the canals are sealed, there are inlays, everything is done seriously. BUT I don’t understand why you worked on the front teeth, but didn’t do anything with the bite as a whole .
You already have extracted chewing teeth; the image shows the tilt of the remaining teeth towards the defect. This indicates that there is a decent decrease in the bite. And this, in turn, leads to the fact that your entire bite begins to rest only on your front teeth. Hence the overload and pain. Of course, this is just an assumption for now, but the picture confirms that the reason is not in the teeth specifically, but in incorrect prosthetics in general. If you were my patient, I would not do the front teeth, no matter how much you insisted on it. First, you need to correctly restore your bite, raising it to your physiological height (this is done by prosthetics of the chewing teeth), only then can you proceed to the front teeth. I'm waiting for clarification on the photo (it's old). If it's old, you'll have to make a new one. If it’s new, then most likely it’s a matter of overloading the teeth due to a lack of prosthetics for the chewing teeth. The last picture was taken today. Since my teeth have been hurting for three months now, I am being offered resection of my upper teeth as an option to relieve the pain. Dentists say that the canal has been filled, but it shouldn’t cause such pain. Advise me what to do. No, of course there is a refilling, but it really cannot cause such pain. Resection - it’s difficult to say whether it will have a positive effect, since the roots are not long; if you cut off another part of the root (resection means exactly this), they will become even shorter. But this is not very good for prosthetics. What about your prosthetics? Why didn't you start studying chewing teeth? And one more thing - when closing the teeth, look to see if there is contact between these front teeth and the lower ones, or is there a gap there? And describe the pain: - when does it appear - morning, evening, after eating, or always, but not severe? - Do you fall asleep with pain or does it not bother you at night? — what causes it? (taking what specific medications and how long do they last? - what makes it worse (eating, just like that), or is it permanent and doesn’t change throughout the day? Thank you very much for your support and answers to your questions. Perhaps what needs to be said in more detail how it all began. In June of this year, they began to prepare my teeth for prosthetics. They treated tooth 11 using depophoresis and the canal was refilled. Tooth 21, the canal was refilled and temporary crowns were made from plastic. There was pain when inserting the pin insert and I was prescribed indomethicin for three days 0.025 2-3 times a day and ciprolet 0.5 2 times a day for 7 days. A few days later I had a hypertensive crisis, which was accompanied by tremors. Before that, nothing like this had happened to me. The upper crowns were made very thick, which interfered with my bite. I told the doctor about this, but he, having sharpened it a little, began to get nervous: “Well, what else is bothering you?” I decided to be patient, but the pain remained and the teeth were impossible to finish. After that, my lower teeth began to hurt, because my upper teeth were constantly banging against them. I told the doctor about this, but he replied that it was due to a hypertensive crisis. Next, 2 adjacent lower teeth became ill, then 2 adjacent upper teeth, and gradually the entire jaw. I underwent treatment by a periodontist and physical procedures (Milta and laser), received injections, but nothing helped, the pain only grew, became stronger and stronger, especially in the jaw. After 1.5 months, the temporary crowns were removed from the bite. When I saw the surgeon, he said that there is no arthritis here, but your jaw hurts from your teeth. Take painkillers and sedatives, but it was impossible to endure it, as there was a feeling that you could go crazy from the pain. The pressure began to rise, the rhythm of the heart began to be disturbed, and recently my heart ached so much from pain that it seemed that I could die from painful shock. I had a fever and very severe chills for 10 days. I could not sleep at night. Doctors said that this is a general condition and that you need to see a therapist. I was examined by a therapist, but he did not find any abnormalities. Because of the severe pain that drove me crazy, I had to turn to a psychiatrist, who prescribed me Atarax and Finlepsin. With these drugs I could at least fall asleep and sleep until the morning. But for the last two nights I could not sleep because I was shivering and it seemed that the severe pain in my jaw would stop my heart, I had a constant fever and was very weak. Then I insisted on taking tests, in which there were 13.9 leukocytes, 11 neutrophils, and 1 young rods. At my insistence, I was admitted to the hospital, but for some reason only in the neurological department, because... They decided that I was fixated on toothache. But after 2 days, neurologists transferred me to the dental department, and the dentists, having found nothing in my mouth, discharged me from the hospital also after 2 days. At the same time, antibiotics were injected for 4 days, and Mexidol was given as a drip for only 2 days. On the second day in the hospital it became a little better, my jaw began to hurt less and the pain in my teeth decreased, but I was discharged on September 20 and was told that it was neurological. At first the condition was very serious, I had some kind of crisis, again with chills and increased blood pressure. I tried to prove to the clinic that this is some kind of inflammation, but they don’t see osteomyleitis in the picture, and there can be no other infections or inflammations. After being discharged, after some time, my condition was almost satisfactory, but the pain in my teeth did not go away, my chin began to hurt a little and my jaw began to hurt again. I’m afraid to think that it could be an infection, since after the first and second course of antibiotics I felt better. Answering your questions, I can say that I have constant aching pain in my teeth from morning to evening, it’s unpleasant to clench my jaws. I fall asleep with pills, tired after work. Sometimes I wake up at night just like that, sometimes it’s painfully hitting tooth on tooth. Now I take sedative pills prescribed by a psychiatrist. Before that, I took Nise and Ketorol, which relieved the pain a little after 1-1.5 hours. Please advise what I should do, because now I’m tired of my requests, they probably offered me resection, but will this make the pain, especially in the jaw, go away? The more I delve into your situation, the more I understand that the problem is not inflammation, but the bite. Since you say that it was your front teeth (both upper and lower) that started to hurt first, despite the fact that your lower ones are completely normal, this only speaks of overload. Because when they put crowns on the front teeth, they did not take into account the fact that the bite was currently very low. And now there’s no point in looking for a neurologist either. Just take off these crowns and walk around without them, with temporary plastic ones (which can be safely cut down so that they are comfortable for you). And I'm sure everything will work out. And resection has nothing to do with it. You can’t have all your teeth, upper and lower, resected? It's all about the crowns. Not even in the crowns themselves, but in prosthetics in general. With these crowns, you will soon knock so hard on your teeth that you will lose your teeth (especially the upper ones, due to overload, they will soon break with a longitudinal fracture at the root) and further damage the joint. Remove the crowns and begin proper prosthetics. First the chewing teeth, and only then the front teeth. When the chewing teeth are already in a new position, in a new bite. This is my opinion. There is no point in convincing me of anything else. If you believe that this is neuralgic, go to neurologists. When you finally get tired of it and realize that the reason is different, you will remember my words. If the doctor who did the diagnosis doesn’t want to remove it, go to another one. I don’t believe that all doctors are the same and they all approach treatment like yours. Personally, I wouldn't get dentures on your front teeth until then. until you would make chewable ones. And it is impossible to persuade me in such situations, because I know that it will be like what you have now. In general, that's all I can tell you. The consultation was held on the Forum zub-zub.ru
The main causes of pain after an injection
After a puncture of the gums in the soft tissues, a violation of the integrity of the integument occurs, the patient feels a pain syndrome in the area of the injection, which will go away on its own after some time. After anesthesia, the gums may hurt from several hours to two days, it depends on the person’s condition.
This is a natural effect of the body on the injection, which does not require any treatment; after some time, the puncture site gradually stops hurting.
If the pain does not subside, but on the contrary, becomes more and more unbearable, you should contact a dentist who will determine its cause and prescribe appropriate treatment.
Reasons why the mucous membrane or gums continue to hurt:
- Development of infection;
- Trauma to the nerve trunk;
- Hematoma formation;
- Necrosis of soft tissue on the gum;
- Allergy to anesthetic;
- Increasing pain at the site of dental surgery.
We will consider each of these reasons separately in order to have an idea of the possible risks of visiting the dentist.
What to do to eliminate pain
Pain in the jaw as a result of tooth extraction is considered a common phenomenon.
This pain can be sharp and twitching, or, conversely, aching and dull. The time frame is also different, ranging from several hours to several days.
Whether this symptom is a variant of the norm or a problem requiring medical intervention, the doctor decides individually.
There are cases when it is impossible to save a tooth, for example, when there is severe inflammation of the soft tissues around the tooth, or when it is completely destroyed along with the root. Then there is only one option - deletion. But this operation has contraindications:
- post-infarction condition of the patient;
- exacerbation of chronic liver diseases;
- flu or pneumonia;
- acute pain in the kidneys and pancreas;
- stomatitis and other diseases of the oral mucosa.
Important! In modern medicine there are painless methods of removal. And then, for a favorable outcome, you must follow all the dentist’s recommendations.
Simple method
A simple method is to pull it out using dental forceps. First, the patient is given local anesthesia, then the soft tissue around it is moved away to access the tooth. Using forceps and hand pressure, the tooth is extracted using a twisting motion. After such an operation, the norm for pain is up to four days, with the pain subsiding.
The hard way
If removal with forceps alone is not possible, soft tissue is cut to provide access to the root of the diseased tooth. This option is considered difficult, and removal is done in parts. The doctor removes the tooth and places stitches on the cut tissue. After such an intervention, the pain is stronger and lasts longer. During the normal course of recovery, the pain lasts from several days to a week, but has the character of attenuation.
Photo 1. Scheme of a complex tooth extraction: the doctor administers anesthesia, after which he cuts the gum and, using a drill machine and forceps, removes the tooth in parts, then the gum is sutured.
There are several recommendations that can be followed to prevent pain:
- Try not to touch the hole with your tongue.
- Refrain from rinsing your mouth for three days.
- Do not consume cold or hot food or drinks.
- Avoid breathing through the mouth so that air does not get into the wound, especially outdoors in winter.
- Avoid sweets for several days, avoid smoking and drinking alcohol, and take a hot bath.
If you apply a cooling compress to the cheek on the side of the sore spot, the nerve endings will freeze and the pain will be localized for a while. A compress can be a piece of cloth soaked in cold water or any other cold object. The method brings relief only the first day after the intervention.
There are several remedies that help with toothache and accompanying pain. Taking drugs Ketanov or Ketorol, Nise, Nimesil or Nurofen will relieve pain and help you survive the postoperative period.
Rinse
You can rinse no earlier than the third day after removal, otherwise the blood clot may be washed out, and as a result, the inflammatory process may begin.
To rinse out areas of pain, dilute baking soda or salt in water. Use the rinse solution several times a day.
Quite often, patients experience pain in the jaw, which can radiate to the ear after dental treatment. There can be many reasons for the occurrence of unpleasant sensations. In many cases, this is a manifestation of the body’s normal reaction to dental intervention. However, sometimes pain still indicates the presence of complications.
In almost all cases, discomfort in the period after treatment is associated with injury to the soft tissues surrounding the tooth, as well as directly with its treatment. Carrying out complex anesthesia, applying a rubber dam during therapy, cleaning and filling root canals - all this creates microtrauma.
As a result, slight swelling and discomfort in the tooth and jaw may occur. Recovery in the oral cavity occurs very quickly, so normally the discomfort goes away on its own within a few days. During the recovery period, an important condition is maintaining high-quality oral hygiene, as well as following all the recommendations of the attending dentist.
If, two to three days after the dentist’s visit, the pain does not go away, spreads to the ear and throat, symptoms of inflammation increase, and the soft tissues in the oral cavity do not recover, this is not normal and you should immediately consult a doctor. Jaw pain is a difficult symptom in the body that requires immediate treatment.
- If the tooth extraction was difficult, then tissue restoration in the mouth takes much longer and requires more attention from both the doctor and the patient. Here, a possible complication is suppuration of the postoperative wound, a crack or fracture of the jaw, as well as incomplete removal of part of the tooth. Most often, difficulties during surgery arise when removing a wisdom tooth, which is due to its complex location in the bone. In the period after the removal of such teeth, swelling may spread to the throat and even the ear.
- Jaw pain after treatment may be due to unskilled root canals. The doctor could perform poor cleaning of the root canals, as a result of which inflammation increases, or fill them with material being removed beyond the root into the thickness of the bone.
- The state of the human immune system also plays a big role in recovery after dental surgery. With an insufficient level of immunity, all recovery processes in the body slow down, and the risk of secondary infection during the postoperative period and the development of inflammatory diseases of the ear, nose and throat increases.
Tooth extraction surgery is a serious injury to the oral cavity. During tooth extraction, the integrity of a large number of blood vessels is disrupted. In this regard, during the postoperative period, the occurrence of swelling of soft tissues both inside and outside the oral cavity is a common reaction of our body.
In addition to swelling, you may also experience weakness, pain in the jaw, and even an increase in body temperature. However, all of the above symptoms last no more than three to four days, and their intensity decreases every day. If symptoms do not subside within three days, you should immediately consult a dentist.
Doctors at the Vitasan dental clinic in Odessa always invite their clients for regular preventive examinations, as well as for professional oral hygiene services. A timely visit to the dentist allows you to identify diseases of the teeth and gums in the early stages and prevent the development of complications.
We never cease to remind our clients of the importance of professional hygiene services. The health of your teeth and gums depends on the quality of oral care. This procedure is a first-class prevention of all dental diseases and takes a minimum amount of time.
After the procedure, our specialists teach clients proper oral care at home, and also individually select hygiene products.
It happens that after treatment of caries, the tooth under the filling begins to ache. Discomfort can occur after the crown comes into contact with hot or cold, and can turn into intense, throbbing pain. Many people associate this condition with poor-quality medical services, but does an aching tooth after treatment always indicate the doctor’s unprofessionalism and is it possible to get rid of the discomfort without re-opening the filling?
What to do if pain occurs after the injection?
If the pain does not stop for several days, you should not self-medicate. Only a dentist knows how to eliminate the cause of the problem without serious consequences. For example, in one case you can do a cold compress, in another it is categorically not recommended.
Warming compresses are not recommended if purulent wounds appear at the site of the anesthetic injection that continue to hurt, this will lead to the spread of infection.
Quite often, after an injection of anesthesia, a headache begins, a general malaise appears, which is in no way associated with a visit to the dentist, and the result is an advanced problem that is more difficult to cope with.
If appropriate procedures are not prescribed after a gum nerve injury, significant complications can occur that are difficult to treat.
The doctor determines whether the patient needs to take antibiotics and, if the inflammatory process progresses and the gums continue to hurt, prescribes Amoxiclav, Sumamed or Lincomycin, which are not advisable to use without a specialist’s prescription.
If the patient is experiencing severe pain, the dentist will recommend painkillers such as Ketanov, Ibuprofen, Nise and Nurofen. If the patient is found to have suppuration, the dentist will open it, treat it with an antiseptic, and leave recommendations for further treatment.
Any drug, including anesthesia, has a toxic effect on the body, so self-medication can negatively affect the general condition, but will not relieve the patient of the problem.
Causes of pain
After anesthesia, all patients have gum pain. This is a normal reaction of tissue damaged by the needle during pain relief. Pain after an injection can be of varying intensity and duration, it all depends on the individual characteristics of each organism. For one person it will be mild and go away after a few hours, for another it can be intense and last for several days. In both cases, this is a normal condition, it does not require treatment and will go away on its own. But sometimes the gums hurt due to complications of anesthesia.
Infectious process
A healthy person’s oral cavity contains a huge number of microorganisms; during inflammatory diseases, their number increases even more. If a person has a reduced immune system, microbes, penetrating through the injection wound, can cause an infectious process in the soft tissues (abscess, phlegmon). With this complication, in addition to pain, which will be intense, body temperature and/or local temperature at the site of inflammation may increase. Often with abscesses, patients note that the gums are swollen. Depending on the severity of the process, swelling can spread to the facial muscles, causing asymmetry of the nasolabial folds and mouth.
Soft tissue hematoma
If during anesthesia the needle damages a small vessel, the leaking blood can form a hematoma in the gum tissue. Depending on the size of the resulting hematoma, it will put pressure on the surrounding soft tissue with varying intensity, irritating nerve receptors and causing pain. If the bruise is located in the superficial layers of the mucous membrane, the patient may also notice that the gums are swollen. The pain from a hematoma will persist for several days (up to a week) and will go away on its own after the blood is absorbed.
Damage to the nerve trunk
Just like a vessel, a nerve fiber can be injured by a needle during the procedure. After a nerve injury, the gums hurt for a long time, up to several months. The duration and intensity of pain will depend on the size of the injured nerve trunk. With infiltration anesthesia, small endings in the mucosa can be damaged, and therefore the pain will be localized and will go away after a few days. If conduction anesthesia was performed, then there is a risk of injury to a larger nerve that innervates half of the lower jaw at once, so after such an injury, as a rule, the entire innervation zone hurts at once. The pain may radiate to other parts of the oral cavity. Often the pain prevents you from opening your mouth, chewing and talking normally, and it lasts for several months. Facial features may become asymmetrical; in the first days, the patient may also feel that the gums at the injection site are swollen.
Irradiation of pain from the surgical wound
At the site of the operation, tissue and nerve endings are also damaged, accompanied by pain that occurs after the anesthesia wears off. The pain may radiate to neighboring parts of the mucous membrane, and the patient feels that the gums hurt at the site of anesthesia.
Necrosis of the mucosa
In rare cases, anesthesia may be complicated by necrosis of the tissue of the gum mucosa. Necrosis develops as a result of tissue death that occurs for various reasons.
- Poor blood circulation at the injection site, usually due to some chronic diseases (diabetes mellitus, systemic vasculitis).
- A sharp spasm of blood vessels after the administration of a large dose of adrenaline along with an anesthetic can also cause necrosis.
- Too rapid administration of the drug can lead to compression of blood vessels and nerve endings and also lead to necrosis.
- Infectious processes at the injection site, especially those caused by anaerobic flora, can also cause tissue necrosis.
- Medical error when another aggressive agent (alcohol, calcium chloride) is administered instead of an anesthetic.
As a rule, the development of tissue necrosis is accompanied by acute pain already during the injection and forces the doctor to take emergency measures. At the site of tissue necrosis, a wound forms, which hurts and heals for several weeks.
narkozzz.ru
Preventing complications
To avoid having to treat complications, the dentist leaves recommendations, following which the patient can easily avoid the problem of inflammation:
- The cotton swab should be on the wound for 20 minutes or more;
- If the gums are very inflamed , you can apply a cold compress to the cheek, it will prevent or slow down bleeding, the tissues will stop hurting;
- After treatment or tooth extraction, you should not eat for three hours;
- Food should not be hot , salty or spicy, as it can cause severe inflammation of the wound;
- Tobacco and alcohol are also not recommended after oral surgery;
- You need to rinse the wound carefully with a decoction of herbs, which should be at room temperature;
- Warming compresses should not be applied to the sore spot;
- Until the wound has healed , you need to brush your teeth extremely carefully, without touching the sore spot, so that it stops hurting.