Indications and contraindications
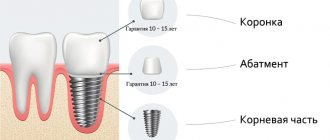
The structure itself consists of a titanium screw and an abutment on which the scab is placed. In order for the product to take root, not only the qualifications of the master and the quality of the dental implant are important, but also the patient’s compliance with all requirements during the recovery period.
Service life of implant parts
Dental implantation is performed only when necessary. It is determined by the doctor after conducting a complete diagnosis and collecting the patient’s medical history. Implantation of artificial roots is carried out for the following indications:
- Single dentition defect;
- The need to create support for removable prosthetics;
- Complete edentia;
- The desire to make your smile more aesthetically pleasing.
All contraindications to such a procedure can be divided into absolute and relative. In the first case, the operation is prohibited. Dental implantation should be completely abandoned in the following clinical situations:
- Bruxism;
- Tuberculosis in open form;
- Serious pathologies of the cardiovascular system;
- Low protective functions of the body;
- Deviations in the functioning of the hematopoietic organs;
- Presence of malignancy;
- HIV;
- Venereal diseases;
- Stage 1 diabetes mellitus.
Relative contraindications may indicate that there is a risk of an adverse outcome. However, the operation can be carried out if all precautions are taken. Such contraindications include:
- Diabetes mellitus 2 degrees;
- Predisposition to an allergic reaction;
- Osteomyelitis;
- Pathological bite;
- Precancerous condition of oral tissues;
- Infection.
Relative contraindications include the period of bearing a child. If the situation allows, it is better to carry out implantation after the birth of the baby.
Single-stage implantation
This technique arose as a development of a one-stage method. This is the name of the technology for restoring lost teeth, when an implant is installed immediately after tooth extraction, in the remaining socket. There is no need to puncture or injure the tissue. The method is especially relevant for restoring the front teeth - the defect is eliminated in the shortest possible time, the treatment achieves a high aesthetic result, excluding loss of bone tissue volume.
Advantages and disadvantages
Dental implantology is a field that has many advantages. After the operation, the aesthetic appeal of the smile is completely restored. This procedure is low-traumatic and reliable. After installation of the implant, the patient can speak and eat normally.
Despite the huge number of advantages, implantation of implant structures has the following disadvantages:
- There is a risk of implant rejection (less than 5%);
- A large number of contraindications;
- Duration of the procedure;
- High price.
The implant may not take root due to the individual characteristics of the patient, due to proper oral care, due to the use of low-quality material, or due to improper installation. In particularly advanced cases, the duration of the procedure can reach six months. The cost of installing an implant is much higher than performing simple prosthetics.
One-stage implantation
The difference between the technique is the installation of a temporary crown on the implant that has just been inserted into the bone. This crown is aesthetically pleasing and can be chewed on. The one-stage implantation method is used in the presence of bone atrophy, when a damaged tooth cannot be saved.
The difference between the method lies in the installation procedure: the abutment of the implanted implant remains above the gum tissue. In this case, there is no need to re-cut the gums - you can simply install a crown on top. Prosthetics are performed 2-3 days after installation of the implant.
Types of implants
There are different models of implant structures. Each of them is intended for a specific clinical case. The following varieties are distinguished:
- Classic;
- Short;
- Mini implants;
- Intramucosal;
- Basal;
- Zygomatic.
The classic type of root implants is presented in the form of an elongated cylinder or tooth root. Their length is 6−7 mm. Such products can be used in almost all clinical cases. In areas with minimal bone tissue, short implants of 3–6 mm are installed. Their stability and reliability is ensured by their large width.
Classic and basal
Extended basal products are installed directly into the basal bone. They take root best in patients with diabetes and smokers. Zygomatic varieties are placed in the cheek bone. Used when the amount of bone tissue is minimal. They serve as an excellent fixation for a bridge or fixed prosthesis.
Mini-implants are used to create temporary support for prosthetics or as additional reinforcement for installing braces.
Mini implants
Intramucosal models are fixed not in the bone tissue, but in the mucous membrane. Most often they are used to fix removable dentures in elderly people.
Pros of use
One-stage implantation has several positive differences:
- Immediately after the problem tooth is removed, an implant is installed;
- the aesthetics of the appearance of the dentition is quickly achieved; a temporary prosthesis is used for this;
- the number of surgical procedures has been reduced;
- as a result, a good cosmetic effect is achieved;
- it is convenient for the doctor to work with the gums;
- no need for gum surgery;
- there is no need to change the configuration of the gum, since its original contour is preserved.
- There are no bite problems that can occur with two-stage implantation;
- the body quickly gets used to the installed structure;
- surgery is only required once, reducing stress for the patient.
- from an economic point of view, there is also a benefit - you will not have to pay for medications for the operation a second time;
Disadvantages of the technique:
- the method is suitable for the absence of 3 or more teeth in a row;
When choosing any technique, it should be taken into account that the process of osseointegration of the implant takes place as standard:
- for the upper jaw for six months;
- for the lower one - within 3 months.
Until this process is completed, it is not advisable to carry out permanent prosthetics and give full loads. Often, instead of a temporary structure, a permanent prosthesis is installed only after 12 months.
Implantation methods
The result of the manipulation depends not only on what type of implant was chosen, but also on the technology of implantation. There are several methods for carrying out such a procedure, each of them has its own advantages and disadvantages. Implantation methods do not require preliminary grinding of healthy teeth that are located nearby.
Two-stage implantation
This method is considered classic in dental implantology. It is excellent for almost any clinical case. Both regular root-shaped implants and short ones can be installed. The main difference between the two-stage technique is that it allows the product to gradually take root in the bone. This approach is more gentle on the patient’s body and ensures successful engraftment.
Initially, the doctor prepares the bone bed for the installation of cylindrical or screw implants. To do this, mucoperiosteal flaps are removed and a small depression is created in the tissue itself. A guide channel is installed in the bone, which is then expanded. After preparing the bone bed, an implant is screwed into it, on top of which a plug is installed. All mucoperiosteal flaps are returned to their place, and the wound is sutured. The entire procedure takes about 1 hour.
Classic scheme
The healing period can last from 3 months to six months. The second stage of implantation is installation of the support head. To do this, incisions are made on the mucosa, the plug is removed and a gum former is mounted, which is then replaced with a supporting head.
The disadvantage of this technique is that it does not allow you to instantly restore a lost tooth. However, in this case, survival is better, and the risk of complications is much lower.
One-step procedure
This method involves installing a temporary crown directly on the implanted implant. Not all types of products are suitable for such an operation, since some of them cannot provide the required level of stability.
One-step installation
One-stage implantation occurs in the following way:
- On the day of tooth extraction, an implant, abutment and temporary crown are installed.
- Over the course of six months, the process of gum formation and engraftment of the product occurs.
- After final healing, an abutment is made to suit the individual characteristics of the patient and a permanent crown is installed.
This procedure has many names: express, instant, one-step implantation. The essence of the technique is that both tooth extraction and temporary crown installation are carried out in one visit to the doctor.
Laser and basal technologies
Some doctors consider the laser method of manipulation to be a separate type, but in fact it is a simple addition to the two-stage technique. In this case, the gum is cut not with a scalpel, but with a laser. Consequently, the operation is bloodless, and the risks of developing an inflammatory process are minimized.
The peculiarity of basal implantation is that instead of conventional root-shaped products, long basal ones are installed. They are screwed into the bone and the prosthesis is immediately installed.
Basal technology involves performing manipulation in one stage. Its advantages include the following nuances:
- Installation of an implant immediately after tooth extraction;
- Less traumatic;
- Installation of a temporary prosthesis on the day of implantation of the product;
- The dentition looks aesthetically pleasing immediately after manipulation;
- There is no need to carry out sinus lifting and other additional procedures that involve bone tissue augmentation;
- Restoration of chewing function occurs in a short time.
Due to the fact that the implant is installed in dense basal bone, its stability and reliability increases several times. The permanent prosthesis is installed one year after successful implantation. It is recommended to use metal-ceramic crowns as a prosthesis.
All-on-4 method
The peculiarity of this technique is that it allows you to install a prosthesis for the entire jaw on 4 implants. To do this, 2 products are implanted at a right angle, and the other two - at an angle of 30-45 degrees on the sides. Most often, this method is used for elderly patients or those with minimal bone tissue.
All-On-4
The advantages of such implantation are as follows:
- prosthetics will take from 4 to 5 days;
- no need for bone tissue augmentation;
- reliable fixation of the prosthesis using screws;
- correct load distribution on all implants.
The cost of this type of implantation is much lower than installing an implant for each tooth separately. This is an excellent opportunity to restore teeth if they are completely lost. The period of adaptation is as short and comfortable as possible.
Abstract: Intraosseous dental implants
homeAPPLICATION OF IMPLANTS WITH BIOLOGICALLY ACTIVE POROUS POWDER COATING.
INTRODUCTION
Intraosseous dental implants are an effective means of eliminating dentition defects. The main problems when creating and installing implants are the compatibility of the implant material with bone tissue, preventing its rejection, as well as the integration of the implant body into bone tissue with the maximum possible coincidence of the biochemical characteristics of the latter with the natural tooth root.
The abstract describes some factors that influence and increase the osseointegration of dental implants.
Tests in clinical conditions of dental clinics, both in Russia and abroad, for many years, have shown the effectiveness and prospects of using implants with biologically active porous powder coating. A thin biologically active layer with a certain porous structure, surface morphology, and adhesive-cohesive properties is formed on the surface of such an implant. When such implants are introduced into the bone tissue, the bone effectively grows into the pores of the coating, or, more precisely, during the healing process, a thin porous powder layer, for example, hydroxyapatite ceramics or another composition on a compact basis, is integrated with living tissue. This ensures strong and long-term fixation of the implant. and its normal functioning in the body. A transition layer of titanium powder is applied to the titanium implant base using plasma spraying technology, and then a layer of biologically active ceramics. Thanks to the distribution of ceramics over the porous structure of the metal, strong fusion with the recipient’s bone tissue is achieved, as well as chemical and physiological stability, which allows us to consider this system as ideal for intraosseous implantation. Let us note the main advantages of implantation over traditional prosthetic methods:
the possibility of unpreparing healthy teeth to support dentures;
the possibility of manufacturing long-term fixed dentures;
no need to preserve diseased teeth, etc.
Ceramic implants have certain advantages over metal ones. This is due to the possibility of connective bone tissue growing into them, replacing part of the implant with newly formed bone tissue, since ceramics in its structure and properties are closer to bone tissue than metal. However, the depth of bone tissue ingrowth into a ceramic implant is small due to the lack of a porous structure. Properties of ceramics such as strength, hardness, and fragility make it difficult to manufacture implants with complex geometric shapes. In this regard, at present, ceramics have not found wide application in the manufacture of implants and their use in clinical practice.
Recently, there has been significant interest in studying the possibility of using inorganic components of bone tissue - hydroxyapatite (HA) and tricalcium phosphate (TCP) for intraosseous implantation. These materials, especially the first one, have not only excellent biocompatibility, but also the ability to easily dissolve in bone tissue, actively stimulating bone formation.
The use of titanium implants with plasma hydroxyapatite coating has shown an increase in osseointegrative properties. This has been established through research.
Example: The objective of the study was to compare the osseointegrative properties of titanium implants. A total of 8 types of implants were prepared: 1 with a smooth surface, the second with a surface that has uneven outlines due to sandblasting, the third with a porous surface formed by the application of titanium particles, and 4 to 8 with the same porous surface as the third, but with hydroxyapatite applied using plasma spraying. The differences in implants No. 4, 5, 6 and 7 were in the pore sizes on the surface - from 50 to 200 microns. Implants in the form of a cylinder with a height of 3 and a thickness of 1 micron were inserted into holes of the same size made in the distal epiphysis of the femur. (The studies were carried out on rats.) The rats were killed by an overdose of hexenyl at 15, 30, 60 days after surgery, an isolated fragment of the femur with an implant was fixed in glutaraldehyde in cocadylate buffer and studied using scanning microscopy.
It was found that a smooth implant does not have osseointegrative properties. The uneven surface relief of the implant weakly enhances this effect, but it manifests itself to a significant extent in all groups of implants with HA sprayed onto their surface. On the same implants, on the surface of which there was no HA, no connection of bone tissue with metal occurred.
The morphological sign of osseointegration is the filling of the space between the covering structures, enclosing them in the internal sections of bone trabeculae. During the observation process, on the 30th and, especially, on the 60th day of the experiment, a gradual smoothing of the crystal structures occurred due to small crystals 1-3 microns in size. In some large granules, the appearance of “corrosion” in their surface is noted. No pathological changes were found in the surrounding bone tissue.
Thus, the results of complex studies have shown a significant increase in the osseointegrative properties of implants with hydroxyapatite applied by plasma spraying.
When designing implants, it should be borne in mind that living tissue grows in the porous structure of the surface layer, while a direct mechanical connection is formed between the bone and the implant. Bone tissue also grows through the holes in the walls of a hollow cylindrical or flat implant, as shown in Figure 1. During replacement defect, the implant is eventually implanted into the bone tissue to form a strong biomechanical connection. It is also important to note that bone tissue has pores and in dynamics (with deformation) the pore volumes change. When replacing a defect in the dentition with an implant, a bone-implant system is formed on its surface, which, after growing into the pores of the implant, the bone substance must also retain the properties of high plasticity and does not collapse under repeated alternating clinical loads.
Comprehensive studies have shown that the predominance of fibrous, cartilaginous, osteoid or bone structures in the area of contact with the implant depends not so much on the material as on the quality of the primary (during implant insertion) contact, which is determined by the amount of interference. It is known that the optimal interference (relative deformation) in the contact zone is 0.09-0.14 µm.
PROPERTIES OF HYDROXYAPATITE
When making ceramics, they try not to use additional binders. Porous substances formed from hydroxyapatite powder are compacted, crystallized and recrystallized at high temperatures (1473-1573 K), and sometimes with the application of pressure. Depending on the purposes of using synthetic hydroxyapatite, different requirements are imposed regarding such properties such as phase and chemical purity, crystallinity, defectiveness, porosity, etc.
If hydroxyapatite is introduced into a bone defect, then there is no need to ensure its structural perfection (stoichiometric composition and high degree of crystallinity). In bone tissue, we are talking about defective HA, with a large number of vacancies and substitutions in the structure, as well as amorphous material as the most defective.
If HA is used as an inert material introduced into the body, then the main requirements for it are biological compatibility and absence of resorption. In this case, it is necessary to use stoichiometric hydroxyapatite with a high degree of crystallinity. Such hydroxyapatite is introduced into the composition of filling materials when it is necessary to bring the physical and physico-chemical properties of the filling as close as possible to the properties of dental tissues.
A significant increase in the efficiency of osseointegration is provided by “replanting” titanium implants with tricalcium phosphate (TCP) and hydroxyapatite (HA). Experiments have shown that to create such implants, it is advisable to synthesize hydroxyapatite with a given TCP content, rather than mixing the components mechanically.
Porous hydroxyapatite beads are becoming increasingly important in clinical practice. A material with such a structure “works” as a biofilter, providing the blood flow necessary for the growth of the resulting tissue structures.
Biological properties of hydroxyapatite.
Numerous experiments on animals have shown not only the excellent biocompatibility of hydroxyapatite, but also the ability, depending on the composition and method of production, to serve as a basis around which bone tissue is formed, while actively stimulating, unlike other bioinert materials, bone formation.
Experimental work has shown that the drug meets the standard of the GF-XI edition in terms of microbiological purity. It is a low-toxic substance and does not cause disruption of the functions of vital organs and systems of the body. The use of GA does not cause undesirable long-term consequences: it does not have an allergenic, mutational or immunomodulatory effect, does not affect the course of pregnancy, the development of the fetus and offspring.
The results of the analysis of hydroxyapol allow us to recommend it for medical use without any restrictions as a means for replacing bone defects and replacing bone cavities, as a component of dental filling pastes, implant materials
The increase in osseointegration is influenced not only by the structure, shape or coating of the implant, but also by the structural features of the patient’s body.
Example:
When examining patients before implantation surgery, specialists often have to note the presence of a thinned alveolar process. Such a narrowing of bone tissue can be a consequence of removal, the result of inflammatory diseases or trauma, as well as a congenital feature of the structure of the alveolar process and is detected in individual areas or along the entire length of the ridge during examination or during surgery. The proposed method allows you to simultaneously increase the volume of bone tissue and perform implantation surgery. The technique makes it possible to achieve through a longitudinal fracture of the jaw ridge like a “green twig”, resulting in the expansion of the alveolar process in the required areas and in a volume sufficient for the subsequent introduction of implants. The presence of several attachments makes it possible to expand the modeling of bone tissue to the desired amount and in the required location without compromising the integrity of the periosteum, which guarantees the subsequent “growth” of bone tissue. Trauma to the alveolar process of the jaw leads to an increase in blood flow, which contributes to the process of osteogenesis and, therefore, controlled growth of bone tissue and osseointegration of the implant.
The method was used in 63 patients; the results of long-term observations show its reliability, effectiveness and accuracy of results with accessibility and ease of implementation.
APPLICATION OF ENDOOSEAL IMPLANTS WITH BIOCERAMIC COATING.
Since bone is a porous object. It is considered necessary to note that in order to create the best conditions for osseointegration, it is very important to match not only the composition of the bone and the biocoating, but also the porous structure. In this regard, the predominant pore sizes of the compact substance of the human jaw in edentulous areas were determined alveolar process. The experimental data obtained were interpreted in the necessary way for the production of implants. By optimizing the technological conditions of the process of plasma spraying of hydroxyapatite onto the titanium base of implants, a bioceramic coating with a specific porous structure was created. It should be noted that by using composite structures with porosity similar to a compact substance, we not only achieve improved osseointegration processes over the entire area of contact with the bone, but first of all, we prevent the development of such complications as epithelial ingrowth and the formation of a bone pocket around the cervical part of the implant.
Among the variety of shapes, preference is given to smooth cylindrical implants, since they largely reproduce the configuration of the tooth root. In this case, the bioceramic coating represents a biotechnical model of the period.
CONCLUSION
The possibilities of modern science and medicine are inexhaustible.
Implantation operations are performed by surgical dentistry.
Since the use of implants is not only practical, but also aesthetic, they are increasingly used throughout the world. This abstract describes the conditions that most enhance osseointegration of implants.
BIBLIOGRAPHY
1. Modern problems of implantology: abstracts of reports of the 4th international conference May 25-27, 1998 - Saratov 1998.
Sukachev V.A.
Operations in dentistry. M., "Knowledge".
Intraosseous dental implants. Designs, technologies, production and application in clinical practice./V.N. Lyasnikov, L.A. Vereshchagina and others / ed. V.N. Lyasnikova, A.V. Lepilina – Saratov. Saratov University Publishing House 1997.
New concepts in technology, production and use of implants in dentistry: abstracts of the international conference June 15-18, 1993 Saratov 1993
Stages of the procedure
The implantation process occurs in stages. Sometimes it takes a long time to complete the procedure. The exact duration of the manipulation depends on the individual characteristics of the patient’s body and the complexity of the clinical situation.
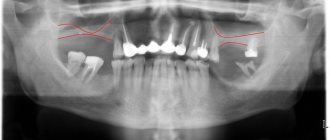
The first stage is planning. The doctor conducts a complete diagnosis. For this purpose, radiographic and computer studies are carried out. If necessary, dental treatment is performed.
The next stage is the surgical intervention itself. An artificial root is screwed into the bone. If necessary, the doctor can perform additional manipulations that will help eliminate degenerative processes in tissues.
The operation itself lasts from 30 minutes to several hours. It involves executing the following algorithm:
- administration of anesthesia;
- implantation of an artificial root;
- suturing the wound.
Sutures are removed 7-10 days after the intervention. In some cases, additional surgery is performed to install a healing abutment. After a few weeks, it will be removed and an abutment will be installed in its place.
The final stage of surgery is the installation of a crown, removable structure or bridge. As a result of all manipulations, the patient receives full-fledged teeth that perform their chewing functions and have an attractive appearance.
Bridge on implants
The engraftment period is important. Due to the good biocompatibility of titanium, osseointegration is about 96%. The result of the operation is assessed by the doctor using testing for root mobility. In this case, the patient should not experience pain.
Classic two-stage implantation
This protocol was the first to be developed and enjoys continued popularity. It is believed that two-stage implantation can be used in any case. It is possible to install both regular and short implant models. The implant is inserted into spongy bone layers, which are characterized by high porosity and a tendency to atrophy. An important condition for use is a full volume of bone tissue.
What is the essence of the method:
- preparatory measures are carried out - examination, identification of contraindications, the oral cavity is sanitized;
- An implant is implanted into the jaw bone using anesthesia in a few minutes;
- the implant is covered with gum tissue, sutures are applied;
- This is followed by the process of osseointegration - bone tissue fills all the uneven surfaces of the implant, increasing its stabilization.
- after osseointegration, the implant is opened and a gum former is installed, giving the tissues the correct shape;
- after 7-10 days, the former is removed, the abutment and permanent crown are installed.
Benefits of use:
- the implant performs the functions of a natural tooth root;
- the smile looks perfect and natural;
- the use of delayed loading allows the implant to completely fuse with the bone;
- successful engraftment occurs in 98% of cases;
- Some manufacturers provide a lifetime warranty on these products.
Complications and preventive measures
In some cases, postoperative complications may occur. These include canal perforation, suture failure, or implant fracture. If pain and inflammation occur, you should consult a specialist.
To prevent the development of complications, it is recommended to follow the following recommendations:
- during the first day after implantation, it is necessary to apply ice to the cheek every 3 hours;
- the oral cavity should be rinsed with antiseptic solutions;
- the gums should be treated with a special dental paste;
- The toothbrush should have soft bristles.
To avoid trauma to the mucous membrane, it is necessary to temporarily switch to soft foods. Medication support during dental implantation is mandatory. The doctor prescribes antihistamines, antibacterial and anti-inflammatory drugs.
Theoretical foundations of implantology
The foundation of implantology is modern ideas about the body’s reaction to the introduction of implants and an understanding of regeneration processes.
Tissue replacement and encapsulation of foreign materials, called organizing processes, are special cases of regenerative processes.
The final outcome of the organization processes is the resorption and replacement of the foreign substrate with connective tissue or its separation through the fibrous capsule from the surrounding tissues, as well as the formation of adhesions up to the overgrowing of the serous cavities.
In relation to a foreign body, the process of organization is expressed in the development of granulation tissue around it, encapsulation (formation of a capsule around the foreign body). In the immediate vicinity of foreign bodies, giant cells in the form of large protoplasmic bodies with numerous nuclei are sometimes formed from elements of granulation tissue. They surround foreign bodies, and in some cases capture and phagocytose them. These cells are commonly called foreign body giant cells.
The above patterns are typical for cases when a foreign body accidentally appears in the body, is completely located inside the tissues and does not communicate with the external environment.
Implant,
established according to certain rules, cannot be considered as a random foreign body, and the nature of its relationship in the implant-bone system, depending on the properties and structure of the material, can be histologically determined by three types of reactions (Table 20).
Table 20. Tissue reaction to the implant
| Pathological histological reaction | Foreign body reaction | Biocompatibility of the material | Materials (examples) |
| Remote osteogenesis (connective tissue intermediate layer) | Minor negative reaction | Biotolerant | Stainless steel, PMMA. Cr-Co-Mo alloys |
| Contact osteogenesis (bone contact) | No reaction | Bioinert | Titanium and its alloys, A12O3, carbon |
| Associated osteogenesis (ingrowth) | Positive reaction | Bioactive | Glass ceramics, CaPO, -ceramics, HAP-ceramics |
Contact osteogenesis was called osseointegration (osseointegration) by Brenemark. Remote osteogenesis is called fibrointegration.
Integrative processes are associated with reparative osteogenesis.
Schematically, reparative osteogenesis during the engraftment of dental implants can be presented as follows:
• trauma and damage to the integrity of the mucous membrane, periosteum, cortical and cancellous bone during the formation of the bone bed for the implant; • identification of two zones in bone tissue: - zone of reparative osteogenesis, - zone of bone tissue remodeling (zone where no intervention was performed); • bleeding from the intervention area, release of serum and cellular inflammatory mediators and other products of macrophage secretion; • formation by fibroblasts of an extracellular protein matrix (collagen, glycoprotein, elastin, proteoglycan, glycosaminoglycan); • formation of a phosphate film on the oxide layer of an implant made of titanium and its alloys (hydroxylapatite epitaxy processes are possible); • adhesion of proteoglycans, osteoblasts on the surface of the implant and its elements; cellular activity of osteoblasts; • final formation of the extracellular matrix with the formation of its inorganic components in the bone wound, as well as on the surface and internal structures of the implant; • formation of bone regenerate, closely related to the structure of the implant; • mineralization of bone regenerate and final formation of bone tissue directly associated with the implant (osseointegration of the implant); • remodeling of bone tissue (in the first zone with the participation of any implants, in the second zone with the participation of only mechanically active implants).
Of all types of bone tissue reactions, only osseointegration provides stability of the implant sufficient for its use as a support for orthopedic structures.
Despite the complexity of the structural connections of the surrounding tissues with the implant (foreign body), this connecting system remains only a biotechnical imitation of the natural connection of periodontal tissues with a natural tooth.
Until now, it has not been possible to solve the main problem of dental implantation - to create a system that reproduces the action of periodontal ligaments, which perform one of the most important functions during the act of chewing - shock absorption.
Prices
It is impossible to name the exact cost of an implant: it all depends on the number of artificial teeth, the chosen technology, the condition of the dental tissue and additional procedures that you will carry out in the future.
We use several technologies and will be able to offer you one that is suitable in terms of cost, quality, and service life. Be sure to make an appointment and the doctor will recommend the optimal type of implantation.
Our clinic employs qualified dentists and specialists with extensive experience in installing implants. We use high-quality materials and provide complete information about the procedure and rules for caring for teeth after surgery.
Clinical fundamentals of implantology
Contraindications and indications
When examining a patient, you should pay special attention to signs of diseases recognized by implantologists as absolute (general and local) or temporary contraindications to implantation.
General contraindications include:
• any reasons for refusing surgery; • any contraindications to local anesthesia; • diseases that may be adversely affected by implantation (for example, endocarditis, artificial heart valve or pacemaker, organ transplantation, rheumatic diseases, etc.); • forms of therapy that may adversely affect the healing and maintenance of the implant and its bed (eg, immunosuppressants, antidepressants, anticoagulants, cytostatics); • mental illness; • situations involving severe psychological or physical stress; • insufficient desire of the patient, as well as cachexia, old age, insufficient habit of general hygiene.
Age is not an absolute contraindication that excludes dental implantation.
There are also local contraindications:
• insufficient propensity for oral hygiene; • limitation of manual abilities, in particular motor activity; • pain syndrome in the maxillofacial area of unknown origin; • dysfunction of the temporomandibular joint that cannot be corrected, which can cause excessive load on the implant; • generalized marginal gingivitis that cannot be treated; • lobular fibromas, fibromas of the prosthetic edge; • insufficient presence of bone tissue, unsuitable bone structure, loss of more than a third of the alveolar tissue mass (for direct implantation); • unfavorable distance to the nervus alveolaris inferior, to the maxillary and nasal sinuses.
Temporary contraindications:
• acute diseases; • stages of rehabilitation and recovery; • pregnancy; • drug addiction; • condition after irradiation (for at least a year).
Impacted teeth, cysts, bone tumors and inflammatory processes in the area of the jaw bones are also contraindications for implantation.
The general condition of the patient’s body and a possible reaction to the implant can be determined through examination, as well as questioning the patient. If this data is insufficient, the patient should be referred for consultation to appropriate specialists. Undoubtedly, the opinion of a local therapist or family doctor about the patient’s health will be of great help.
Legal issues have now become particularly important when planning dental implantation.
Before starting the intervention (treatment), it is necessary to conclude and sign an agreement that provides for the possible consequences and actions of the parties. The patient should be familiarized in detail with the treatment plan, prognosis, possible complications, and warned about the likelihood of implant rejection.
In addition, the patient should be provided with objective information about possible alternative treatment methods.
The expected outcome of treatment should be discussed with the patient. When planning dental implantation and to predict its results, it is recommended to find out the functional qualities of previously manufactured prostheses.
The current level of dental implantology is, unfortunately, limited to a narrow range of indications for orthopedic treatment using implants.
The main prerequisite for the use of implant-supported dentures is the impossibility of using traditional prosthetic methods. This may be due to both objective factors (conditions for traditional prosthetics) and subjective ones (the patient’s categorical refusal of removable structures). In this regard, the desire of many patients to have fixed dentures instead of removable ones or to improve the fixation of removable dentures through implants very often does not coincide with the capabilities of the method.
Indications for the clinical use of dental implants are:
1) toothless jaws (especially the lower) with a high degree of atrophy of the alveolar part; 2) a single defect in the dentition with intact adjacent teeth; 3) the presence of a distally limited defect (Kennedy classes I and II); 4) the presence of a large distally limited defect (Kennedy class III); 5) the presence of a large defect in the frontal region (Kennedy class IV).
It should be noted that in all cases except 1, the use of implants can most often be associated with the psycho-emotional mood of patients, when they categorically refuse removable structures.
It must be remembered that the use of Brenemark-type implants, except for the 2nd case, still requires the manufacture before the operation of temporary removable structures that cover the defect in the dentition above the implantation site.
There are cases when patients agree to leave a well-made removable denture and refuse implantation. However, the patient’s refusal of a removable prosthesis and his desire to have a non-removable structure using implants should not be considered as some kind of whim or whim.
In each case, the doctor needs to deeply analyze the patient’s motivations, find out the reasons for refusing removable structures and carefully evaluate the possibility of using implants.
Patients who, for various reasons, have not been able to achieve satisfactory results from traditional prosthetics often experience a feeling of disappointment and hopelessness. In these cases, the use of implantation (in the absence of contraindications) may be the only way to get out of this situation.
This circumstance is associated with enormous interest in implantation of a certain part of patients and deep disappointment when, due to general or local contraindications, the use of implants is impossible.
Explaining contraindications to implantation in such patients must be carried out very thoughtfully, with strict adherence to deontological principles. It should definitely be emphasized that with the development of implantology, contraindications will narrow and removable structures should be considered as a stage that has important therapeutic and prophylactic significance.
Theoretically, any toothless area of the jaw can be restored with a dental implant.
To successfully install implants, the following basic requirements must be taken into account:
1. The width of the bone tissue in the bucco-lingual region is at least 6 mm. 2. The distance between the roots of adjacent teeth is at least 8 mm. 3. The thickness of the bone above the mandibular canal and below the maxillary sinus is 10 mm (or special surgical preparation is required). 4. For the manufacture of a superstructure supported on implants, the distance between the dental arches is 5 mm.
The minimal cortical thickness and low cancellous bone density of the bone bed compromise the success of implant osseointegration.
The volume and structure of the bone bed is determined by X-ray examination (panoramic, axial, targeted radiographs).
The final decision on dental implantation depends on the agreement of all parties involved: a detailed examination of the patient is recommended together with an implant surgeon to select the location and number of implants; When choosing an orthopedic design, it is desirable to involve a dental technician.
What treatment alternatives are there?
The simplest alternative to implants is dental prosthetics using tooth or gum support. The work involves installing both bridges and removable dentures. The disadvantage of this choice of treatment is the appearance of atrophy in the future.
- Bridge - connects artificial crowns and support on teeth that are ground down.
- Removable prosthesis. It is used to restore both part and all teeth. In case of complete absence of teeth, there is an attachment by suction on the gum.
How will such an implant take root?
Modern implantology systems allow you to be confident in the installed implant and not be afraid of material rejection. This does not happen often, in only 2 percent of cases, and is often a medical error or patient failure to comply with doctor’s instructions or improper postoperative care.
The engraftment itself is a long stage and lasts about six months. Doctors recommend at this time to relieve the work of the jaw and use a special design of a plastic prosthesis, which will not interfere with the formation of artificial roots.