Exacerbation of lumbar osteochondrosis is the appearance of unpleasant heaviness, pain, and stiffness of movements that disrupt the usual rhythm of life and force one to limit mobility. In most cases, a working patient with an exacerbation of lumbar osteochondrosis is provided with a temporary disability certificate. Bed rest is prescribed for 5-7 days. Therefore, if you are employed, then you should contact the city clinic and make an appointment with a therapist. He will issue a sick leave certificate, prescribe primary treatment, and conduct a diagnostic examination. If necessary, a consultation with a neurologist will be scheduled.
If you do not work, it is still recommended to carry out treatment if symptoms of exacerbation of lumbar osteochondrosis appear under the supervision of an experienced doctor. You cannot independently, without special diagnostic methods, exclude the possibility of prolapse of an intervertebral hernia. But it requires a slightly different treatment. Therefore, you should first visit a doctor, and then carry out treatment either independently at home, or attend those procedures that are recommended by the doctor.
Exacerbation of osteochondrosis of the lumbar spine can occur suddenly and can be triggered by various pathogenic factors. Most often, this is inadequate physical activity or prolonged positioning of the body in a certain position. When carrying out differential diagnosis, it is important to exclude the possibility of displacement of the vertebral body, sprain of the ligamentous apparatus, rupture of the fibrous ring of the intervertebral disc with the formation of extrusion or hernia. All these pathologies are similar in clinical manifestations to exacerbation of osteochondrosis, but require a more careful approach to complex therapy. All of them are dangerous primarily because toning of the spinal canal can occur with compression of the dural membranes of the spinal cord. In this case, the patient's condition may gradually worsen. Convulsions, numbness in the upper or lower extremities occur, weakness, drowsiness, etc. occur. Only an experienced neurologist can make an accurate diagnosis.
Causes of exacerbation of lumbar osteochondrosis
There are various reasons for exacerbation of lumbar osteochondrosis, but before we look at them, let’s talk about what it is. Osteochondrosis itself is a degenerative dystrophic disease that occurs in a chronic recurrent (constantly developing) form. It affects the cartilage tissue of the intervertebral discs. Each disc consists of a dense shell in the form of a fibrous ring, and a nucleus pulposus located inside it (this is a gelatinous body that maintains the shape and height of the disc, ensures uniform distribution of shock-absorbing load during movements).
The intervertebral disc does not have its own vascular network and receives fluid and nutrition through diffuse exchange with adjacent muscles. If the muscles do not receive regular, full-fledged physical activity, they stop secreting fluid and the fibrous ring becomes dehydrated. A network of small cracks appears on its surface, which are filled with deposits of calcium salts. This prevents complete diffuse nutrition in the future, therefore, without comprehensive adequate treatment, osteochondrosis constantly progresses.
Exacerbation of osteochondrosis is an inflammatory reaction in response to the deterioration of the intervertebral disc affected by dystrophic degenerative changes. The following happens:
- with increased physical activity or under the influence of stress factors (hypothermia of the body, prolonged static stress, emotional shock, overheating, etc.), the microcirculation of blood and lymphatic fluid in the lesion occurs;
- the fibrous ring quickly loses fluid and the height of the intervertebral disc decreases;
- it begins to put pressure on the surrounding soft tissue;
- the body launches an inflammatory response, which is designed to restore microcirculation of blood and lymphatic fluid;
- the surrounding muscle tissue tenses to compensate for the forces of the damaged intervertebral disc.
In this case, the patient experiences a feeling of stiffness and severe pain. In some cases, neurological clinical signs appear.
The main causes of exacerbation of lumbar osteochondrosis:
- heavy lifting (can also provoke a rupture of the intervertebral disc or displacement of the vertebral body in the form of retrolisthesis or antelesthesis);
- a fall from a height or a jump with an unsuccessful landing (sharp compression of the damaged intervertebral disc occurs, which can no longer cope with the shock-absorbing load placed on it;
- prolonged stay in a static position (lying on one side, sedentary work, long flight in an uncomfortable seat;
- Road accident with emergency braking;
- hypothermia or exposure to high ambient temperatures;
- stress or emotional overstrain;
- acute viral respiratory infection;
- back bruise in the lumbar region.
In fact, there may be many more reasons. Often, exacerbation of lumbar osteochondrosis occurs when performing unusual work, for example, when digging a garden or painting walls. This is due to the fact that the muscular frame of the back is not trained and is not ready to compensate for the mechanical and physical stress placed on it. Therefore, most of it falls on the spinal column. If there are damaged areas of the intervertebral discs, then there is a high probability of developing an exacerbation of osteochondrosis.
Causes of pain
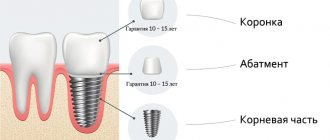
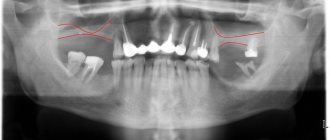
Aching pain after dental implantation can be caused by the following factors:
- Direct surgical intervention and tissue healing after.
- Carrying out some necessary additional manipulations during the operation.
- Failure to comply with medical recommendations for speedy tissue healing.
Sometimes pain can be an individual reaction of the body to the administered anesthetic. Also, there are differences between implantation methods - in a one-stage procedure, the gums are not cut, the jawbone is not drilled and sutures are not placed and, of course, the pain after such an operation is much less and lasts less time. But it is not available in all cases, so classical implantation cannot be completely abandoned.
More information about the implantation procedure can be found here.
Why legs fail during exacerbation of lumbar osteochondrosis
In the lumbar spine there are radicular nerves that are responsible for the innervation of the lower extremities. This is where the sciatic nerves originate. Some of the radicular nerves participate in the formation of a nerve plexus called the cauda equina.
The only reason why legs fail during exacerbation of lumbar osteochondrosis is a violation of innervation. This occurs when the radicular nerve is compressed - in this case, weakness and numbness are determined in one of the legs on the affected side. If both legs fail, muscle weakness and numbness are felt in them, then most likely there is compression of the spinal cord due to spinal canal stenosis. This may be a clinical symptom of an intervertebral hernia formed in the cavity of the spinal canal.
Numbness in the legs can occur when a vertebral body or intervertebral disc is displaced. If a similar symptom appears during an exacerbation of osteochondrosis, you should immediately seek medical help. This may be a harbinger of subsequent paralysis of the lower extremities.
The exception is situations when the patient is prescribed injections of muscle relaxants. These pharmacological drugs act to relax all types of muscles. They also cause a feeling of weakness in the legs. The patient feels as if his legs are giving out. This is actually a consequence or side effect of using muscle relaxants.
Disease prevention
To prevent otitis media, it is necessary to undergo regular medical examinations, maintain personal hygiene, and take care of your ears.
If symptoms of the disease appear, you should immediately consult a doctor. You should also avoid getting water into the ear. If your nose is stuffy, you need to blow your nose correctly, closing one nostril and freeing the other from mucus.
Many experts recommend vaccination for preventive purposes. Pathogenic agents lead to the development of otitis media. To protect yourself from infection, it is recommended to administer the polysaccharide pneumococcal vaccine.
Symptoms of exacerbation of lumbar osteochondrosis
There are certain clinical symptoms of exacerbation of lumbar osteochondrosis, which are absent in the remission stage. It is worth paying attention to the following symptoms of exacerbation of lumbar osteochondrosis:
- sharp pain in the lumbar region, which can radiate to the sacrum, groin, buttocks or thigh;
- limited mobility (impossible to lean forward or straighten up, make body turns, etc.);
- there is stiffness associated with sudden, prolonged muscle tension in the lumbar area;
- palpation of the spinous processes is painful;
- It is impossible to stay in a certain position for a long time.
Neurological signs may appear if the root nerves are pinched. They are expressed in numbness of certain parts of the body and lower extremities, paresthesia, irradiation of pain down to the heel, muscle weakness, etc. In severe cases, the functioning of the intestines of the bladder, etc. may be disrupted.
Specificity of pain in cholecystitis and pancreatitis
With exacerbation of pancreatitis, the pain is girdling in nature, radiating to the left or right hypochondrium. When the entire organ is affected, pain appears behind the sternum and in the back, intestines.
Acute cholecystitis is characterized by pain in the right hypochondrium radiating to the back, provoked by overeating, poor diet, and physical activity. Pain is present in the upper abdomen, an attack of biliary colic occurs, associated with a violation of the outflow of bile.
What to do if the exacerbation does not go away
The first thing to do in case of exacerbation of lumbar osteochondrosis is to consult a doctor who will conduct a high-quality differential diagnosis. Pain in the lumbar region is not always an exacerbation of osteochondrosis. In some cases, the pain may be referred. For example, in women such a symptom often occurs due to inflammation of the appendages, ectopic pregnancy, etc. In men, under the guise of exacerbation of osteochondrosis, urolithiasis may occur or prostate adenoma may develop. Therefore, you should not look for advice on what to do in case of exacerbation of lumbar osteochondrosis; it is better to seek medical help.
Especially if the exacerbation of lumbar osteochondrosis does not go away, and the symptoms only get worse. This may indicate that the treatment was prescribed incorrectly or that the diagnosis was incorrect.
How long does mental pain last?
We discussed here with a friend from LiveJournal our ways of dealing with pain and disease states. I discovered so much that I decided to share. The post contains my own experience and skills of dealing with mental pain. The key word is “my own”, that is, my methods are personal, they may suit some people, but not so much for others.
So, let's go.
The first and most important thing that psychotherapy taught me about living through pain is the very idea that you can somehow settle into pain and experience this state in a special way. Second, and no less important, the pain will end. Definitely and without options.
I won’t be original and will use a hackneyed weather metaphor. In the inner world, just like in the outer world, there is different weather. Rain (in our case, pain) also happens, for sure.
But. You can get caught in a downpour, where icy hail hits, and stubbornly walk forward barefoot, no longer understanding why and where, feeling how your calves are cramping in icy water, dry, prickly bronchitis slowly flaring up in your chest, your body is exhausted by the blows of the ice, and there is only one end. - stumble over the next pothole, finally fall and die, choking in this viscous water under your feet. A very colorful, traumatic and auto-aggressive way to live your life. Sometimes, by the way, it’s useful - with the goal of later discovering that you don’t want to do it that way anymore.
Or it can be done differently. Stop and look around - is there a place where you can hide from the hail? Can someone let you under their umbrella? Is there a store nearby with an assortment of rubber boots - albeit not too elegant and in a different size? Is it possible to drop under some roof, is there a bus stop nearby that will take you to someone’s (even if not yours) house?
Do you feel the difference? Or - automatically, senselessly wander through an atmospheric nightmare - and know that it will always be like this. Or - go into raging bad weather, look for ways to take care of yourself and remember for sure - the weather always changes, without exception, and soon the rain will end, and the wet, sticky, cold will be removed from the body, and the situation will provide an opportunity to warm up and relax.
I repeat - this is perhaps my most important and global discovery about ways to deal with oneself in difficult and painful periods of life.
And now - developed concrete practical ways to deal with pain.
- Notice.
When suddenly something in the body begins to hurt that didn’t hurt before; when there is a lot of tension in the face, and it’s somehow difficult to breathe; when you find that you only have enough strength not to cry; when you don’t want anything, there is a scratching in your chest, and the world gradually takes on the color of various shades of gray - don’t continue to dwell on the remnants of stubbornness, but notice and understand - something is happening. You probably need to stand a little and take a closer look at what exactly it is. The markers here, of course, are mine; they are different for different people, and knowing your pain markers is, in my opinion, a very useful thing.
- Organize support and people.
It’s better, at a minimum, to call, and at a maximum, to come in person to someone close, rather than deal with it yourself. It’s better for many reasons - it’s not so scary, and it’s not so lonely, and right next to you there is that same, warm, familiar, fluffy feeling, and there is someone to lean on. Therefore, I definitely recommend that during periods of life’s difficulties, have in your head a list of people who can withstand your pain, value and respect you, and are ready to devote time to you. Friends who have similar experiences are psychologists. Just a list in my head, or better yet, on paper. I'm serious, yes. Because in moments when it’s really bad, the brain refuses, contacts fly out of the head, and the habit of being alone and/or not noticing oneself wins dry.
Therefore, at a painful moment, we pick up the phone, call our loved ones, check the situation and talk about how we are feeling. Little by little, little by little, we unwind what is bursting from within, listen to questions, answer, meet with experiences that overwhelm the soul and create pain. Let’s not delay, because psychosomatics are more difficult to treat.
- Face the pain and breathe. Breathe. And breathe again - a lot.
Breathing is generally a very useful thing, thanks to it we live, if anyone doesn’t know. And it is thanks to breathing that pain can be experienced quite easily - because inhalation-exhalation, inhalation-exhalation is a very good cycle. Inhale - breathe in fresh air, gain strength - and exhale - exhale from the chest-body-eyes-soul the excess that no longer fits in the body and asks to come out with screams and tears.
In the case when it has already covered you, when it has come and taken over with pain - the sweetest thing is to breathe-scream-cry, the way you want - loudly, with force, so you get tired faster, and the strength runs out, and the crying passes, and peace comes after it .
- Remember with all your might - it will end, much faster than it seems. And it will be much easier.
When I worked with pain, my own or someone else's, and when I saw other people's work, the most acute moment of pain did not even last 15 minutes. Because the body is not made of iron and cannot withstand much, it is quite difficult to cry and worry more than the given time. Therefore, remember with the remnants of your brain in its most broken state - it will be painful, unpleasant - but not for as long as it seems. If you allow the pain to be, then everything will end soon. And then there will be peace, and plenty of room for other experiences - usually much more joyful ones.
This is generally an incomprehensible and difficult thing to believe - but it is absolutely true. When you really experience the pain, everything becomes much easier. Exactly everything - mood, state, life situation (at least, a look at it). And a lot can be changed and done when you have the strength and mood - that is, when you let go of the body and let it experience what has been asking for a long time.
- Walk, move, live.
Sometimes there were moments in my life when I could not cry. There were simply no tears. I also couldn’t speak or explain to anyone what was happening to me. I just felt bad. Really capslock.
And then movement saved me. Go somewhere far away (with a fully charged phone in your hands!), wash, put away, clean, play sports - do something that takes and pulls energy from the body, reduces the intensity and removes heaviness. This method does not bring any great existential discoveries. But it is almost certain that after a long, grueling physical activity you will most likely want to eat and sleep. And it’s already great when you want something. This is life.
- Have a way to slow down. At least - to know that it definitely exists.
At the very beginning, when pain was something new and unfamiliar to me, and the amount of it in my body was off the charts, and supportive people did not exist in my mind as a class, there really was no way out or a stop screen in my subjective reality. Then a way out was discovered.
Since then, I have had a boundary pillar inside me - where I no longer have the strength to understand and think, but for now there remains the opportunity to follow the algorithm that was set long ago and has helped me more than once. The pole is made of thick wood, old and very reliable, with a board firmly nailed to it with the inscription: “Take your medications, hide in a corner and sleep.” I know for sure that this helps me relieve the most acute condition. At these moments, I don’t watch anything about people, I don’t read or hear emotional stories. I have a rest and a stop - because I have a lot.
If you know how to slow down, that's cool. Because in the most difficult, most hopeless situations, you can definitely rely on your experience of stops, after which a new day comes - and it is usually a little better than the one yesterday.
Lyudmila Marchenko.
PS:
- Call those who you need at the moment. Find the strength yourself and call . Give the delusions of grandeur a rest, which believes that only you can care, and others are not worthy of it. There's also the complex of a victim who is unworthy of care. All? And call. It is part of self-responsibility to learn how to organize support for yourself. Grow up, it's fun!
- Let the pain be and it will end. Courage, dear friend, and courage! Yes, this is heroism.
- Erkhart Tolle in support - about physical and mental pain. For example, The Power of Now. I know people whom she helped learn to cope with regular, multi-day physical pain, those whom she helped learn to cope with panic attacks that are not regulated by any medicine, and learn to live with the loss of loved ones. And I am among them.
Breathe. Live. Be afraid and do it.
How to treat lumbar osteochondrosis during an exacerbation
Before treating lumbar osteochondrosis during an exacerbation, try to undergo at least some examinations. An X-ray, CT or MRI examination will eliminate the risk of developing a hernia and protrusion. If osteochondrosis is diagnosed, it can be treated using manual therapy methods. If this is not possible, then with the help of medications you can only relieve the symptoms of the pathology. It is impossible to achieve restoration of a damaged intervertebral disc using pharmacological drugs.
For exacerbation of lumbar osteochondrosis, the following medications are used in treatment:
- non-steroidal anti-inflammatory drugs to eliminate inflammation and relieve pain (“Diclofenac”, “Ortofen”, “Ketorol”, “Baralgin”, “Piroxicam”, etc.);
- muscle relaxants to relax overly tense muscles;
- B vitamins (thiamine bromide, pyridoxine hydrochloride, cyanocobalamin) – there are complex preparations, for example, “Milgamma”;
- nicotinic acid – to enhance microcirculation of blood and lymphatic fluid in the area of inflammation;
- chondroprotectors - for the restoration of cartilage tissue of intervertebral discs (but their effectiveness is very doubtful due to the fact that if diffuse nutrition is impaired, they cannot penetrate into the tissue of the fibrous ring).
There are more effective and safe methods of treating this disease. We'll talk about them later in the article.
Diagnostics
An ENT doctor can suspect otitis media based on its symptoms and look into the ear using an otoscope. A pneumatic otoscope allows you to see if there is fluid behind the eardrum. The doctor directs a weak stream of air onto the membrane. Normally, it should move under this stream, but if the middle ear is filled with fluid, the eardrum will not be able to move.
If the diagnosis is in doubt or it is necessary to determine the condition of the auditory analyzer in chronic persistent otitis media, an ENT specialist can use diagnostic methods such as:
- Tympanometry. With its help, you can measure the degree of mobility of the eardrum, the conductivity of the auditory ossicles (hammer, incus, stapes), and also, indirectly, the pressure inside the middle ear.
- Acoustic reflexometry. This test helps to understand how much the eardrum “passes” sound. The greater the pressure of the fluid in the middle ear, the more sound it will reflect and the less sound it will transmit.
- To find out how chronic ear infections or middle ear effusion affects your child's hearing and development, your doctor may refer you to an audiologist or child psychologist.
Classification of osteochondrosis: stages of progression
The acute period of spinal disease is divided into stages according to localization and symptoms. In total, 4 stages of development of acute spine disease are known in medicine. At the initial stage, osteochondrosis is quite difficult to determine due to mild symptoms.
The patient experiences severe fatigue, which can easily be confused with a host of other ailments. At the first stage, back discomfort is most often observed, which many associate with hard work and overwork. It is for this reason that few people instantly react to a slowly developing pathology in the body.
The second stage is accompanied by the destruction of cartilage tissue, which causes severe pain. If urgent assistance is not provided, the intervertebral space will begin to decrease, which will compress the blood vessels and nerve processes.
In this case, the relief of shooting pains in the limbs or head and acute back pain is carried out only with strong medications. The third stage is accompanied by the development of secondary pathologies such as hernia, scoliosis and kyphosis.
The most dangerous is the last stage, during which the patient can no longer move normally, and any body movements are accompanied by severe pain. The vertebrae are displaced, bone tissue grows, which can lead to disability.
Treatment
The effectiveness of therapeutic measures depends on identifying the underlying disease. In case of infections, an important step is to detect the type of pathogen; only by determining which microorganisms (bacteria, viruses, fungi, protozoa) caused the disease can one count on success in treatment and full recovery and restoration of male power.
Neurogenic disorders must be corrected in sessions with a psychotherapist or psychologist. Anatomical or traumatic defects are treated using surgical manipulations or operations.
Diseases and damage to the liver that may be accompanied by abdominal pain:
- Acute toxic hepatitis: can develop as a result of toxic substances entering the body with food, which results in acute damage to liver cells - hepatocytes. The disease may be accompanied by pain in the right hypochondrium of low intensity, and there may be jaundice.
Further, after the duodenum, food enters the small intestine, where further digestion occurs with the participation of pancreatic enzymes and bile. From the small intestine, the contents pass into the large intestine, where water is absorbed and further formed from undigested particles of feces and removed from the body. Abdominal pain near the navel may be associated with functional disorders and intestinal diseases. Pain in the lower abdomen is also characteristic of this pathology.
Emotional and physical pain
Over time, any emotional pain, if not eliminated, manifests itself as illness, both mental and physical.
Physical pain is a signal of cell destruction in the human body. Unlike emotional pain, such pain passes and is forgotten, but not always.
It also happens that physical and emotional pain act as one whole. For example, a person has kidney cancer. Experiencing physical pain when the kidneys are destroyed, he simultaneously suffers from emotional pain, caused in turn (in most cases) by the feelings (energies) of resentment or guilt that gave rise to this disease. In this case, a person is subjected to double destruction at the same time: mental and physical.
Emotional pain is the influence of unfavorable energies (negative feelings) on the spiritual component of a person, which can be represented as an energy shell that contains all these feelings.