Alveolitis is an inflammation of the socket (alveoli) left after tooth extraction. This pathology does not always develop; its development depends on many factors. The disease is characterized by severe pain in the area of the hole formed after surgery, general weakness, fever, headache, enlarged submandibular lymph nodes, bad breath and other unpleasant symptoms.
Alveolitis is not only physically painful, but also a dangerous disease. In the absence of proper treatment for several days, the inflammatory process can result in limited osteomyelitis, purulent melting of the jaw bone, and then surgical intervention will be required again.
With timely diagnosis of pathology and proper sanitation of the socket, the treatment prognosis is favorable. The main thing is to detect the symptoms of the disease in time and begin to treat it.
Classification
Depending on the nature of the healing of the hole, dentists distinguish several main forms of dental alveolitis:
- Serous. The initial stage of the disease usually appears 2–3 days after tooth extraction. This form is characterized by continuous pain that worsens while eating. Although the patient does not yet complain of feeling unwell, his lymph nodes are not enlarged, but he already feels that the disease is progressing.
- Purulent. If the serous form of alveolitis is not treated, the disease turns into a purulent form. Most often it is diagnosed 6–7 days after tooth extraction. The painful sensations can no longer be ignored, the pain intensifies, radiating to the ear or temple. Exploring the affected area also causes severe pain. Purulent alveolitis is characterized by a dirty gray coating inside the socket, significant swelling around the wound, thickened alveolar process and other problems. The patient's general health deteriorates significantly. Lymph nodes enlarge and become painful on palpation. Often the patient cannot even eat or open his mouth.
- Hypertrophic. At this stage, the symptoms of the disease subside. The patient notes a decrease in body temperature, improved well-being and decreased pain. However, at the hypertrophic stage, dangerous tissue proliferation occurs, which is clearly visible upon examination. When touched, pus is released from the inflamed area, and the mucous membrane acquires a bluish tint.
Ask a Question
Causes of inflammation
The disease can develop only after tooth extraction. Most often, the hole formed after removal heals within a day after the operation, and the patient feels better. But if the blood clot that covers the open wound moves or becomes deformed, an infection can penetrate into the hole, in which case alveolitis of the gums develops. As a result, the surface of the wound heals for a long time, and the patient suffers from complex discomfort.
Predisposing factors for the development of inflammation:
- Surgical injuries during complex removal. The more complex the operation, the more pronounced the postoperative inflammation of the bone tissue will be, and the more likely the release of direct plasminogen activators.
- Complex extractions associated with tooth segmentation, osteotomy, detachment of the mucoperiosteal flap. Complex operations increase the chance of developing alveolitis 10 times.
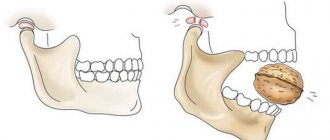
- Removal of wisdom teeth. The denser, less vascularized bone tissue adjacent to the figure eights is prone to the formation of dry sockets.
- General diseases of the patient. Alveolitis often occurs against the background of concomitant diseases. For example, patients with diabetes mellitus or immunocompromised patients are more susceptible to alveolitis due to impaired healing processes in the tissues.
- Taking oral contraceptives. The estrogen contained in these drugs may indirectly enhance the fibrinolytic process, causing the breakdown of the blood clot.
- Smoking. The direct connection between smoking and alveolitis has been repeatedly proven clinically. According to studies, the risk of socket inflammation in smokers increased 4-5 times compared to non-smokers. The incidence increased by more than 20% in patients who smoked 1 pack per day and by 40% in patients who smoked immediately before and after surgery.
- Dislocation of a bunch. If the socket is handled carelessly and there is negative pressure (for example, due to drinking through a straw), alveolitis may develop.
- Bacterial infections. Dentists agree that bacterial infections are the main risk factor for dry socket.
- Poor oral hygiene. The incidence of alveolitis increases significantly with poor oral hygiene.
- Excessive use of local anesthetics. According to some studies, excessive use of an anesthetic with a high concentration of a vasoconstrictor can provoke ischemia and make it difficult for the socket to fill with blood. This condition also increases the risk of alveolitis.
In fact, alveolitis is a fairly rare disease. According to statistics, it affects approximately 3% of patients who have undergone tooth extraction surgery. More often than not, the socket is not formed properly when lower incisors and molars are removed.
But alveolitis is especially common when removing lower wisdom teeth: according to experts, in approximately 20% of cases, the removal of “eights” with difficult eruption is complicated by alveolitis. In addition, it is believed that the risk of developing the disease is inextricably linked with age. This is explained by the fact that metabolism slows down, immunity is weakened, and the regenerative abilities of the body deteriorate.
Causes of alveolitis after tooth extraction
The extraction of teeth in itself is not a direct cause of the development of alveolitis. Factors that provoke inflammation of the tooth socket are complications that arose during surgery:
- Injury to the wall of the alveolus, in which the root was fixed before the tooth was removed.
- Penetration of infection into damaged jaw tissue.
- A dry socket after tooth extraction is the absence of a blood clot, which serves as a natural isolation of the resulting wound from pathogenic microorganisms.
- Tooth destruction during extraction.
- The presence of curved roots of the tooth being removed or growths on their surface.
- Root stuck in the gum after crown removal.
- Using additional removal methods: sawing, cutting.
Molars are large teeth with a large number of roots, so alveolitis appears more often after the removal of a wisdom tooth or adjacent molars than when pulling out incisors.
Alveolitis can develop due to an infectious disease of the tooth to be extracted or nearby gum tissue:
- Chronic inflammation in the gums.
- Presence of caries, periodontitis.
- An abundance of dental plaque with actively multiplying microbes.
Inflammation can be caused by improper actions of the dentist or patient: insufficient treatment of the instrument and wound, eating rough food after surgery, and poor hygiene. The patient's weak immunity increases the risk of developing inflammation.
Symptoms of alveolitis
As a rule, the patient ignores the first symptoms of inflammation without due attention, considering them to be the norm after surgery. After tooth extraction, as already noted, pain within 24 hours is considered normal. As the hole heals, the pain subsides and completely disappears after a few days.
If the patient develops an inflammatory process, then the unpleasant sensations do not subside after a day or two, and 3–5 days after the operation, severe, throbbing pain in the socket occurs, which intensifies as the infection develops.
With alveolitis, patients may complain of both unbearable and moderate pain. Pulsation and pain are focused, as a rule, only in the removal area. However, in rare cases, the pain radiates to half of the face.
Other characteristic symptoms of alveolitis are:
- a sharp rise in body temperature;
- tooth sensitivity to hot/cold food;
- enlargement of the submandibular lymph nodes;
- decreased appetite;
- increased salivation.
In rare cases, the disease causes weakness, increased fatigue, and secondary infectious foci appear on the oral mucosa.
What causes alveolitis?
Alveolitis is caused by partial or complete loss of a blood clot in the tooth socket after extraction. Typically, as the first step of the healing process, a small amount of blood will form to cover and protect the exposed jawbone. If the clot is lost or does not form, the bone is exposed and healing is delayed.
Main causes of alveolitis
In general, alveolitis is the result of bacterial, chemical, mechanical and physiological factors. Below are examples for each.
- Bacterial factor: A pre-extraction infection, such as periodontal disease (or periodontitis), often prevents the blood from clotting properly. Some oral bacteria can cause it to break down.
- Chemical: Nicotine consumed by smokers leads to decreased blood flow in the mouth. As a result, a blood clot may not form in the area of the extracted tooth.
- Mechanical: Sucking through a straw, aggressively rinsing the mouth, spitting, or dragging the cigarette causes dislodgement and loss of the blood clot.
- Physiological: Hormones, dense jawbone or poor blood supply also prevent clot formation.
Example of alveolitis socket
Diagnostics
The main symptom of the disease is the appearance of acute pain, which does not subside either 24 hours or 2–3 days after tooth extraction. Sometimes a dentist can identify chronic alveolitis during routine oral examinations. In this case, an empty socket without granulation tissue appears in place of the impacted tooth. The bone is already visible at the bottom of the hole.
The dentist will be able to determine the presence of tissue changes during the examination; radiography and radiovisiography of the affected area may also be prescribed.
Types of inflammation
The most common types of inflammation that occur after tooth extraction are:
- Alveolitis is an inflammation of the walls of the empty socket of an extracted tooth. The patient suffers from swelling, redness, and “tugging” pain. Weakness, malaise appear, and body temperature rises.
- Gingivitis is inflammation caused by tooth extraction. The tissues turn red, begin to swell and bleed.
- Periostitis is an inflammation of the jaw bone (periosteum). The disease is characterized by severe toothache, swelling of the gums, gumboil, and distortion of the facial contour. Pathological mobility of the tooth appears, lymph nodes are palpated in the face and neck.
- Periodontitis is inflammation of the periodontium, the area around the root of the tooth. The disease is characterized by aching or sharp pain in the tooth, which intensifies when biting. Without treatment, the pain gradually turns into throbbing, tearing pain. The patient complains of severe weakness, fever, and sleep disturbances.
- Trauma to the gums from dental fragments. With mechanical damage to tissues, swelling, redness appear, and spontaneous pain begins, intensifying when touched. If the injury persists for a long time, a dark pressure ulcer with purulent and serous discharge may form at the site of injury.
Treatment of alveolitis
When the socket becomes inflamed, the main thing is to eliminate the source of infection, prevent the development of inflammation and preserve the dentition. In order to alleviate the patient’s condition, the dentist uses the following therapy methods:
- Mechanical cleansing of the hole, washing out purulent residues with a solution of nitrofural or hydrogen peroxide.
- Anesthesia of the hole. The pain syndrome is relieved with the help of local applications with anesthetics and analgesics. To do this, the doctor applies the lotion for half an hour and then removes it to prevent the proliferation of microbes in the area. The dentist will advise the patient to repeat the procedure several times a day. Taking painkillers orally is not recommended.
- Taking antibiotics. In the presence of concomitant diseases, alveolitis is treated with antibiotics.
With the right approach, the signs of alveolitis subside 2-3 days after the start of treatment. If therapy was not started on time, residual pain may drag on for 2–3 weeks.
With the permission of the dentist, additional treatment of alveolitis with folk remedies is possible:
- Sage rinses. To prepare the solution, brew a large spoonful of dry sage in 250 ml of boiling water, leave the mixture for an hour, wrapping the container in a towel. After this, the liquid should be filtered and used for rinsing.
- Gargling with chamomile flowers. To prepare the composition, brew a large spoonful of chamomile flowers in a glass of water for 15 minutes, insulating the container with a towel. The infusion should be strained and rinsed your mouth up to 12 times a day.
- Poplar buds. To prepare, take half a glass of buds, pour into a glass container and pour in 500 ml of vodka. The product should be infused for 10 days in the dark and cool, then filtered, soaked in cotton swabs and applied to the inflamed area.
- A soda rinse solution can also be an effective addition in the treatment of alveolitis. You should take a large spoonful of powder in a glass of warm water or mix soda with water to obtain a paste-like mass, which then needs to be used to treat the hole.
- Burdock leaves. To prepare a medicinal decoction of burdock leaves, you need to pour 20 grams of raw material with 2 glasses of water, and then simmer the mixture over low heat for about 40 minutes. The resulting solution should be cooled and filtered, and then used for rinsing.
- Aspen bark. Pour 1 tablespoon of crushed aspen bark into one glass of boiling water. It is important to leave the solution in an airtight container for 3 hours, and then use 100 ml of strained warm liquid at least 3 times a day.
- Anise infusion. To prepare the infusion, pour 1 tablespoon of anise into 200 ml of boiling water, and then keep in a thermos for 50 minutes. The liquid should be filtered and used to rinse 3 times a day.
Treatment at the dentist
The doctor begins treatment by washing the socket and treating it with antiseptic solutions, and then cleans the socket from the remains of the blood clot using a surgical curette. Then the wound is dried with a gauze swab and treated with an anesthetic and antibacterial agents. The wound is covered with a bandage, which is designed to protect the open surface of the wound from possible biological, chemical or mechanical irritants. To check the possibility of detecting pieces of the extracted tooth in the socket, an x-ray can first be taken.
The procedure for cleaning the hole as a whole is carried out according to the following scheme:
- Local anesthesia is performed;
- The well is washed with an antiseptic solution (hydrogen peroxide solution 3%, chlorhexidine 0.05% or furatsilin 0.02%), and food debris and necrotic masses are removed;
- If there are foreign bodies in the hole (root fragments, cysts and granulomas), they are removed using special instruments;
- After cleaning the hole, it is treated with antiseptic solutions, dried with a sterile gauze swab, and turunda with an antiseptic and an anesthetic is injected into it. With a mild degree of inflammation, a turunda may not be necessary; thorough cleansing of the hole and subsequent care for it is sufficient;
- In case of a pronounced necrotic process in the hole, rinsing and application with trypsin is carried out - this is an enzyme preparation that accelerates the breakdown of dead tissue. Trypsin has anti-inflammatory and anti-edematous effects, helps clean the socket from necrotic masses and pus;
- After completing all the manipulations, the patient goes home, the doctor appoints appointment days when he needs to come for antiseptic treatment of the hole and change the turunda, if one has been installed. If necessary, a course of antibiotics is prescribed.
For alveolitis, antiseptic baths (not rinsing) with solutions of chlorhexidine 0.05% or miramistin 0.01%, which can be purchased ready-made at the pharmacy, are effective. When performing baths, the solution is taken into the mouth and held for several minutes, then carefully spat out. To relieve pain and reduce the degree of inflammation, nimesulide or ibuprofen are prescribed.
To prevent the turunda from falling out of the socket, during treatment you need to eat soft, pureed food and do not chew on the sore side. If the turunda does fall out, you need to rinse your mouth with chlorhexidine solution and immediately consult a doctor.
If this is not possible, you should rinse the hole yourself from food debris: to do this, bite off the sharp tip of the needle from a 5 ml syringe, bend it a little, and disinfect it with pure alcohol. A chlorhexidine solution is drawn into the syringe, the needle is inserted into the hole (not too deep) and the piston is pressed intensely to create a liquid pressure that can remove food debris.
All cases of alveolitis treatment are individual, so it may be necessary to visit the dentist up to several times.
With a favorable course of the healing process, the pain goes away, and the inflammatory process gradually subsides and disappears after a few days.
If the process, despite the procedures performed, progresses, then after antiseptics, gauze tampons soaked in propolis tincture or camvorophenol solution (10%) are inserted into the hole. A tetracycline-prednisolone cone inserted into the well has a good antibacterial effect.
Prevention
The best prevention of pathology after tooth extraction is to be attentive to yourself and follow all the surgeon’s recommendations. While the hole is healing, give up bad habits, eating too hot, spicy, sweet foods, and if possible, switch to pureed foods. And if you suspect inflammation, contact your dentist as soon as possible.
Under no circumstances should the first symptoms of alveolitis be ignored. Against the background of inflammation, more serious problems may arise:
- Phlegmon is an acute diffuse purulent inflammation.
- An abscess is a purulent inflammation of tissues with their melting.
- Osteomyelitis is a purulent-necrotic process that can develop in the bone and bone marrow, as well as in the surrounding soft tissues.
- Periostitis is inflammation of the periosteum.
- Sepsis is a severe systemic inflammatory reaction.
- Tissue necrosis is local tissue death.
Modern methods of treating alveolitis make it possible to quickly relieve the symptoms of inflammation and avoid the complex consequences of the disease. The sooner the patient consults a doctor, the less likely it is to develop complications.
What about traditional methods?
Home treatment usually involves temporary pain relief until a dentist can intervene. Methods that provide some relief include:
- using over-the-counter pain relievers;
- Apply a cold compress or sealed ice pack to the affected side of the face (15 minutes);
- rinsing the mouth with salt water to remove food debris;
- using clove oil (place 1-2 drops of oil on a clean cotton swab and gently apply to the affected area).
Clove oil
Again, these methods are only intended to provide temporary relief from unpleasant symptoms. Delaying a follow-up visit to your dentist or surgeon will only prolong the pain as well as recovery time.
Table. Effective folk remedies and their use.
| Home Remedies | How to use |
| Clove oil | Clove oil can be applied directly to an open tooth socket using a cotton pad. First rinse it in water, then apply oil and apply it in place. This will help reduce pain. Repeat the procedure twice a day as needed. |
| Salty water | Dissolve salt in warm water and rinse your mouth. Thus, after some time, relief will come. |
| Yogurt | Yogurt works as a natural antibiotic. He can treat the socket and reduce pain. |
| Ice pack | Alveolitis can lead to swelling of the jaw. To prevent this, apply ice cubes to the sore spot. |
| Iced tea bag | Place a cold tea bag on the affected area. This is one of the most effective home remedies for alveolitis, and all because of tannic acid, which helps reduce pain. |
| Turmeric solution | Mix a pinch of turmeric with warm water and rinse your mouth with the solution to get rid of pain associated with alveolitis. |
| Paste of salt, turmeric and mustard oil | To get great socket pain relief, mix these ingredients together to form a paste and apply it directly to the affected area. |
| Gauze | Exposing the socket to air or saliva will only make the pain worse. You can prevent it by biting gauze soaked in water. |
| Valerian root | It is an extremely effective natural tranquilizer that provides powerful pain relief, speeds up the healing process, and reduces stress and anxiety. |
| Lemon and salt | Lemon is a natural healer that contains a lot of vitamin C, and its juice can significantly improve the healing process of the socket after wisdom tooth removal. Mix lemon juice with salt and apply it to the affected area. |
| Moisture maintenance | Drink plenty of water as this is essential to reduce or prevent pain associated with alveolitis. |
Treatment of alveolitis in STOMA clinics
Surgeons at STOMA clinics are required to examine patients and give recommendations on how to care for the hole formed after tooth extraction. If problems arise after extraction, the patient can always call the clinic and clarify whether inflammation has really begun and what to do to reduce pain.
At any time after removal, the patient can contact our clinics. The attending surgeon will examine him and prescribe appropriate therapy.
Feel free to call us at any time and consult about your condition. The sooner we start treating alveolitis, the lower the risk of complications.
Treatment in hospital
- Surgical intervention.
Surgical intervention may be necessary if, during dental X-rays, the doctor reveals an incompletely removed tooth or bone fragments in the soft tissues. The resulting granulation tissue must also be removed.
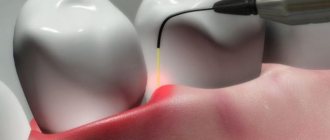
- Physiotherapeutic treatment.
The following are used as physiotherapy:
- Magnetotherapy
- Exposure to laser radiation
- Electrophoresis
- Ultraviolet irradiation
- Fluctuarization
- Microwave therapy
Early treatment includes:
- Use of analgesics
- Washing the alveoli with antiseptic solutions
- Removing foreign particles from the site of inflammation
- Repeated rinsing
- Application of a lotion with analgesic and anti-inflammatory effects
Late stage treatment includes:
- Washing and anesthesia of the alveolar socket
- Nerve block with Lidocaine (repeat if necessary)
- Regular rinsing of the mouth with a solution of potassium permanganate
- Introduction of proteolytic enzymes into the wound (to get rid of dead tissue)
- Antibiotic therapy