.
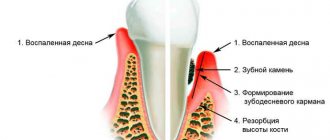
Periodontitis is a fairly common dental disease. It occurs in the form of an inflammatory process localized in periodontal tissues. The disease is accompanied by progressive destruction of bone and periodontal tissue, as well as the appearance of periodontal pockets. This is a fairly serious dental disease that manifests itself in different forms. Many of them are aggressive and lead to tooth loss.
Aggressive periodontitis requires a special approach to treatment. If any unusual symptoms appear in the oral cavity, you should immediately consult a doctor.
Aggressive periodonitis develops very quickly
Features of the disease
Aggressive forms develop due to increased proliferation of pathogenic microflora. Inflammations can be caused by certain groups of pathogens. The disease can develop in both adults and children. As a rule, in children, periodontal disease develops on one or two teeth, while in adults it is most often global.
Periodontitis, which is actively progressing, differs from the usual forms in certain features. The main ones include:
- generalized periodontal damage;
- feeling of weakness and malaise;
- weight loss;
- state of depression;
- deterioration of the protective functions of the immune system;
- extensive damage to bone tissue.
Aggressive periodontitis is a form of periodontitis in which there is a rapid and deep spread of inflammation in the bone tissue. It also creates deep pockets.
Aggressive form of periodontitis in a 22-year-old patient
As a rule, the disease reaches its peak very quickly. This can happen within a year. In other forms, periodontitis can last for ten years.
Due to the rapid progression of the disease, many experience early tooth loss. It is very important to start treatment on time. As is correct, such aggressive forms are not as common as marginal periodontitis.
T.N. Modina, S.S. Molkova, N.A. Kopylova, E.G. Starikova, M.V. Bolbat, I.R. Ganja Today, the development model of rapidly progressive periodontitis (RPP) is an integral mechanism of interaction between an etiotropic factor, the pathogenesis of development and clinical manifestations. Therefore, BPP is of great interest not only among scientists, but also clinicians, who must take into account the characteristics of the clinical manifestations and course of this pathological process. The treatment strategy for STDs includes selection of pathogenetically based diagnostic tests, selection of appropriate individual stages of treatment, including antibacterial therapy, splinting, surgical treatment using osteoplastic materials, orthodontic and orthopedic stages of treatment, supportive therapy. At the stage of surgical treatment, augmentation of the alveolar process is an important component in preserving teeth. Therefore, it is very important to choose the right osteoplastic material, which can not only fill the bone defect, but also induce integration processes in the bone tissue. Complex treatment and implantation of various plastic materials into bone pockets are the most effective; they help preserve teeth, which are usually removed with the traditional approach, and increase the remission stage. The main purpose of using osteoplastic materials is to fill a bone defect so that the bone adheres to the outer surface of the implanted material, infiltrates the intercellular space through pores, or causes biodegradation before the onset of osteogenesis. The most common outcome of surgical treatment of periodontitis using synthetic bone substitutes is the formation of the internal epithelial lining of the periodontal pocket to its entire depth. The volume of bone structures restored to one degree or another under the influence of modern osteoplastic materials is delimited from the surface of the tooth root by a layer of newly formed non-keratinizing epithelium. This outcome is interpreted as reparative. Among dentists, the domestic biocomposite material “KollapAn” is very popular. The biocomposite developed in the early 90s for disaster surgery has been successfully used in dental practice for more than 10 years. Microbiological and pathohistological studies carried out at the CITO named after. Priorov, showed that the drug has pronounced osteoprotective and antimicrobial properties, actively stimulates the processes of reparative regeneration of damaged tissues, promotes the restoration of bone structure, and is replaced by bone tissue without the formation of a fibrous layer. In the bone cavity, the valve gradually dissolves, being replaced by newly formed bone tissue, while the antibiotic contained in the composition is uniformly released over 20-50 days. Collapan-gel promotes angiogenesis, migration and attachment to the surface of bone marrow stromal and stem cells, their differentiation into osteoblasts and subsequent reparative osteogenesis. Mineralization of the osteoid matrix apparently occurs both by recipitation of calcium and phosphorus released from the implanted material, and due to the functional activity of osteoblasts. This material has proven itself well in bone oncology, in the treatment of open and gunshot fractures, and in the treatment of chronic osteomyelitis. This biocomposite, introduced into the bone pocket, retains its antibacterial activity for 20 days; its use in the treatment of periodontitis (especially early and rapidly progressing forms) helps reduce mobility and preserve teeth, increasing the period of remission. This bioactive material makes it possible to obtain good results from the surgical treatment of periodontal diseases and to monitor the dynamics of reparative osteogenesis. Taking into account the experience of working with the biocomposite material kollapan in other areas of medicine and its properties, we have used this biocomposite to close bone defects of the alveolar bone during surgical interventions since 1994. As an example of the positive results of complex treatment, we present two clinical cases. In recent years, the introduction of new technologies has allowed us to apply the method of tissue engineering (TI) - the use of artificial biocomposites in combination with bioactive molecules (bone morphogenetic proteins, growth factors, etc.) capable of inducing osteogenesis to close bone defects. The TI method can be used to close the sockets of extracted teeth, hemisection, amputation of roots, bone cavities with radicular cysts of various sizes, and during flap surgery. In practice, the combination of cerasorb and kollapan with platelet-rich plasma (PRP) and fibrin membrane (FMM), obtained by double centrifugation from the patient’s blood, has been widely used. As an example, a case of closure of a bone defect resulting from a split in the root of the 24th tooth under a metal-ceramic crown, in which an anchor pin was used during endodontic treatment, is given. Thus, ten years of work experience has shown excellent positive long-term results of using the kolvalpan not only independently, but also in combination with bioactive materials in periodontics, implantology, and maxillofacial surgery, where the interdisciplinary approach used in TI is aimed primarily at creating new biocomposite materials for restoration of lost functions of individual tissues and organs as a whole.Clinical case No. 1
Il. 2. Surgical stage of treatment
Patient P., 48 years old, came to the clinic with complaints of periodic swelling of the gums, bleeding, bad breath, and discomfort when eating (ill. 1). Three years ago, the patient underwent orthopedic treatment using metal-ceramic bridges on the upper and lower jaws. According to the patient, no X-ray examination was performed on the patient during treatment; a sharp deterioration in the condition of periodontal tissues was noted after prosthetics. An objective examination reveals a loose fit of the marginal part of the crowns, underbite on the lateral parts, and mobility of individual teeth. Periodontal pockets larger than 6 mm are noted, and purulent discharge occurs when pressure is applied. The radiograph shows pronounced destruction of bone tissue (Fig. 7a). Diagnosis: rapidly progressive periodontitis, severe form. The Fuchs bone index before treatment was 0.47.
Il. 3. Small vestibule of the oral cavity and a small area of attached gums
The patient was offered a complex of treatment measures, including professional hygiene, antibacterial therapy, surgical treatment using a collapan, and orthopedic treatment. At the stage of surgical intervention, flap surgery was used on the upper and lower jaws, vestibuloplasty according to Edlan (Fig. 2, 4). At the stage of orthopedic treatment, metal-ceramic bridges were made to splint the teeth along the arch, with cast inlays for fixation on the second molars of the upper and lower jaws on the left (Fig. 5). After the complex of treatment measures, the condition of the periodontal tissues remained stable, no exacerbations were noted for five years.
Il. 4. Vestibuloplasty according to Edlan The patient underwent professional hygiene twice a year as a rehabilitation and preventive measure, and according to indications, a vector system was used when treating the marginal gums (Fig. 6). After a year, the CP, according to the orthopantomogram, was 0.67, and after five years - 0.76 (Fig. 7c).
Il. 5. To strengthen the distal support of the metal-ceramic structure and splint the 28th and 38th teeth, cast inlays Il were used. 6. Application of the vector system at the stages of maintenance treatment
Clinical case No. 2
Patient M., 48 years old, came to the clinic with swelling in the area of the 24th tooth. The patient had pain in the root projection area, slight mobility of the bridge from the 24th to the 27th tooth, and a periodontal pocket of 8 mm. The radiograph showed arcuate bone destruction, root splitting, and a central anchor pin. Diagnosis: exacerbation of chronic periodontitis, fracture of the root of the 24th tooth. (ill. 8). After removing the crown under infiltration anesthesia, the mucoperiosteal flap was detached and root fragments were removed (Fig. 9). Using the method of double centrifugation, PRP and PPP were prepared from the patient’s blood (Fig. 10-12). The collapan was soaked in blood and connected to PRP, and then inserted into the bone defect (Fig. 13, 14). The top is covered with a fibrin membrane, and then the wound is sutured with a mucoperiosteal flap (Fig. 15). The sutures were removed on the 5th day. The condition is satisfactory, there are no complaints (Fig. 16). After six months, the defect was completely eliminated (Fig. 17). Il. 7. The condition of the oral cavity in patient P. five years after complex treatment Il. 8. Patient M., 48 years old. Periostitis of the upper jaw in the area of the 25th tooth, complicated by vertical root fracture with an anchor pin Ill. 9. Removal of the root of the 25th tooth and revision of the socket. The compact vestibular lamina is completely resorbed.
Related materials
- Tissue engineering in the complex treatment of patients with rapidly progressing periodontitis
- Minimally invasive therapy with the Vector system and its role in the complex treatment of periodontal diseases
| Next > |
Classification
Aggressive forms of the disease are presented in several types.
- Adult periodontitis. This is a chronic form of the disease that occurs after the age of 35 years. The course of the disease is slow. Its cause is the activity of gram-negative bacteria; bone tissue with this pathology is affected both horizontally and vertically. This form is the most common.
- Prepubertal. Occurs quite rarely. As a rule, it develops in the period after the eruption of molars. Pathology can manifest itself in two forms. The first occurs locally and affects only individual teeth, and the second is generalized - the entire dentition.
- Juvenile. Most often, this form occurs in girls during puberty. As a rule, molars and incisors are affected. Bone tissue is destroyed without severe symptoms. The presence of plaque is insignificant. According to experts, this disease is hereditary. Sometimes the development of the disorder is caused by nonspecific anaerobic bacteria from the gram-negative group. The disease is highly treatable with antibiotics.
- Rapidly progressive. Typically diagnosed in patients under 35 years of age. There is destruction of the alveolar bone and a small amount of plaque. The disease often appears in people who have diabetes and Down syndrome. There are two types of rapidly progressive periodontitis. The first is type A, which manifests itself at the age of 14-26 years. Type B is diagnosed in patients aged 26-35 years. Even after careful treatment, periods of exacerbation are observed. Rapidly progressive periodontitis is one of the most complex forms.
- Ulcerative-necrotizing gingivo-periodontitis. As dental practice shows, this form of the disease develops as a result of untreated necrotizing ulcerative gingivitis. There is increased damage to periodontal tissue and the appearance of cavities between the gums and teeth.
- Refractory. A feature of the pathology is a continuous process of relapses. Even after careful treatment, periodontitis returns and causes destruction of bone tissue.
The classification also includes periodontitis, which is associated with diseases of a systemic nature. It develops against the background of existing pathologies.
Juvenile form of aggressive periodontitis
Classification of periodontitis
With the flow:
- acute
- chronic
- aggravated (abscess)
- remission
According to the prevalence of the process:
- localized (focal)
- generalized (diffuse)
By severity:
- easy
- medium degree
- heavy
Characteristics of periodontitis of varying severity
Mild Periodontitis of the first mild severity is characterized by a loss of alveolar bone to 1/3 of the height of the tooth root, the bottom of the periodontal pocket during examination is reached at a depth of up to 3.5 mm, while the teeth are motionless. Moderate The second degree - moderately severe is characterized by the presence of a periodontal pocket, the depth of which reaches 5 mm, and the loss of alveolar bone is 1/2 of the height of the root, while pathological mobility of teeth of 1-2 degrees is observed. Severe The third degree is severe, characterized by a depth of periodontal pockets of more than 5 mm, with a concomitant loss of alveolar bone by more than 1/2 of the height of the root, while 3-4 degrees of tooth mobility are revealed.
Degrees of tooth mobility
- The 1st degree of mobility is diagnosed when the ability of a tooth to move, in relation to the neighboring one, in the palatal - buccal-lingual, vestibulo-oral directions, by no more than 1 mm.
- The 2nd degree is determined by pathological mobility of more than 1 mm in the same directions, with the addition of mobility in the palatal-distal direction.
- The 3rd degree is considered to be mobility of the tooth in all directions, including vertical; in the absence of adjacent teeth, it may be tilted.
- The 4th degree is pathological mobility of the tooth, in which it can make forced movements even around its axis.
Degrees of tooth mobility
Marginal periodontitis
A fairly common form of the disease is marginal periodontitis. It is presented in the form of an inflammatory process, which is localized in the ligament of the tooth near the dental edge. Marginal periodontitis can be caused by trauma to the edge of the periodontium: when something sharp gets stuck between the tooth and the gum. And also reasons include:
- injury due to impact;
- improper filling and prosthetics;
- constant accumulation of food between teeth;
- regular trauma to the peridontal edge with dental floss.
Marginal periodontitis is accompanied by painful sensations at the edges of the gums and its redness. As a rule, it is diagnosed when patients present with the listed complaints.
Marginal periodontitis occurs in the form of relapses, followed by periods of subsidence. Increased periodontal destruction is observed.
Aggressive forms are very serious and require careful treatment. If you neglect treatment, tooth loss is inevitable.
Aggressive periodontitis can be asymptomatic and patients often present too late with an already developed disease. Therefore, you need to constantly consult a doctor and monitor the condition of your teeth.
Generalized periodontitis on x-ray
Types of periodontitis
Periodontitis often occurs after untreated gingivitis. The infection reaches deep tissues and invades the adjacent tooth. May spread further, affecting the bone and most of the mouth. The following types of periodontitis are distinguished:
Treatment
Aggressive periodontitis takes a long time to treat. Antibiotics are often used, since most forms of pathology are caused by the activity of pathogenic microflora. The first stage of treatment begins with the following actions:
- teeth cleaning;
- plaque removal;
- removal of dental stones;
- root polishing.
Closed curettage is performed over two days. During this time, the root is polished or removed. An ultrasonic device is used for this. The need for the procedure is as follows: cleaning the gum pockets and reducing the amount of pathogenic microflora.
After the first stage of treatment is completed, patients get rid of the burning sensation and increased bleeding of the gums. Teeth become stronger.
Closed curettage removes gum pockets
After such a procedure, the sensitivity of teeth to cold may increase. This is due to the fact that along with the plaque, part of the tooth enamel is also removed. After 1-2 weeks, this symptom goes away. To reduce sensitivity, you can use special pastes. And there is also exposure of the roots, which is associated with deep pockets in the gums.
Focal
In the classification of periodontitis, a focal or local disease is distinguished. The main difference is the acute course of the disease. Symptoms of this type of periodontitis are:
As the focus of inflammation increases, the pain when chewing increases. Children are susceptible to this type of disease when they change teeth. During adolescence, this type of periodontitis develops into a chronic form. Timely treatment allows you to avoid progression of the disease.
Alternative method
One treatment option is splinting. It is used in cases where the teeth have already become mobile. Using a special design, teeth are secured. It can be either permanent or temporary. Aggressive periodontitis requires long-term therapy.
After six months have passed, the second stage of therapy begins. During this time, when the disease is not advanced, small periodontal canals are eliminated, and large ones become smaller.
In cases where the depth of the pockets is within 5 mm, surgical intervention is required, since other methods are no longer relevant. During surgery, final cleaning of the enamel is performed. Plaque and tartar are removed. Replacement of tooth tissue destroyed as a result of the inflammatory process.
How does it end?
The third stage of treatment is supportive in nature. At this point, it is necessary to provide conditions under which pathogens cannot cause an inflammatory process and thereby contribute to the re-development of the disease. It is necessary to avoid relapses, since the disease will be much more difficult, as will the treatment process.
Splinting teeth - the final stage of treatment
At the final stage of therapy, it is recommended to adhere to the following preventive measures:
- visit the dentist and carry out preventive treatment;
- brush your teeth every day;
- improve oral immunity, which will avoid the proliferation of bacteria;
- carry out professional teeth cleaning in dentistry.
If all recommendations are followed, as well as timely consultation with a doctor, the disease can be treated and it is possible to save teeth without further loss.
Treatment methods
With periodontitis, the risk of losing a tooth or an entire row of teeth is high. It is important to detect and treat the disease in time. High-quality cleaning of gum pockets at home is impossible, so this hygiene step should be entrusted to a doctor. Conservative or surgical treatment can be supplemented with folk remedies. The goal of any method is to destroy the infection and restore tissue.
Complex therapy
The treatment regimen includes professional hygiene, the use of local and general medications, and physical therapy.
In dental clinics, the oral cavity is sanitized: tartar and deposits are removed, periodontal pockets are cleaned, and the cause of the disease is identified and eliminated. During sanitation, antiseptic agents are used: iodinol, chlorhexidine, furacillin, peroxide, which effectively clean and disinfect inflamed tissues.
To stop inflammatory processes and destroy pathogenic microflora, gel applications are made or medications are injected into the periodontal pocket. Hypertonic drugs help relieve swelling and inflammation, eliminate bacteria and their waste products - antibiotics and adsorbents. Enzyme preparations are used to normalize oxidative processes and break down necrotic tissue. To increase local immunity, immunostimulants are used.
In case of severe inflammation, it is advisable to use systemic drugs: antibiotics, histamines, immunomodulators, vitamin complexes, which include vitamins C, group B, E, K, PP. If the patient experiences anxiety or irritability, sedatives are used. The duration of the course of medication is determined by the doctor.
The treatment complex includes physiotherapy: phototherapy, ultrasound, UHF, aerosol therapy, electrophoresis, laser treatment and other procedures. Physiotherapeutic methods are aimed at normalizing metabolic processes, blood circulation, lymph circulation, eliminating inflammation, strengthening and restoring periodontal disease. The number of sessions depends on the severity of the problem.
To support basic therapy, you can rinse your mouth with herbal infusions: pine rinse, oak bark decoction, tincture of marsh calamus, lingonberry leaves.
Orthopedic treatment
It is used when a tooth is missing or it is impossible to save it (after preliminary removal). Dentures are necessary to prevent malocclusion, which can provoke further development of the disease. Medical procedures are performed by an orthopedic dentist.
Basal implantation shows high efficiency. The implants are easily placed in the deep part of the jawbone and have a smooth antimicrobial layer. Plaque does not accumulate on them, and the inflamed tissues are restored over time and the person recovers.
Surgery
Surgical intervention is required in advanced cases, if the problem cannot be eliminated by conservative methods. The surgeon performs flap operations, splinting teeth, and open curettage.
During flap operations, periodontal pockets and tartar are eliminated, the gum edge is corrected, and the volume of bone tissue is replenished (bone grafting). Splinting is done to fix a moving tooth in the correct position. Open curettage allows you to efficiently clean gum pockets more than 5 millimeters deep.
What other treatment options are there?
Treatment of aggressive forms of periodontitis must be comprehensive. It is necessary not only to eliminate the symptoms, but also to provide a set of measures that will be aimed at overall strengthening the body in order to speed up recovery. Orthodontic treatment may be performed. It will help resolve the following problems:
- deep caries, as well as its complications;
- incorrect position of teeth and their absence;
- deformed bite.
After solving these problems, the treatment process becomes much more effective. In cases where pathology has led to tooth loss, prosthetics are required. It provides for the following actions:
- treatment of gums in areas of tooth loss;
- production of dentures;
- installation of prostheses.
Dentures are a good option
Prosthetics is a long process. Dentures allow you to evenly distribute the load on the teeth and ensure chewing function. They provide an aesthetic effect. After complete elimination of the inflammatory process, permanent prosthetics are performed. Initially, temporary, removable dentures can be used. Prosthetics are possible only under the following conditions:
- absence of tartar and plaque;
- complete elimination of inflammation;
- compliance with the rules of oral hygiene;
- the depth of the gingival pockets should be no more than 4 mm;
- the presence of dense gums around the tooth;
- completely cured caries;
- correct bite.
If the teeth are very mobile, elements are used that will fix them. When the load on the prosthesis is increased, implants can be used to act as a support.
Before installing implants, the inflammation must be completely cured. A thorough examination is performed to exclude the presence of contraindications. Additionally, chronic diseases are treated.
Teeth implantation is performed when teeth are lost
Typically, implants are used in cases where there is a poor prognosis. If there is a risk of losing a tooth, it is removed, but the bone tissue that is located around it is preserved.
When installing an implant, the volume of bone tissue may increase, which often decreases in aggressive forms of periodontitis.
Is it possible to do implantation and do I need to remove my teeth?
Inflammation at the initial stage, as a rule, does not lead to tooth loss - if this happens, then the reason lies in other problems (for example, pulpitis or periodontitis, wearing bridges that led to the destruction of supporting teeth). Therefore, implantation may be required to restore single elements or small segments. And the issue of preserving your teeth (and there are probably many of them left) is actually very pressing.
With this form of the disease, implantation can be carried out - the prognosis is quite favorable, including in cases of partial edentia, that is, if you need to restore only a few teeth (for example, chewing ones), while preserving the remaining ones. But only if you undergo comprehensive treatment for a year according to the chosen program - after this time, the doctor will assess the condition of the periodontal tissues, and you will be able to develop a strong habit of careful and high-quality oral care. In the future, this will allow you to maintain the results of both periodontal and implantological treatment.
Recommendations
What the prognosis will be depends on what form of the disease the patient has and at what stage of its development he turned to a specialist. In advanced forms of periodontitis, prosthetics or implantation are required, since it is no longer possible to save your teeth.
Aggressive forms of periodontitis develop very quickly, so you need to see a dentist as soon as possible. The danger of the disease is that it negatively affects the entire body. The pathology can be completely cured only if special recommendations are followed.
- Strict adherence to all dentist instructions.
- Carrying out a full course of therapy. You cannot stop treatment, as the disease will continue to progress, leading to various complications.
- Proper oral hygiene.
- Regular visits to the doctor and consultation on treatment.
Aggressive forms of periodontitis, despite their frightening name, can still be treated. It is very important that when the first symptoms appear, you need to consult a dentist and undergo treatment.
Acute periodontitis
The acute type of periodontitis is divided into 3 stages:
- Bleeding gums, itching, and irritation appear. There may be some pain from the cold. There are no visible changes at this stage.
- Bleeding occurs when brushing teeth and eating solid foods. A gingival pocket appears. Teeth become mobile. There is pain when biting. The person experiences discomfort. At this stage, patients most often turn to dentists for help.
- The bone tissue is partially destroyed. The gums become loose. Teeth become loose when chewing. If left untreated, the disease at this stage leads to tooth loss.
The cause of acute periodontitis is inflammation. Occurs as a result of mechanical, less often thermal damage. Active interaction between pathogenic flora and decreased immunity leads to inflammation. Vascular permeability increases, blood supply decreases, and tissue structure is destroyed.
Provoking factors for the development of acute illness are:
Causes of periodontitis
Neglect of the teeth and oral cavity leads to the formation of plaque, which consists of waste products of bacteria. After brushing your teeth, the plaque disappears, however, after eating it appears again. According to statistics, 85% of the world's population is prone to periodontal disease. Carious lesions of teeth cause tooth loss five times less often than periodontal pathology.
At the beginning of the disease, slight redness and irritation of the gum tissue (gingivitis) appears; the mucous membrane can sometimes bleed when brushing. Then the gum tissue thickens and rises above the crown, forming “pockets” - voids between the tooth and the gum tissue. Food debris accumulates in pockets and bacteria multiply. The pathology process is getting worse.
Important! A feature of the initial development of periodontal pathology is the absence of pain or other unpleasant sensations. Only regular check-ups with a dentist can reveal the initial process of the disease.
At the stage of gingivitis, you can stop the spread of infection into the deep gum tissue and prevent tooth loss.
Other causes of pathological gum disease include:
- smoking, chewing tobacco - nicotine tends to weaken the human immune system, which negatively affects periodontal tissues;
- hereditary predisposition - even careful hygiene does not save you from the disease;
- the use of medications that reduce the formation of saliva, which leads to accelerated formation of plaque and tartar;
- the presence of some serious diseases that reduce immune defense;
- Poor nutrition, lacking sufficient calcium and vitamins B and C.
Concomitant factors in the development of pathology are bruxism and malocclusion. Sometimes periodontitis can develop after injury to a tooth due to impact (cracks, chips), as well as when aggressive acids or alkalis influence the tissues of teeth and gums. Unfortunately, the disease can also occur with incorrectly installed dentures or fillings.
Periodontal disease has two stages of development - chronic and acute. In the acute phase, the following signs are present - chronic periodontitis symptoms:
- throbbing pain in the gums;
- looseness and itching of gum tissue;
- unpleasant taste in the mouth;
- loosening and mobility of teeth;
- reaction of the neck of the teeth to hot/cold food;
- discomfort while chewing food.
Subsequently, there is swelling of the gum tissue, profuse bleeding when touched by a toothbrush, and increased pain. In some cases, the acute form of the pathology leads to an increase in temperature and a feeling of loss of strength.
Also characteristic of the development of the acute form is:
- enlarged lymph nodes under the jaw;
- formation of fistulas and abscesses on the gums;
- the appearance of microbial allergies.
The acute form, in the absence of qualified therapy, becomes chronic, which is characterized by increased pain symptoms. In the chronic form of periodontitis, a change in the color of the gums occurs, the appearance of gaps between the teeth and the loss of individual (healthy) teeth.
The pockets increase in size, and the exposure of the tooth crown exceeds a height of 5 mm. Purulent inflammation of the pockets, decreased body tone, and the appearance of heart failure are often observed.
A decrease in the functionality of the process of chewing food leads to gastrointestinal disorders and diseases of the internal systems of the body.