2346
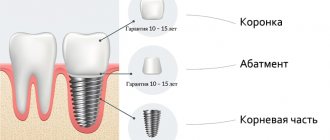
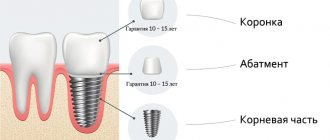
The most reliable, from a long-term perspective, method of restoring lost teeth today is dental implantation. Replacing the tooth root with a durable threaded metal rod maximizes the life of the crown.
This not only makes it possible to eat normally and improve the appearance of the dentition.
With the help of implantation, the patient has the opportunity not to worry about the timely replacement of prostheses and installed orthopedic structures. All together, this significantly improves the standard of living in general.
However, on the other hand, implantation is a serious surgical intervention . Therefore, even taking into account the high level of modern medical technologies, there remain risks of complications after implant installation.
These are the ones we will talk about today.
What is considered normal?
Many people believe that since operations are performed using anesthesia, pain and similar manifestations should not be present at all. However, this is not quite true. As already mentioned, even the simplest case of implant installation is a surgical intervention.
After the anesthesia wears off, most people experience very painful and unpleasant sensations. How long can they last, and is this considered normal?
Pain
This is a normal reaction of the nervous system to injury, which, in essence, is the screwing of the rod into the jaw bone. In almost all patients who have undergone such an operation, pain appears when the anesthetic drugs stop working .
Basically, this lasts about 2 – 3 days, but can last up to a week . Gradually, the pain should decrease and appear only with mechanical pressure on the area where the rod is installed.
If the sensations not only do not go away, but even intensify, this is a clear deviation from the norm. In this case, be sure to consult your doctor to avoid serious consequences.
Edema
Just like pain, swelling is an indispensable accompaniment of damage to soft tissue and bone.
Swelling appears in the installation site. Moreover, this process is almost never instantaneous. During the first 2-3 days it can only gradually increase. However, by the end of the first week after installation it usually goes away without a trace.
A complication would be an increase in the area of swelling and no improvement after the first week and a half.
Paresthesia and numbness
Numbness is a complete loss of sensation, and paresthesia is a state of tingling, tickling and incomplete sensitivity of soft tissues. Paresthesia is caused by prolonged resumption of blood supply to the soft tissues in the work area.
Typically, such phenomena occur immediately after the cessation of anesthesia. Mild numbness of the upper and lower lips, as well as partially of the tongue and surrounding soft tissues on the cheek . This often happens if the implant is placed near areas where nerves pass through.
With severe damage to the nerve bundles, numbness and paresthesia can be present for a very long time and cause partial immobility of the facial muscles. Such situations require medical intervention and appropriate therapy.
Bleeding
It is usually observed within several hours after surgery . This is completely normal, because in most cases it is necessary to cut the gum, so the blood vessels are damaged.
The benefit of such bleeding is that, along with the discharge, germs and pathogenic bacteria are washed out of the wound, which can provoke subsequent inflammation.
Usually it can last from one to five days, depending on individual blood clotting parameters. However, in cases where blood is released from the wound for more than a week, you should consult a specialist.
Additionally, some patients may experience local inflammation at the surgical site. This provokes a rise in body temperature to 37–38°C , sometimes more.
What is the characteristic of late peri-implantitis? What treatments are used?
In a separate publication, we will tell you how much it costs to install a dental implant and what factors influence the price.
Here https://www.vash-dentist.ru/implantatsiya/metodiki/odnomomentnaya.html we will look at what contraindications exist for one-stage dental implantation.
What to do if complications develop after dental implantation
The first thing the patient should do when the first symptoms of complications appear is to contact the doctor who performed the implantation procedure. You can take a painkiller yourself and rinse your mouth with antiseptic solutions. The principles of treatment of complications directly depend on their nature.
When inflammation develops, it is first necessary to identify and eliminate its cause, improve the patient’s oral hygiene, and prescribe appropriate medications, including antimicrobials. If the implant is fractured, it is replaced.
The most common pathologies
Seam divergence
Risks bleeding and infection of the entire area.
Can happen in several cases:
- First of all, this is mechanical damage or trauma to the sutured area.
- Also, wound infection may not be a consequence, but a cause of suture dehiscence.
The occurrence of such a complication requires immediate consultation with a doctor and constant monitoring , as it can lead to serious consequences, including loss of the implant.
Implant failure
It may manifest itself as spontaneous twisting and removal of the installed metal rod .
Causes:
- Most often this occurs due to significant weakening of bone tissue . In this case, they will need to be strengthened.
- In addition, a similar situation may arise due to an infectious process in the soft tissues surrounding the installation area , which can occur due to chronic diseases, smoking, mechanical or surgical trauma.
Repeated surgery is possible only 1–2 months after therapy.
The appearance of hematomas
This is associated with deep soft tissue injury and is caused by muscle hemorrhage. Gradually, the hematomas decrease in size and disappear completely.
It is recommended to undergo constant monitoring by the attending physician during this period , as well as the use of various ointments that help reduce the hematoma.
Photo: complication after dental implantation surgery in the lower jaw
Stages of nerve damage
Only a doctor can determine the extent of nerve damage.
- Neuropraxia. At this stage, the patient feels a slight numbness of the soft tissues in the operated area. Usually after some time the nerves regain their sensitivity
- Axonotmesis. Partial numbness, but more severe and accompanied by pain. It takes longer to restore normal functioning of the nerve than in the first stage (about a month)
- Neurotmesis. Significant damage to the nerve with the appearance of a scar at this location. It will take about two months to restore sensitivity.
After surgery on the upper jaw
Implanting upper teeth is much more difficult than lower teeth. This is explained by the structural features of the jaws and the difficulty of accessing the desired areas.
Also in close proximity to the implantation site on the upper jaw there are important organs.
The upper jaw is less dense. Because of this, specialists quite often choose longer implants for installation .
By increasing the length, a more durable installation can be achieved, which is required for safety and aesthetics. However, it is precisely because of this that complications most often begin:
- In the center, behind the incisors, there is a nasopalatine bundle, which can be easily damaged if the length of the rod is incorrectly selected or if there are violations during the operation. then a risk of bleeding and lack of integration of the implant into the bone .
- There is also the possibility of damage to the floor of the nasal cavities. In this case, you can get perforation of the internal nasal mucosa and, as a result, future infection in the apical (lowest point of the rod) part of the implant.
- In the canine area there are neurovascular bundles, if damaged, numbness or paresthesia of the upper lip .
- The area of the maxillary sinus is the most difficult for implantation. This is where the greatest number of complications arise. The volume of this zone can vary greatly, so it is quite easy to penetrate the bottom of the sinus. Then the presence of an implant can trigger the development of sinusitis .
- Prosthetics of the palato-pterygomaxillary mass is also fraught with complications. In particular, damage to the palatal artery and the occurrence of bleeding .
Patient selection
When selecting patients for treatment with immediate implantation, we are guided by the same criteria as for classical delayed implantation. At the same time, local selection criteria come first, namely:
- absence of acute inflammatory process in the area of proposed implantation.
- sufficient volume of bone tissue and mucous membrane (the latter is most important) in the area of the tooth to be removed
A consultation with an orthopedic dentist and, in some cases, an orthodontist is required.
Computed tomography and diagnostic models are required. In some cases, a surgical template may be required.
Consequences of unsuccessful interventions on the bottom row
Possible complications may also arise during implantation in the lower jaw.
There are dangerous areas around which all work, in particular drilling the initial hole and installing the implant, must be carried out with extreme caution in order to avoid negative consequences.
Loss of sensation
This is one of the most common complications when installing implants in the lower jaw. Of course, if we are not talking about the first hours after surgery, when numbness and loss of sensitivity are associated with the action of anesthetic drugs.
When the patient does not feel the area or the entire jaw after several hours, this already indicates a complication.
In any case, such a symptom indicates some kind of damage to the mandibular branch of the trigeminal nerve - its compression (compression) or rupture. Moreover, this was caused by a medical error.
What makes basal dental implantation different from other methods?
In this review, we will tell you which teeth can be fitted with a metal-ceramic crown.
Here https://www.vash-dentist.ru/implantatsiya/proizvoditeli/ankylos-dostoinstva-raznovidnosti-tsenyi.html you will find reviews from doctors and patients about Ankylosis implants.
Damage to the wall of the mandibular canal
Most often, complications associated with such injuries are not too acute.
Common manifestations are a feeling of numbness of the lower lip and adjacent soft tissues , as well as the entire lateral part of the lower jaw.
Damage to the external branch of the facial artery
A fairly rare occurrence, however, it can occur during surgery to install an implant in remote, hard-to-reach areas.
In this case, emergency care will be required by a regular surgeon .
Buccal perforation
This can lead to the threading of the implant being exposed.
This in itself is not a serious problem, since the situation is quite easy to correct. However, if you do not pay attention to this, you may subsequently lose the implant , which cannot be reinstalled without appropriate tissue regeneration and proper therapy.
In order to reduce all the consequences of dental implantation to a minimum, it is necessary, first of all, to fully comply with the technique and methodology that are determined by the treatment plan.
Much also depends on the patient himself.
How to avoid complications after implantation, watch the video:
Nerve damage during implantation: diagnosis, treatment, prevention
Damage to branches of the trigeminal nerve (eg, inferior alveolar, lingual, mental, or infraorbital) is a potential complication that can develop during the dental implant procedure.
Direct damage to the nerve fiber can be caused by injury, inflammation, or the result of an infectious factor. Most often, the branches of the trigeminal nerve are affected during anesthesia, flap separation, bone augmentation, osteotomy and direct installation of a titanium intraosseous support. Since the restoration of damaged nerve fibers is quite problematic, the best tactics for treating such complications is prevention. Therefore, it is extremely important for the doctor to understand the features of the histology and anatomy of the nerves of the maxillofacial region, and to be informed about the symptoms that most often accompany their lesions. Also, the clinician must take into account aspects of differential diagnosis in order to correctly establish the cause of the development of certain symptoms, based on which in the future he will have to carry out appropriate treatment. Treatment options for trigeminal nerve branch lesions include the use of various pharmacological agents, monitoring with physical therapy, or even removal of the problematic dental implant.
In this article we will discuss approaches to the treatment of dental patients with damage to the nerves of the maxillofacial area associated with the dental implantation procedure, as well as the main aspects of the etiology and pathogenesis of such pathologies in general.
Anatomy and histology of the trigeminal nerve
The trigeminal nerve is the fifth and largest pair of cranial nerves, which consists of the following branches: the ophthalmic nerve (V1), the maxillary nerve (V2), and the mandibular nerve (V3). The mandibular nerve is the largest branch and innervates the lower lip, chin area, teeth, adjacent soft tissues, lower jaw and part of the external ear. The motor fibers of the mandibular nerve are not damaged during the implantation procedure because they arise from the main branch of V3 before exiting the mental foramen. The main structural unit of a nerve is the nerve fiber. The structure of V3 is dominated by myelinated nerve fibers. Each axon and Schwann cell is covered in connective tissue called the endoneurium. Groups of nerve fibers form bundles that are surrounded by epineurium. Damage to any part of the nerve bundle can lead to neurosensory impairment. The trigeminal nerve consists of 7000-12000 axons, and the number of bundles varies in different parts of the maxillofacial region. The inferior alveolar nerve (IAN) is polyfascicular (consisting of more than 10 fascicles), while the lingual nerve contains only a few similar nerve structures. Since the NAN is characterized by a large number of nerve bundles, its regenerative abilities are also significantly higher compared to the lingual nerve.
Types of nerve lesions
Lesions of the trigeminal nerve can be caused by compression, stretching, complete or partial disruption of the integrity of the nerve fiber. Damage may result in neurosensory changes in touch, pressure, temperature, and pain. Such pathologies significantly affect the patient’s comfort and ability to talk, eat, kiss, shave, apply makeup, brush teeth and drink normally. In addition, neurosensory disorders also affect the patient's ability to interact normally in society. Signs of these pathologies can be identified directly during surgery (if there is a pain symptom), or during long-term monitoring of the patient’s condition. To describe traumatic lesions of axons of varying degrees of complexity, the following terms are used:
- neurapraxia - a lesion in which the integrity of the nerve fiber is preserved, and the mechanism of injury is associated with stretching or impact such as blunt trauma; Sensitivity usually returns to normal within a few days or weeks.
- axonotmesis - damage to the nerve, in which the processes of its degeneration and regeneration develop, but the axon itself does not lose its integrity, and sensitivity is normalized over 2-4 months; however, sensitivity after recovery may be slightly less than before the intervention, and in some clinical cases it is characterized by accompanying dysesthesia.
- neurotmesis - damage to the nerve, in which there is a violation of its integrity, and the prognosis for the restoration of normal sensitivity is unfavorable.
The International Association for the Study of Pain has standardized nomenclature regarding traumatic nerve injuries. In particular, the definition of the term paresthesia, which was previously used to refer to loss of sensation, was changed. Current terminology provides the following definitions:
- paresthesia - a change in sensitivity without accompanying discomfort;
- dysesthesia - a change in sensitivity, which is accompanied by unpleasant sensations;
- anesthesia - loss of sensitivity.
To describe changes in neurosensory functions, terms such as allodynia (the occurrence of pain to stimuli that normally do not provoke pain), causalgia (the presence of persistent burning pain), hypoesthesia (decreased sensitivity to the action of stimuli), hyperesthesia (increased sensitivity to action) are also used. irritants).
When nerves are stretched or compressed, the perineurium protects the bundles from damage. However, lengthening the nerve by more than 30% can provoke structural damage. When the integrity of the nerve is completely disrupted, symptoms of anesthesia and a decrease in certain sensory functions develop. When the integrity of the nerve fiber is partially disrupted, various symptoms of damage, including dysesthesia, may be observed. It should be noted that the presence of persistent pain after surgery is not a criterion for determining the potential for complete restoration of the function of the affected fiber.
After damage to the peripheral nerve, Wallerian degeneration begins to develop, which continues for several weeks and even months. Axonal necrosis develops distal to the site of traumatic intersection. Degeneration in such cases is progressive and irreversible and lasts for up to 18 months. The ability of the affected nerve area to heal is influenced by factors such as the patient's general health, age, and type of injury. A key point in the process of nerve recovery after damage is the formation of scar tissue in the area of endoneurial tubules.
Evaluation of traumatic lesions of the trigeminal nerve
NAN is most often affected during the installation of dental implants. Signs of inferior alveolar nerve involvement include anesthesia, paresthesia, or dysesthesia in the skin, lower lip, cheek, and gums up to the second molar site. Patients with damage to the lingual nerve are characterized by uncontrolled salivation, biting the tongue, a feeling of heartburn, loss of taste, changes in speech and swallowing function, numbness of the mucous membrane and tongue. Both during and after surgery, all potential symptoms of sensorineural impairment should be documented. Areas of altered sensitivity are mapped (both by location and area of the affected area). Thus, it is possible to monitor changes in all parameters in the future, and determine whether the patient needs microsurgical intervention or not. To identify and determine the extent of disorders, both objective and subjective diagnostic tests are used, which are conventionally divided into mechanoceptive (response to mechanical stimuli and compression) and nociceptive (sensation of pain).
Mechanoceptive tests include static touch with a soft brush, two-point discrimination, and determination of the direction of brush movement. The sensation of a needle prick and the recognition of thermal stimuli are classified as nociceptive diagnostic procedures. To compare indicators, not only the affected area is always diagnosed, but also a symmetrical area, thus accurately identifying the fact and degree of neurosensory impairment. If the patient complains of loss of taste, a cotton swab moistened with salt or sugar is used for diagnosis.
Prevalence of traumatic nerve injuries
After implantation, permanent loss of sensitivity in the lip area due to traumatic damage to nerve fibers is observed in 0-36% of clinical cases. However, these data can be considered somewhat outdated and do not correspond to the approaches of modern implantological practice. After all, earlier during operations, dental surgeons more often used vestibular incisions, which caused sensitivity disorders to develop. Today, during the installation of dental implants, midline mucosal incisions are made along the top of the residual ridge, and the entire procedure is pre-planned, taking into account the data obtained after a computed tomographic examination. Thus, it can be assumed that the prevalence of nerve fiber damage due to implantation is significantly less than 36%.
Dannan et al reported that the incidence of nerve damage with implantation was as high as 2.95% (5 of 169 patients treated) in cases of temporary neurosensory changes, and 1.7% in cases of irreversible implant-associated neuropathies. Another study found that the incidence of nerve damage after maxillofacial surgery was 2.69% (42 of 1559 patients), with an even lower percentage of irreversible neurosensory damage, but the exact number was not specified in the study. . In the author's opinion, however, even such rates of implant-associated damage to neural structures are too high for clinical practice. Transient loss of sensation in the lip can often be associated with swelling, which is observed during the first two weeks after surgery.
Traumatic damage to the lingual nerve during surgical procedures
The lingual nerve in the region of the mandibular molars passes through the soft tissues on the lingual side of the jaw. Sometimes the nerve is located coronal to the surface of the bone tissue and is tightly adjacent to the cortical bone plate on the lingual side. Therefore, any surgical interventions must be carried out very carefully in this area. After removal of the third molars of the mandible, lesions of the lingual nerve are observed in 0.5-2.1% of clinical cases. Traumatic disorders of the lingual nerve during dental implantation are not a common phenomenon and are recorded quite rarely. To prevent such complications when installing dental implants, the following rules should be followed: only intrasulcular incisions can be made without releasing incisions and flap separation from the lingual side; During flap separation, it is necessary to avoid overstretching it and maintain a safe distance when performing osteotomy. 90% of all recorded cases of neurosensory changes associated with lesions of the lingual nerve resolve within 8-10 weeks after surgery.
Preoperative planning: prevention of traumatic nerve injuries
To prevent most complications associated with the installation of dental implants, it is necessary to ensure careful planning of the surgical intervention. Using the capabilities of computed tomography and surgical templates allows you to avoid unexpected outcomes of iatrogenic intervention. When installing a dental implant, a minimum of 2 mm of bone thickness must be left between the apical part and the coronal part of the mandibular nerve canal. In addition, it is important to adhere to the specified osteotomy length and strictly follow the bone preparation protocol. The presence of 2 mm of bone thickness also avoids excessive bone compression in the area of the nerve after installation of a titanium intraosseous support (photos 1 - 2).
Photo 1. The implant was installed in the area of the 30th tooth. After the anesthesia wore off, the patient began to complain of parasthesia in the area of the right lip and chin. On an x-ray taken immediately after implantation, there are no signs of implant penetration into the mandibular nerve canal.
Photo 2. The implant was installed 10 years ago, and during this time the patient was able to adapt to changes in sensitivity. The CBCT image shows that the implant in the area of the 30th tooth is much closer to the nerve canal than previously thought.
If necessary, to ensure the safety of the intervention, short dental implants can be used. It is also important for the doctor to be familiar with the absolute length of all drills that are used during the manipulation, since failure to take these parameters into account can provoke excessive deepening by more than 0.4-1.5 mm relative to the selected safe boundary. To control the deepening into the bone tissue, it is also recommended to use special stoppers. However, the physician must understand that neither the thickness nor the density of the bone tissue over the area of the nerve ensures the safety of its condition during the osteotomy procedure, therefore applying too much force and pressure during the preparation of the bone tissue is strictly prohibited. Finally, it should be noted that up to 50% of lawsuits related to nerve damage after implantation are caused by the lack of informed consent on the part of the patient, which the doctor must obtain before surgery. It is also a good idea to assess the patient’s neurosensory parameters before the intervention in order to compare them with the data that will be obtained after implantation.
Local anesthesia: a potential cause of nerve damage
Traumatic lesions of the mandibular and lingual nerves can occur during anesthesia due to needle trauma, hematoma, and exposure to the components of the anesthetic solution. The mechanisms of such lesions are still quite unexplored. One retrospective study estimated the incidence of nerve injury during anesthesia to be between 1/26,762 and 1/160,5716 cases, while Haas and Lennon predicted the incidence of such complications to be 1/785,000. Other data suggest that the prevalence of short-term transient lesions of the mandibular and lingual nerves as a result of anesthesia ranges from 0.15% to 0.54%. Whereas cases of the development of permanent changes in sensitivity of the same etiology are quite rare, with a prevalence of 0.0001-0.01%. After performing mandibular anesthesia, 3-7% of patients experience electrical sensations that resolve spontaneously over time. However, when the clinician notes that the patient has overreacted to the needle insertion, the needle may need to be withdrawn and repositioned slightly. Methods for the treatment or prevention of nervous complications associated with the anesthesia procedure have not yet been developed. Between 70% and 89% of anesthesia-related neurosensory lesions develop in the region of the lingual nerve. This trend can be explained by the fact that the lingual nerve consists of only a few bundles, while the lower alveolar nerve consists of a huge number of them, which, in turn, increases its potential for regeneration. From a geometric point of view, everything is explained much more simply: the size of the needle is on average 0.45 mm, while the diameter of the lingual nerve is 1.86 mm, and the diameter of the inferior alveolar nerve is 3 mm.
Anesthesia-associated nephropathy most often develops after anesthesia with 4% solutions of articaine or pilocarpine. Compared to lidocaine, pilocarpine and articaine cause 7.3 and 3.6 times more neurosensory impairment. Garisto et al reported that in 4 of 9 studies, the complication rate was higher with prilocaine or articaine 4% solutions than with lower concentration anesthetic injections. According to the authors, local anesthesia with these drugs should be avoided in order to reduce the incidence of associated neuropathies after iatrogenic interventions. However, according to Malamed, the cases in which Arcticaine has demonstrated a greater association with neuropathies than lidocaine are anecdotal, and do not have sufficient evidence-based argumentation. Similarly, in 2013, after an extensive review of the literature, Toma and colleagues concluded that studies suggesting extreme neurotoxicity of articaine were retrospective in design, the data presented were at high risk of bias, and the findings should not be regarded as sufficient evidence. . The authors concluded that direct trauma to the nerve fiber is the predominant cause of neurosensory impairment, and the latter has little to do with the chemical toxicity of the anesthetics used. In general, there is disagreement in the literature on this issue; Therefore, clinicians should make decisions regarding the use of higher concentrations of anesthetics based on the conditions of each individual clinical case, while interpreting prior information and taking into account the recommendations of the drug manufacturers.
Osteotomy procedure for implantation
The osteotomy procedure should be performed using well-sharpened drills and abundant irrigation. Hypothetically, overheating of the intervention area during osteotomy can provoke traumatic nerve damage. The extent of bone necrosis caused by overheating is directly proportional to the preparation temperature under which iatrogenic intervention was performed.
Eriksson and Albrektsson summarized that performing an osteotomy at 47°C for 1 minute may provoke subsequent bone resorption. In cases of progressive resorption, given the shift in the position of the mental foramen, a transcrete incision is contraindicated; instead, it should be shifted to the lingual side. When placing implants anterior to the mental foramen, careful analysis of CT images should be performed, which may help detect the presence of a loop of mental nerve.
Flap separation procedures
As a rule, flap separation does not provoke any neurosensory disturbances, however, the doctor should still pay great attention when performing this iatrogenic intervention in the chin area. The doctor must clearly understand where the mental nerve exits the mental foramen, so that when separating the flap it does not cause damage to the nerve fiber.
Tooth extraction
Before extracting molars and premolars in the lower jaw for subsequent installation of dental implants, the relationship between the position of their roots relative to the course of the inferior alveolar and mental nerves should be carefully studied. Care should also be taken to curettage the sockets after resection, since periapical lesions may often be close to neural structures (Figures 3–4).
Photo 3. The patient sought help for pain in the area of the 31st tooth. The X-ray image shows signs of acute apical periodontitis.
Photo 4. The results of CBCT diagnostics indicate that the pathological focus is located near the nerve canal. The tooth was carefully removed, followed by careful curettage of the defect area.
Pharmacological therapy of neuropathies associated with the installation of dental implants
There is no clear opinion regarding which drugs are best to use in diagnosing traumatic lesions of the nerves of the maxillofacial area. Some authors prefer corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs). It is worth remembering that the use of various pharmacological agents is relevant only if the integrity of the nerve fiber as a whole is preserved. In cases of sensory impairment after injection, the patient can be given dexamethasone 4 g/ml directly to the area of the injury, and after 3 days the dose of steroids can be increased. If a nerve is compressed or a fiber is injured during surgery, 1-2 ml of dexamethasone is administered intravenously, after which dexamethasone is prescribed orally for 6 days (4 mg, 2 tablets after meals for three days, then 1 tablet after meals for another three days). If the integrity of the nerve is compromised, steroids may be prescribed for a period of 5 to 7 days. Impaired sensitivity can be relieved by 800 mg of ibuprofen, which should be taken three times a day for 3 weeks. If neuropathy develops after removal of the implant, patients can also be prescribed 800 mg of ibuprofen three times a day and with the same frequency 500 mg of amoxicillin for 5-7 days. In parallel, 50 g of prednisolone is prescribed, reducing the dose by 10 mg every day (for 5 days). Post-traumatic neuropathy can be treated with low doses of antidepressants and antiepileptic drugs.
In combination with a pharmaceutical approach, Renton and Yilma recommend physical therapy interventions for patients with chronic neuropathy. The goal of such a treatment algorithm is to reduce the patient’s discomfort and help him get rid of pain. Bagheri and Meyer generally question the effectiveness of corticosteroids in the treatment of traumatic lesions of the inferior alveolar nerve, since the density of the bone tissue forming the nerve canal is so high that it is simply impossible for medications to reach their space. At this time, there are no results from clinical studies that confirm the feasibility and success of using corticosteroids or NSAIDs for traumatic neuropathies associated with the installation of dental implants.
When to refer a patient to a microsurgeon
Universal recommendations regarding when to refer patients with traumatic trigeminal neuropathies to a microsurgeon have not yet been developed. Some authors argue that the patient should be referred to a specialist immediately after noticing sensory disturbances after the implantation procedure. Other researchers recommend referral to a microsurgeon after 2, 3, 4, or even 6 months of monitoring if signs of traumatic neuropathy are observed during these months. Ziccardi and Zuniga recommend microsurgical intervention for up to 1 year after the implantation procedure, since the effectiveness of microsurgical correction noticeably decreases one year after the intervention. When determining the fact of traumatic neuropathy after implantation, the physician must determine whether the patient needs to be referred to a microsurgeon, or whether the situation can be improved with the use of various pharmacological drugs.
Sometimes explantation, or slight “unscrewing” of the implant from the bone, can help resolve the symptoms of traumatic sensory dysfunction. The results of individual studies indicate that the advisability of referral to a microsurgeon is justified only by stating the fact of a complete violation of the integrity of the nerve. When the doctor is sure that he did not violate the integrity of the bone canal of the nerve, then the disturbance in sensitivity can be caused by compression of the nerve fiber or an inflammatory effect. In such cases, a pharmacological approach to treatment can also help. Meanwhile, the doctor must understand that even if he did not perforate the main nerve canal, the nerve often has additional branches, the course of which is quite difficult to predict. The latter is possible only with a careful analysis of the data obtained after CBCT scanning, because two-dimensional radiographs provoke superimposition of individual anatomical structures, therefore, the prediction of possible traumatic nerve damage with their help is ineffective (photo 1-2).
In cases of discomfort after implant installation, if it can be confirmed that the intraosseous support is not located near the nerve canal, treatment algorithms are variable. Bagheri and Meyer suggest monitoring for 3 to 4 months to see if sensory improvements are observed before referring the patient to a microsurgeon. The authors also claim that if the position of the implant is too close to the nerve, the level of compression of the latter can be reduced by a slight reverse movement of the implant. Other researchers suggest explanting the intraosseous construct within 36 hours and immediately prescribing steroids if the patient exhibits signs of neurosensory impairment after surgery.
Khawaja and Renton described four clinical cases of the development of sensory symptoms after the installation of dental implants, in which the intraosseous structure was not located near the nerve. However, upon explantation, the symptoms of neurosensory disorders resolved quite quickly in two of the four patients. Interestingly, positive dynamics were observed in patients whose implants were removed within 18 and 36 hours, and residual symptoms were observed in patients whose explantation was performed 3 and 4 days after surgery.
Renton, Dawood and colleagues suggest that patients with such symptoms should be monitored for no more than 3 months, since after this period the risk of developing neural changes outweighs the potential success of microsurgery. Ziccardi and Steinberg in their review article recommend initial monitoring for 1 month, and if symptoms improve, continue to monitor the patient. If the symptoms do not improve or worsen, it is necessary to refer the patient to a microsurgeon. Research results indicate that patients operated on for neurosensory impairment 6-8 months after implantation have the same level of success as patients operated on in a shorter period after iatrogenic intervention. According to the authors, earlier intervention is possible and more effective, but there is no evidence to support this assumption. In addition, microsurgery is not indicated in cases of only minor neurosensory changes, since the risk from the intervention itself in such cases exceeds the predicted success rate. There is also a 12-week waiting period - on average, this is the amount of time a doctor needs to decide whether to refer a patient for microsurgical surgery.
It is logical that in cases where patients have acute pain, it is not necessary to wait 12 weeks. Before arguing for certain approaches to treatment, the doctor must objectively compare X-ray data and clinical symptoms, and then take into account all possible medico-legal aspects of the violations.
Surgical restoration of damaged trigeminal nerve
There are specific reasons that justify the need for microsurgical restoration of the damaged trigeminal nerve, and contractual factors that determine the prognosis of this manipulation. Ziccardi and Zuniga formulated the following list of reasons that justify referral of a patient to a microsurgeon: sensory impairment that persists for more than 3 months and interferes with the patient’s normal life activities, confirmation of the fact of nerve transection, lack of improvement in signs of hypoesthesia, development of pain after implantation. After microsurgical correction is performed, a number of factors influence the success of it: the waiting time after implantation, the type and volume of the lesion, the degree of vascularization of the affected area, the experience of the surgeon, the method of harvesting and preparing the graft, the presence of tension in the repair area, the age and general health of the patient.
In fact, microsurgical restoration of the branches of the lingual and inferior alveolar nerves is possible. However, the success rate of such manipulations is very variable - on average, researchers indicate only 50-59.4% effectiveness of such treatment, and in only two studies the results of the intervention reached levels of 81.7% and 63.1%. In all the studies conducted, the number of subjects is quite small, so it is methodologically impossible to compare the final results of such studies. However, 50-60% of patients after microsurgical correction show signs of improvement in neurological impairment. Ziccardi and Zuniga warn that patients with severe sensorineural impairment should be informed that full rehabilitation is virtually impossible. Also, many researchers indicate that the effectiveness of microsurgical procedures in cases of treatment of anesthesia, dysesthesia and spontaneous pain is exaggerated. To summarize, microsurgical correction can help individual patients, but the level of predictability of the results of such treatment is ambiguous. Thus, the best treatment for neurosensory disorders associated with implantation is their prevention.
Conclusion
A common dilemma in clinical practice is: if an implant is successfully osseointegrated but causes mild paresthesia without pain, what should be done with it? After all, explantation may not always help resolve symptoms, and retention of the implant in the bone with actual nerve damage can trigger the development of neuroma. The latter is formed as a result of excessive healing of the area of the damaged nerve and hyperplasia of adjacent tissues, and very often requires subsequent surgical removal. The decision to choose a possible treatment method should be made together with the patient after a thorough discussion of all possible options, and before starting rehabilitation, the patient must formally confirm his consent by filling out a special written form.
Authors: Gary Greenstein, DDS, MS Joseph R. Carpentieri, DDS John Cavallaro, DDS
Reviews
Despite the apparent complexity of such operations in dentistry, negative consequences and serious complications are quite rare . This is facilitated by the use of the latest techniques for treatment and implantation itself.
You can share your feedback about such unpleasant consequences of dental restoration with implants by leaving a comment on the article.
If you find an error, please select a piece of text and press Ctrl+Enter.
Tags upper jaw implants implantation lower jaw dental operations complications
Did you like the article? stay tuned
Previous article
Dentistry: several centuries ago
Next article
What do you need to care for braces?
Clinical case #3
The above clinical situations are resolved relatively simply. We worked with single-rooted teeth under conditions of relative preservation of the volume of bone tissue and mucous membrane. However, this is not always the case.
Clinical situation: the upper sixth tooth was previously treated with the resorcinol-formalin method. An attempt to perform endodontic retreatment ended unsuccessfully:
The tooth must be removed. The situation is complicated by the low location of the bottom of the maxillary sinus.
Together with the patient, a decision is made to combine tooth extraction, immediate implantation and sinus lift into one procedure.
The 16th tooth is removed. In parallel, the gum former is fixed onto the 15th tooth implant installed two months earlier:
The reference point for positioning the implant is the interradicular septum. Despite the fact that installing an implant in one of the alveoli would avoid sinus lifting, it is highly undesirable to do this, since such positioning will create a number of serious problems during prosthetics and further operation of the prosthetic structure
An additional lateral approach is used for sinus lift surgery. The subantral space is filled with Bioss xenograft mixed with autologous bone shavings in a 2:1 ratio. Also, this material is used to fill the sockets of the roots of the teeth, although there is no great need for this. A Friadent Xive implant with a diameter of 5.5 and a length of 11 mm is installed.
The implant holder is removed:
In this case, the primary stability of the implant is extremely low. Therefore, the decision was made to abandon the installation of a gum former.
The tooth socket is closed with a BioGide collagen membrane, which is fixed to the implant with a plug through a pre-made hole.
Unlike the previous case, the surgical wound is completely sutured. This is associated with certain technical difficulties, but is necessary because, as mentioned earlier, the stability of the implant is relatively low, and, moreover, the use of a collagen membrane and a xenograft, in order to avoid infection, requires hermetically suturing the wound.
The postoperative regimen and prescriptions do not differ from those for delayed implantation and sinus lifting.
After 10 weeks, you can begin to open the implant and install the gum former.
After resection of the mucous membrane covering the former, we refer the patient to an orthopedic dentist (Arthur Makarov) for the manufacture of temporary prosthetic structures.
This clinical case clearly shows that the low primary stability of the implant and the low location of the bottom of the maxillary sinus are not an obstacle to immediate implantation. However, it is necessary to carry out a number of additional procedures to avoid infection of the surgical area, namely: hermetically suturing the wound, refusing to immediately install a gum former, etc. In the postoperative period, special attention is paid to antibacterial therapy, it is advisable to prescribe vitamins C and D3 in therapeutic dosages.
Clinical case #4
What to do in the case when, in addition to the above factors, the tooth is the cause of an active inflammatory process? Even in this case, we can consider immediate implantation as an alternative to a delayed technique.
Clinical situation: the upper sixth tooth must be removed for orthopedic and therapeutic reasons. The case is complicated by the low location of the bottom of the maxillary sinus and the presence of a fistula with purulent discharge.
Since the inflammatory process in the area of this tooth is in a chronic stage and nothing bothers the patient, it was decided to carry out tooth extraction, sinus lifting and implant installation in one intervention.
The incision is made along the periodontal sulcus with a vertical release incision sufficient to perform a sinus lift using a lateral approach. Since there is a fistula opening on the mucous membrane, its detachment should be carried out as carefully as possible.
Previously, computed tomography determined that the fistulous tract originates from the medial buccal root of the 16th tooth. Therefore, when examining the surgical wound, we see destruction of the vestibular wall of the socket and, partially, a granuloma at the apex of the medial buccal root.
The tooth is removed. During the removal of a tooth and root granuloma, the vestibular bone wall of the socket is completely destroyed.
The sinus lifting stage is carried out. Using the Variosurge device, osteoplastic access to the subantral space is created. The mucous membrane of the maxillary sinus is lifted, and at the same time a hole for the implant is prepared.
A Friadent Xive 4.5×11 mm implant is installed, and a Bioss Collagen xenograft is placed in the subantral space.
Working in this sequence helps to better control the condition of the mucous membrane of the maxillary sinus and avoid perforations. In addition, it is possible to work with very small amounts of osteoplastic material in this way.
There is only one problem left to solve, namely the lack of an outer wall of the hole. For this purpose, you can use a fragment of the outer wall of the maxillary cavity, which remains after creating access to the subantral space. It is fixed in place of the vestibular wall of the socket using a screw.
In this clinical situation, we do not use any materials to fill the tooth socket. The installed implant has high primary stability, which makes this procedure unnecessary.
Sutures are placed on the mucous membrane.
In the right photo you can clearly see that there is empty space between the gum and the former. In this case, we are guided by the principle “it is better to under-tighten than over-tighten,” since excessive tension of the mucous membrane will lead not only to its thinning and atrophy, but also to bone loss. We expect the area to fill with a blood clot.
In the postoperative period, special attention is paid to antibacterial therapy - the dosage of the antibiotic is increased by one and a half times. The patient is also recommended to take keratoplasty vitamins - C, A, E, as well as vitamin D3.
Picture 2 days after surgery:
As can be seen in the figures above, the fistula opening on the vestibular side of the alveolar process has completely closed and epithelialized. The condition of the mucous membrane is normal. The implant is stable and painless upon percussion.
Already at 8 weeks we can state that the operation was successful: there are no patient complaints, the implant is stable, painless upon percussion, the condition of the mucous membrane in the area of the intervention is satisfactory. After 8 weeks we can begin temporary prosthetics.
This clinical case further expands the possibilities of immediate implantation. In fact, we performed four operations (tooth extraction, sinus lifting, osteoplasty, implantation) in one intervention, and we operated under conditions of an active inflammatory process. As a result, we have significantly reduced not only the treatment time, but also maintained acceptable volumes of hard and soft tissue in the implantation area.
conclusions
Immediate implantation has the same capabilities as delayed implantation, and, subject to the conditions of adequate stabilization of the implant, is completely compatible with operations such as sinus lifting or osteoplasty.
At the same time, by preserving the soft and hard tissues surrounding the tooth, immediate implantation can easily achieve a satisfactory clinical result. Also, this technique greatly facilitates the positioning of implants, with the exception of cases of removal and subsequent implantation of abnormally located teeth.
The timing of osseointegration of implants is quite comparable to the timing of tooth socket regeneration, therefore these processes occur simultaneously and in parallel. The period at which we begin prosthetics after tooth extraction and implant installation is, on average, 6-10 weeks, which makes immediate implantation very desirable for prosthetics of dentition defects in an aesthetically significant area.
The incidence of complications with immediate implantation does not exceed that with a delayed technique. This is due to the fact that the bulk of complications of implantation in general are associated with a deficiency of bone tissue and mucous membrane, and with the immediate implantation method this problem is absent in principle.
However, there are disadvantages:
- Not every brand of implant is suitable for installation in the socket of a newly extracted tooth. Preference should be given to screw implants with small, non-aggressive threads.
- The immediate implantation technique is very demanding on the technique and quality of tooth extraction. From this point of view, low-traumatic tooth extraction with preservation of all alveolar walls represents the most difficult task for a dental surgeon.
- Despite the fact that in my practice there were two successful cases of tooth extraction and immediate implantation during exacerbation of chronic periodontitis, I would not recommend using this technique in the area of acute inflammatory process.
- The roots of an extracted tooth are not always an accurate guide for selecting an implant of the required length and optimal diameter. Therefore, the immediate implantation technique does not replace the need for computed tomography (and, in some cases, the production of a surgical template) for diagnosis and planning of surgical intervention.
- the decision to install an implant is made only after the tooth is removed, after a visual and instrumental examination of the alveoli. Therefore, before the operation begins, it is impossible to guarantee the patient that immediate implantation will be carried out in his case - and this must be warned about.
- work in an initially infected tooth socket requires increased attention to the postoperative regimen and prescriptions. Vitamin therapy is also recommended.