797
According to statistics, damage to the inferior alveolar nerve (IAN) during dental implantation is not so rare.
We will tell you in our publication how such neurological complications of dental treatment manifest themselves and what the risks are.
Probability percentage
Statistics on damage to the NAS during dental implantation seem contradictory. According to some studies, nerve damage occurs in no more than 3% of cases. Other data suggests that this happens in 30-40%.
This variability is explained by the fact that the statistical results depend on many factors - the calculation method, the age group of the patients undergoing the examination, the time period during which the information was collected, and some others.
If we consider all cases of damage to the NAS during dental intervention, then the frequency of their occurrence, depending on the cause, is in the following order:
- conduction anesthesia;
- removal of third molars;
- entry of filling material into the canal with NAS;
- surgical intervention (periostitis, resection of the apex of the tooth root, etc.);
- implantation.
However, it has been established that in older age groups, implantation takes first place in the frequency of damage to the mandibular nerve.
There is one more factor that influences the statistical results. The later the data is taken, the lower the percentage of damage to the NAS during implantation, and this is quite understandable.
The implantation of artificial roots is becoming an increasingly popular technology, the qualifications of doctors are improving, safer technologies are being used, and high-tech diagnostic equipment is being used.
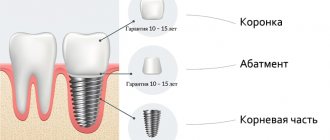
How to properly organize nutrition after dental implantation and a sample menu for the day.
Come here to find out how long does a tooth hurt after implantation.
At this address https://zubovv.ru/implantatsiya/metodiki/unikalnyie-vozmozhnosti-skulovoy.html we will consider the technique of zygomatic dental implantation.
Symptoms of the lesion
Numbness of the face and pain symptoms are signs of damage to the mandibular nerve
- numbness of the face from the implantation side: lower lip, chin, tongue, lower teeth, cheeks;
- pain in the implant area;
- the appearance of profuse salivation;
- choking when eating or drinking;
- the occurrence of facial expression and articulation disorders.
A person feels discomfort when caring for facial skin (unpleasant sensations during shaving, applying makeup). Clinical manifestations depend on the type of injury and the depth of the lesion.
Causes
The mandibular nerve fascicle is one of the branches of the trigeminal nerve. It is located in the canal of the lower jaw, below the tooth roots.
The NAS innervates the lower lip, mandibular teeth and adjacent soft tissues, chin, and external ear. This means that it is in these areas that pathological sensations caused by damage to the NAS occur.
The main structural element of any nervous tissue is the nerve fiber. Individual fibers are collected into bundles covered with perinervium. The fascicles form groups surrounded by epineurium.
The membranes of the nerve trunk (perineurium and epineurium) protect it from possible damage, however, under strong mechanical stress they can only weaken the damaging factor.
The following types of damage to the NAS are distinguished:
- compression (squeezing);
- stretching;
- partial intersection;
- complete intersection.
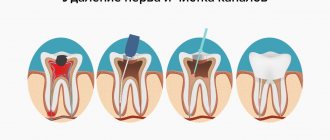
Damage to the NAS during implantation occurs during preparation of the implant bed and installation of the implant.
This is usually the result of poor planning or errors made when drilling into the bone and screwing in the implant. Moreover, the nature of the lesion can be anything - from compression to complete intersection.
Diagnosis of the disease
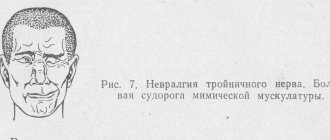
The diagnosis of trigeminal neuralgia is established by a neurologist . A preliminary diagnosis is established based on the patient’s characteristic complaints and typical medical history.
During the examination, the neurologist pays attention to the presence of specific complaints and symptoms.
What patient complaints are taken into account when collecting anamnesis?
The presence of typical complaints in a patient with trigeminal neuralgia is decisive in diagnosis.
The patient complains of the following:
- paroxysmal, severe pain in one half of the face, it alternates with light intervals;
- the appearance of pain is preceded by itching, redness of the facial skin or goosebumps;
- exposure to the trigger zone provokes an attack;
- the pain is burning, occurs suddenly, is comparable to the passage of an electric current and never changes its character.
In the anamnesis, the patient indicates a head injury or herpetic rashes on half of the face, where pain is bothersome.
How is a facial examination performed by a doctor?
Neurologists, along with a general neurological examination, examine in detail the functions of the cranial nerves.
When examining a person, he pays special attention to the following signs:
- the exit points of the trigeminal nerve of its three branches are examined (on the forehead, near the nose and on the chin);
- a search is underway for trigger zones that trigger an attack of pain;
- decreased superficial sensitivity on the skin of half the face.
On examination, there is no neurological deficit (signs of damage to neurological structures). The doctor will rule out other causes of pain during the examination.
Laboratory research
The patient is prescribed standard general clinical laboratory tests (complete blood count, urinalysis, blood biochemistry) and no changes are detected.
There are no specific laboratory tests for trigeminal neuralgia. These methods are used for differential diagnosis with viral lesions of the nervous system.
Instrumental examination methods
In the diagnosis of trigeminal neuralgia, instrumental examination methods are widely used.
X-ray
To diagnose damage to the trigeminal nerve, they are used to diagnose pathological formations that pinch the nerve.
For this use:
- x-ray of the skull in two projections;
- panoramic photograph of teeth.
With their help, diseases of the dental system, manifested by severe toothache, are identified.
CT
On a computed tomogram you can see bone formations that have a pathological effect on the branches of the trigeminal nerve. You can also identify narrowing of the bone holes through which the nerve branches pass.
MRI
This examination identifies formations that can impinge on the trigeminal nerve.
Search is underway:
- tumors;
- cysts;
- foci of demyelination.
This method identifies neurovascular conflict in the area of the trigeminal nerve.
Electroneuromyography
Using electroneuromyography, defects in the conduction of electrical impulses along the nerve fiber and foci of demyelination are detected.
Ultrasound
A search is underway for formations in the soft tissues of the face that put pressure on the branches of the trigeminal nerve.
First signs
Symptoms depend on the extent and type of damage. The following manifestations are distinguished:
- Paresthesia. It is characterized by the fact that unusual sensations (numbness, tingling, “goosebumps”) occur in the innervated area (lower lip, chin, gums and cheeks).
Paresthesia is divided into hypoesthesia (abnormally low sensitivity to stimuli, such as absence of pain when a needle is given) and hyperesthesia (excessively high sensitivity). As a rule, the sensations of paresthesia are not uncomfortable.
- Dysesthesia. A distortion of sensations in which ordinary touch can give a sensation of pain, and where the patient should feel mechanical pain, he feels a burn.
- Anesthesia. Complete lack of sensitivity.
During implantation, the lingual nerve, which is located in the mucous membrane of the gums, located lingually in the area of the chewing teeth, can also be damaged. This happens rarely, in about 1% of cases, however, you need to know about it.
Damage to the lingual nerve manifests itself as burning of the tongue, drooling, numbness, changes in speech and taste. Tongue biting may occur. As a rule, damage to the lingual nerve is low-risk and goes away on its own within a few weeks.
Clinical picture
Temporal tendonitis symptoms appear gradually. At the initial stage, mild pain occurs when chewing food. Their intensity increases with the development of the inflammatory process. In the places where the tendon attaches to the bone, a swelling forms, spreading to healthy tissue. Swelling compresses sensitive nerve endings, increasing pain, and disrupts the functioning of muscle fibers. A person’s usual rhythm is disrupted due to the inability to eat food. The following clinical manifestations are characteristic of the disease of moderate and high severity:
- formation of a compaction in the area of the affected tendon;
- redness and smoothing of the skin over the swelling;
- pain that occurs when palpating the seal;
- malocclusion;
- crepitus (crunching and clicking) when moving the jaw;
- irradiation of painful sensations to the temples, frontal lobes, bridge of the nose, and the back of the head.
When a tendon becomes infected, symptoms of general intoxication of the body often occur. Pathogenic bacteria begin to grow and multiply, releasing toxic products of their vital activity into the bloodstream. The patient's temperature rises above 38 °C, fever, chills, and excessive sweating appear. Against the background of hyperthermia and pain when chewing, appetite decreases, digestion and peristalsis are upset. A person gets tired quickly, feels constantly drowsy, and suffers from headaches.
Chronic temporal tendonitis is not characterized by pronounced symptoms. Occasionally, mild pain is felt, and there is a slight swelling over the inflamed tendon. But with the slightest decrease in immunity, a relapse of the pathology occurs, accompanied by acute paroxysmal pain. If chronic tendinitis is left untreated, irreversible degenerative changes begin to develop in the tendon.
Classification of conditions
In 1943, the Englishman Seddon described 3 types of nerve damage:
- Neuropraxia. Stretching or compression of fibers without breaking the membranes (perineurium and epineurium). This is a benign, reversible condition that does not cause degeneration of nerve fibers or impair their functions. Completely curable.
- Axonotmesis. More severe damage with disruption of axons (the processes of the nerve cell that transmit impulses) and degeneration of peripheral structures, but with preservation of the main functions of the nerve. Axonotmesis requires long-term treatment, but most often ends successfully.
- Neurotmesis. Complete rupture of the nerve with degeneration of the affected area and replacement of its structures with scar tissue. Requires surgical treatment. The timing of it is very important; if it does not happen within the first year, then it becomes useless in the future.
Features of manifestations of iatrogenic damage to the trigeminal nerve
- Painful discomfort, changes in sensations, numbness (anesthesia).
- Functional consequences - Patients who experience pain from touch or cold often have difficulty with daily functions: kissing, communicating, speaking, eating and drinking, etc.
- Psychological consequences - patients develop various anxiety, fear, anger, post-traumatic stress disorder. Psychological disorders can be aggravated in cases where informed consent for implantation, endodontic treatment, orthognathic surgery, etc., which specifically indicates possible nerve damage, has not been signed before medical intervention.
Rice. 6. Schematic representation of the relationship of the branches of the inferior alveolar nerve with the formed implant bed. Pain during drilling is an important diagnostic criterion for the proximity of the nerve.
Ways to assess case complexity
In diagnostic studies for neurological lesions, 2 types of testing are used:
- mechanoceptive;
- nociceptive.
Using the first, the reaction of tissues innervated by the NAS to mechanical stress is checked:
- The brush test involves lightly passing the brush across the lips and asking the patient to determine the direction of movement of the brush.
- The two-point stimulation method is based on the use of a probe with two legs, the distance between which varies in 2 mm increments. By touching the legs to the skin, it is determined at what distance between them the patient ceases to feel each point of contact individually.
Nociceptive studies can determine pain and temperature sensitivity. Pain sensation is tested using a pin, temperature sensitivity is tested using ice and the handle of a dental mirror heated to a temperature of 43 °C.
A study of taste sensations is also carried out using sugar and salt sprinkled on a cotton pad.
To compare the results, not only the affected area is checked, but also the opposite side of the face.
The essence of the method of compression dental implantation and the dental structures used.
In this article we will tell you what alternatives to dental implants exist.
Here https://zubovv.ru/implantatsiya/metodiki/vliyanie-stabilnosti-vnutrikostnyih.html we will consider ways to determine the stability of implants.
Therapeutic effects
Treatment of patients diagnosed with inflammation of the trigeminal nerve must be urgent: painful attacks that have a tearing, burning nature of high intensity exhaust a person. Their sudden appearance, the presence of trigger points that the patient is afraid to touch, lead to the development of neuroses, phobias, hypochondria, and depression.
Treatment, which is carried out in a hospital setting, begins with the use of anticonvulsants, which are classically used in patients with epilepsy. These medications form the basis of therapy. To enhance their actions, antihistamines are prescribed simultaneously with them. For elderly patients, in order to avoid the occurrence of cerebral circulatory failure, antispasmodics and vasodilators are prescribed.
Treatment is supplemented by the administration of B vitamins - known to support the brain and nervous system - usually for 10-15 days, but in serious cases longer use is recommended.
In case of very severe exacerbation, the administration of sleeping pills is recommended.
Acute attacks are also exposed to electrophoresis with novocaine, codeine, phonophoresis with analgin, as well as UHF (pictured).
Novocaine blockades with this form are, as a rule, ineffective.
The practice of alcoholization of the trigeminal nerve (alcohol-novocaine blockade) is now not widespread due to the large number of delayed complications - increased pain in the acute stages, reduced remission time. This method is considered destructive.
Treatment of less pronounced attacks is indicated using transcutaneous electrical neurostimulation procedures, the principle of which is to apply impulses to the affected area. Pain in 70% of patients disappears or decreases by 10–11 hours.
When all measures are ineffective, surgical treatment is indicated. They use the method of treating the nerve with nitrogen, thermorizotomy, in which the gasser node is destroyed, as well as decompression of the nerve root (if it is affected by a pulsating vessel).
Treatment concept
The method of treating the pathological phenomenon depends on the nature of the lesion and symptoms. In general, there are four tactics:
- Observation (for minor symptoms).
- Drug therapy.
- Implant removal.
- Surgical intervention.
If there is visible damage (most common with implantation), it should be repaired as quickly as possible. The operation, if necessary, should be carried out within a year. After this period, it becomes useless due to irreversible changes in the nervous tissue.
Drug treatment includes:
- anti-inflammatory therapy with glucocorticosteroids (dexamethasone);
- pain relief (nurofen, ibuprofen);
- hydrogen pump blockers.
Removing an implant is usually associated with great doubt, since it can be difficult to determine whether surgery is actually necessary or not. What is at stake is the loss of results from a lengthy and expensive operation such as implantation.
If it is determined that removal is truly necessary, this should be done as soon as possible. The greatest effect is obtained when the dental system is removed in the first 1.5 days.
The essence of surgical treatment lies in the following effects:
- Elimination of compression (squeezing) of the nerve.
- Excision of a neuroma (tumor of nervous tissue), if found.
- Transplantation of the affected area of NAS.
The speed of diagnosis is very important for the success of the operation. Delay in treatment can trigger the development of carpal tunnel syndrome, which is characterized by constant aching pain due to compression of the nerves.
Therapy
Treatment should begin with a mandatory visit to the attending physician. You should make an appointment with a therapist (pediatrician, if we are talking about a child’s illness), and he will write out all the necessary referrals to other doctors.
Medicines
The main therapy is aimed at eliminating pain, inflammation, and preventing destruction of the temporomandibular joint. For this purpose, drugs of the following categories are prescribed:
- non-steroidal anti-inflammatory drugs;
- analgesics;
- glucocorticosteroids, if non-steroidal anti-inflammatory drugs do not produce the desired effect;
- chondroprotectors, which strengthen bone tissue and prevent joint destruction;
- multivitamins.
Treatment also involves the use of physiotherapeutic methods of treatment: massage, exposure to a magnetic field, acupuncture, etc. The duration of treatment directly depends on the symptoms and can take from 2 weeks to 6 months.
If the disease has led to jaw deformation (and its displacement), then conservative treatment is no longer provided - the patient is sent for surgery, and the joint is replaced if necessary.
Folk remedies
Among the traditional methods of treatment, the most effective are:
- Cold compresses with chamomile. You can freeze the broth and use it.
- Salt compresses: for 1 glass of water, 1 tbsp. l. salt. Soak a compress in the resulting mixture and apply to the place where the pain is most pronounced.
- Turmeric – consume about 2 g per day in any form. Helps relieve inflammation.
- Eucalyptus oil. Rub into the area of the affected joint using massage movements.
It is not recommended to use traditional methods of treatment without medical consultation, since if the patient’s diagnosis was made incorrectly, this will only prolong the destructive process.
Experts' forecast
The prognosis for damage to the NAS is uncertain and depends on the degree of damage to the nerve structures. With neurotmesis, it is unfavorable; neurosensory changes most often cannot be stopped.
Axonotmesis - with adequate treatment, nerve sensitivity is partially restored within 2-4 months.
With neuropraxia, complete restoration of normal sensitivity occurs within a few days or weeks.
The main treatment for severe neuropathies is surgery, leading to success in 50-80% of cases
.
What methods are used in treatment
The treatment method depends on the extent of the lesion and is carried out after assessing the sensitivity deficit. With neuropraxia, recovery occurs on its own within 4-6 weeks. No medical attention is required since the nerve structure is not damaged.
With partial degeneration, symptoms subside two months after the injury. For a complete recovery, medical measures will be needed. Numbness for 9-12 months is dangerous due to irreversible degeneration of nerve cells. Microsurgical treatment can be urgent (for an open injury) or planned (for a closed injury).
- For numbness that does not go away for three months - suturing, transplantation;
- For dysesthesia (perversion of sensitivity) for more than 3 months - revision, decompression, neurolysis, suturing and nerve transplantation;
- If hypoesthesia (decreased sensitivity) lasts for more than 3 months, partial unscrewing or removal of the structure, revision, transplantation, suturing is indicated.
Antineuralgic drugs to relieve inflammation of the nerve
- Antineuralgic drugs:
- Carbamazepine;
- Phenytoin;
- Baclofen.
- Local products:
- ointments with capsaicin;
- acupuncture;
- electrical stimulation;
- physiotherapy.
Preventive actions
The main prevention of NAS lesions is adequate diagnosis before implantation. It is necessary to establish the exact location of the mandibular nerve, and if there is a risk of damage, take measures to eliminate complications.
The most important factors in preventing damage are the following:
- Accurate pre-implantation diagnosis , correct planning and competently carried out implantation.
- During diagnosis, the location of the mandibular nerve must be determined and ways to bypass it must be outlined. The use of CT scanning and a surgical guide virtually eliminates the risk of damage.
- During implantation , it is necessary to ensure at least a 2 mm gap between the nerve bundle and the instrument/implant.
- When creating a bed and fixing the implant, excessive force should be avoided .
An important factor in ensuring safety is the high qualifications of the doctor performing implantation.
The video shows a diagram of the movement of the mandibular nerve during dental implantation.
Injury Prevention
The main preventive measure is a complete, correct examination of the dentofacial apparatus before implantation. The exact position of the mandibular nerve must be established, and if there are risks, measures must be taken to eliminate this.
The highly qualified doctor, his knowledge of the topography of the maxillofacial system, the location of the nerve trunks, and good command of conduction anesthesia are also factors that exclude the occurrence of pathology.
Preventive measures to prevent traumatic neuropathy:
- Correct choice of implantation system.
- Comprehensive diagnostics using CT, building a three-dimensional model of the jaws, making a surgical template.
- Proper planning of the operation.
- Pre-implantation confirmation of the mandibular alveolar nerve pathway in accordance with the radiograph.
- Ensuring a distance of 2 mm between the drill (implant) and the nerve. If necessary, shorter implants should be used. It must be taken into account that the length of the drill indicated in the marking is given without taking into account its tip, which is 0.4-1.5 mm long.
- The use of stoppers that limit the amount of immersion of the drill into the bone.
- Avoiding excessive force when drilling and installing the implant.
- Exercise caution when implanting in the area of the posterior teeth of the lower jaw to avoid damage to the lingual nerve.
Skeletonization of the alveolar bone should be carried out carefully, do not make incisions in the mucous membrane from the side of the tongue, and do not stretch the mucoperiosteal flap too much. When performing an osteotomy (preparing the bed), it is necessary to maintain a safe distance from the lingual nerve.
The doctor is required to have the patient's informed consent for implantation. The document should contain information about preoperative neurosensory sensitivity in order to exclude existing nerve pathologies.
The video shows a diagram of the movement of the mandibular nerve during dental implantation.
Prevention is high-quality preparation for surgery and professional performance of manipulations. A thorough study of the structure of the patient’s mandibular canal, the parameters of the alveolar process and the topographical position of the nerve fiber prevents neurological complications.
Carrying out a computed tomography scan as preparation for implantation
Complications will be avoided:
- correct formation of the implant bed;
- careful implantation of the dental structure;
- lateralization (change in the position of the nerve) when it is close to each other.
Reviews
Damage to the mandibular nerve is a very unpleasant complication of implantation, although it is relatively rare.
If you have experienced it yourself, please share your experience of overcoming it. You can do this by leaving comments at the bottom of the page.
If you find an error, please select a piece of text and press Ctrl+Enter.
Tags: implantation, complications of implantation
Did you like the article? stay tuned