September 26, 2020
Most people have no idea what jaw bone atrophy is. But it is simply necessary to know about this, especially when you lose teeth and are in no hurry to restore them. Why is this so important? What does it affect? What consequences does it lead to? The editors of the UltraSmile.ru portal will tell you about this in clear and accessible language. In the article we will also talk about whether bone atrophy can be prevented and what treatment options are possible if it has occurred.
What is atrophy
Jaw bone atrophy is a pathological process that leads to a decrease in cell size and loss of the normal volume of bone structures (both in width and height). With atrophy, negative changes begin to occur in the body and the full functionality of the maxillofacial apparatus is disrupted.
Atrophy is a decrease in bone volume
Bone
Bone tissue is the main supporting tissue and structural material for bones, i.e., for the skeleton. Fully differentiated bone is the strongest material in the body, with the exception of tooth enamel. It is very resistant to compression and tension and is extremely resistant to deformation. The surface of the bone (except for the articulated surfaces) is covered with a membrane (periosteum), which allows bone to heal after fractures.
The mechanism of atrophy
The jaw bone is heterogeneous; it consists of several layers:
- central: this is the top layer where a large number of capillaries and vessels are located. This layer is quite loose or, as it is also called, spongy,
- cortical shell: consists of bony septa,
- basal: very dense section, not subject to atrophy and inflammatory processes. This is, in fact, the basis of the jaw bone, its base.
The jaw bone consists of several layers.
If the oral cavity is healthy and a person’s natural teeth are completely intact, then all layers of bone tissue receive adequate nutrition and blood supply. They function under the influence of chewing pressure. However, if the load for some reason disappears or changes (destruction, tooth loss and removal, periodontal inflammation), then negative consequences occur. The central spongy area is most affected.
If a person removes a tooth, then an empty space appears in the central part of the bone, there is no chewing load, and accordingly, food ceases to flow into this area, that is, it is, as it were, de-energized. Gradually, the spongy layer becomes thinner, it literally “melts” - this is called jaw atrophy. At the same time, the cortical and basal sections retain their volume.
Osteocytes
Osteocytes are mature, well-differentiated bone cells, located one at a time in lacunae, also called bone cavities. The cells are oval in shape with numerous processes. The size of osteocytes is approximately 30 μm in length and up to 12 in width. The nucleus is elongated and located in the center. Chromatin is condensed and forms large clumps. The organelles are poorly developed, which may explain the low synthetic activity of osteocytes. Cells are connected to each other by processes through cell contacts of nexuses, forming a syncytium. The processes carry out the exchange of substances between bone tissue and blood vessels.
The main causes of the pathological process
Jaw atrophy develops due to many factors:
- tooth extraction and untimely restoration: this is the main reason. All other circumstances listed below sooner or later again lead to loss of teeth,
- periodontal inflammation: periodontitis is the #1 cause of early tooth loss. The disease in its advanced stage leads to the destruction of the ligaments that hold the teeth in the sockets, causing them to become loose, shift and fall out,
- periodontal disease: not to be confused with periodontitis! This is a much less common systemic pathology,
- chronic diseases: diabetes, osteoporosis, cardiovascular pathologies, thyroid problems,
- bad habits: for example, smoking,
- metabolic disease,
- elderly age,
- injuries.
Features of the destructive process in the upper and lower jaw
Bone atrophy is a gradual process, but quite rapid. So, if a tooth is removed, negative changes begin almost immediately, but in the upper and lower jaws they occur slightly differently.
Atrophy of the lower jaw occurs more slowly and in the future creates fewer difficulties for prosthetics and implantation. This is easy to explain: the mandibular bone is very massive and dense, because it contains teeth that take on serious loads during the process of chewing food.
Bone atrophy is a gradual process, but quite rapid.
Atrophy of the upper jaw is a much faster process. Here the bone is thin, it is more fragile, and accordingly, all destructive changes occur faster, which in the future creates significant difficulties if the patient wants to undergo implantation and prosthetics.
Bone remodeling
During the process of restructuring, coarse fibrous connective tissue is replaced with lamellar tissue, bone substance is renewed, and the content of mineral substances is regulated. On average, 8% of bone matter is renewed per year, and spongy tissue is renewed 5 times more intensely than lamellar tissue. In the histology of bone tissue, the mechanisms of bone remodeling are given special attention.
Remodeling includes resorption, tissue destruction and osteogenesis. With age, resorption may predominate. This explains osteoporosis in older people.
The restructuring process consists of four stages: activation, resorption, reversion and formation.
Bone tissue regeneration in histology is considered as a type of bone remodeling. This process is very important, but most importantly, knowing the factors influencing the regeneration process, we can speed it up, which is very important for bone fractures.
Knowledge of histology and human bone tissue is useful for both doctors and ordinary people. Understanding some mechanisms can help even in everyday things, for example, in treating fractures and preventing injuries. The structure of bone tissue in histology is quite well studied. But still, the bone tissues are far from fully studied.
Consequences of a negative process
Adentia (lack of teeth) provokes a lot of problems, and atrophy of the jaw bone is not the only one of them. Destructive processes lead to the fact that with the loss of natural tissue volume, a person develops external changes in the contour of the face. This becomes especially noticeable if all teeth are missing: the number of facial wrinkles increases, lips and cheeks recede, asymmetry appears, visually a person looks older than his age, and sagging skin is noticeable.
A person experiences external changes in the facial contour
Health problems begin, the gastrointestinal tract suffers, and the clarity of pronunciation of sounds is impaired.
The most unpleasant thing is that even timely installed removable dentures and bridges do not save you from the problem. As the atrophic processes progress, they begin to cause more and more trouble: they no longer fit tightly to the gums and become displaced. Between the dentures and the mucous membrane, as a result of thinning of the bone tissue, a gap or gap is formed, into which food particles and bacteria penetrate, provoking the development of the inflammatory process. To get rid of these defects, patients often have to go to the correction of prostheses, buy adhesives and fixing creams.
There is another problem that atrophy leads to. If you have lost one or more units, and after a few years you decide to restore them with implantation, then difficulties will arise. Which? If there is insufficient bone volume, the implant cannot be securely fixed in it. He just won't hang in there. In addition, during the installation process, the doctor can injure nerves, touch the maxillary sinuses and adjacent areas. To avoid this, bone augmentation will have to be done before implantation. And this is a very costly and unpleasant manipulation that takes a lot of time. After it, you need to wait until the tissues heal, which usually takes 4-6 months.
Indirect osteogenesis
Indirect osteogenesis occurs during the development of tubular and spongy bones. To understand all the mechanisms of osteogenesis, you need to have a good understanding of the histology of cartilage and bone connective tissue.
The whole process can be divided into three stages:
- Formation of a cartilaginous model. In the diaphysis, chondrocytes become starved of nutrients and become vesicular. The released matrix vesicles lead to calcification of the cartilage tissue. In histology, cartilage and bone tissue are interconnected. They begin to replace each other. The perichondrium becomes the periosteum. Chondrogenic cells become osteogenic, which in turn become osteoblasts.
- Formation of primary cancellous bone. In place of the cartilaginous model, rough fibrous connective tissue appears. A perichondral bone ring, a bony cuff, is also formed where osteoblasts form trabeculae directly at the diaphysis. Due to the appearance of a bone cuff, nutrition of the cartilage becomes impossible, and chondrocytes begin to die. Cartilage and bone tissue are very interconnected in histology. Following the death of chondrocytes, osteoclasts form channels from the periphery of the bone to the depth of the diaphysis, through which the movement of osteoblasts, osteogenic cells and blood vessels occurs. Enchondral ossification begins, eventually turning into epiphyseal ossification.
- Tissue restructuring. The primary coarse fibrous tissue gradually turns into lamellar tissue.
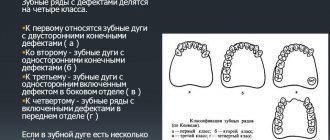
Degree of development of pathology
Doctors distinguish four stages. In the first, the bone has a satisfactory volume, and if the patient wishes, the tooth can be restored without resorting to the procedure of increasing bone tissue during implantation. At the second stage, gum loss is noticeable, the first destructive processes are just beginning, but the bone tissue is still suitable for implantation.
There are four stages of atrophy development
At the third stage, the loss is uneven, but it is quite pronounced, so if you want to do implantation, you can’t do without procedures to increase the volume. At the fourth stage1, strong destructive processes are noticeable in the central section (there is practically no spongy substance left here), and when restoring a tooth using traditional implantation methods, increasing the volume is mandatory.
Osteoblasts
Osteoblasts are cubic, oval-shaped cells with an eccentrically located nucleus. The size of such cells is approximately 15-20 microns. The organelles are well developed, granular ER and the Golgi complex are pronounced, which may explain the active synthesis of exported proteins. In histology on a bone tissue specimen, the cytoplasm of cells is stained basophilic.
Osteoblasts are localized on the surface of bone beams in the forming bone, where they remain in mature bones in the spongy substance. In formed bones, osteoblasts can be found in the periosteum, in the endosteum covering the medullary canal, and in the perivascular space of osteons.
Osteoblasts take part in osteogenesis. Thanks to the active synthesis and export of proteins, the bone matrix is formed. Thanks to alkaline phosphatase, which is active in the cell, minerals accumulate. Do not forget that osteoblasts are the precursors of osteocytes. Osteoblasts secrete matrix vesicles, the contents of which trigger the formation of crystals from minerals in the bone matrix.
Osteoblasts are divided into active and resting. Active ones participate in osteogenesis and produce matrix components. Resting osteoblasts with an endosteal membrane protect bone substance from osteoclasts. Dormant osteoblasts can be activated during bone remodeling.
Implantation methods and atrophy: what options are possible
Jaw bone atrophy is not a disease, but a pathology, the development of which, ideally, can be prevented immediately after root removal. Adequate and timely treatment will help with this, namely, prosthetics on implants. There are also implantation options that are possible for atrophy, but first things first.
An implant is an analogue of a tooth root. It is implanted into the bone and acts specifically on it, in contrast to removable and bridge prostheses, which restore only the visible part, that is, the crown. The artificial root forces the bone to work, regenerate, puts pressure on it while chewing food, due to which it again begins to receive the necessary nutrition.
One-stage treatment protocol
With this approach, an artificial root is installed in the hole of the element that was just removed, or next to it. That is, two procedures, removal and implantation, are carried out simultaneously. The method helps preserve bone structures and subsequently avoid augmentation procedures. If conditions allow (high initial stability of the implant), then the implanted rod can be immediately loaded with a lightweight fixed crown, otherwise you will have to wear a removable immediate prosthesis and wait for the implant to heal, which on average takes up to six months.
With one-stage implantation, an artificial root is installed in the socket immediately after tooth extraction
The approach saves time, money, avoids osteoplastic surgery and difficult rehabilitation.
“My husband is a dentist, so I’ve heard a lot about bone tissue augmentation during dental implantation. When I needed to remove one tooth, I clearly did not want to go through this operation. At the clinic, my husband was advised not to delay, but to immediately install the Nobel implant, which was done. It was first closed with a removable denture, and after 3-4 weeks a permanent crown was made. I was surprised that it was so fast. But it turns out that Nobel was not recommended in vain, because he has super-coating (according to my husband’s colleagues), which helped get everything done so quickly.”
Anna, fragment of a review from the site Irecommend.ru
Classic two-stage implantation with bone augmentation
Suitable for solving the problem of missing 1-2 teeth. Involves two stages of treatment. The first includes careful preparation and installation of implants, the second - fixed prosthetics. Here, permanent prosthetics can be carried out only after the artificial roots have taken root - on average, this will take 4-6 months, during which time the “gap” in the smile will have to be hidden with a removable denture.
The photo shows a classic two-stage implantation
There is another big disadvantage with this approach - before placing implants, the doctor determines the condition of the bone, and if it is atrophied, then it needs to be built up. And this is a mandatory condition, without which the method is simply inapplicable, because it uses classical models of implants, which, when installed, are implanted into the cancellous layer of bone, the same one that undergoes resorption after root removal.
If you have had a tooth removed, you are in a hurry to restore it as quickly as possible, because years later it is unlikely that you will be able to avoid the build-up of bone tissue. But you can do without surgery if you have multiple defects or teeth are completely missing. How? Read on!
One-stage implantation without bone augmentation
It involves the installation of implants and the immediate fixation of prostheses on them (within 2-3 days), and immediately non-removable ones. The main thing is that in 90% of situations the method allows you to do without bone grafting, even in the case of severe atrophy and inflammatory processes in the tissues. This can be achieved with special models of implants that can be installed at an angle. Thanks to this, layers that are not subject to atrophy and inflammation are used, including the cortical plate and the basal region - they, as noted above, do not undergo resorption and retain the density and volume necessary for reliable fastening of the implant. In the arsenal of experienced doctors there are also models that are placed even deeper, extend beyond the jawbone and capture the bones of the skull, cheekbones, and chin area - such implants are called zygomatic.
The photo shows the method of installing zygomatic implants
The implant models commonly used for this approach have a number of other advantages, for example, antibacterial or anti-inflammatory coating, which accelerates the process of engraftment and tissue regeneration.
And the fixed prosthesis itself, installed almost immediately, makes it possible to give the implants stability and stability. And the fact that the patient immediately begins to chew food with it leads to the fact that the jaw bone starts working, begins to receive the necessary nutrition and is restored naturally.
One-stage implantation includes several treatment protocols: all-on-3, all-on-4, all-on-6, basal complex. Thanks to the variety of methods, doctors can find an approach to each patient, work with the most complex clinical cases, and eliminate the build-up of bone structures.
Diagnosis of peri-implantitis
Once signs of gum peri-implantitis appear, it is necessary to determine the cause of the disease. For this purpose, computed tomography or x-ray is used. The doctor examines the condition of the bone tissue and determines the reason for the rejection of the metal structure. Depending on the result obtained, a correction is made.
With peri-implantitis, a deep and wide periodontal pocket is formed, and bone tissue begins to thin and collapse.
Correction methods for peri-implantitis largely depend on how long ago the prostheses were installed. If rejection occurs within a month after implantation (up to six months), then the cause of the pathology lies in the incorrect actions of the orthopedist. If an artificial tooth begins to wobble a year or three years after installation, this is due to the fault of the patient himself. Either he did not maintain oral hygiene, or he injured his jaw or developed a chronic disease.
If the crown of an artificial tooth has come loose, it is fixed with dental cement. If the crown previously stood on cement, the surgeon replaces the fixation method with another. It is impossible to determine in advance the method of working with a broken orthodontic structure, because the reasons for its rejection by jaw tissue are different for everyone.
Stages of pathology development
The method of treating pathology depends on the stage of its development, there are four of them.
The first stage is characterized by slight swelling of the gum tissue around the prosthesis, redness and formation of a gum pocket, and bleeding. The artificial tooth becomes mobile and interferes with chewing food. But the integrity and density of the supporting bone are not changed, so the structure can be saved from falling out with the help of conventional conservative treatment.
At the second stage, bone mass decreases, gum tissue becomes loose, and deep gum pockets appear. The denture wobbles greatly in the oral cavity, since the gums cannot hold it in a stable position.
At the third stage, severe pain appears at the site of pathological changes in the gum tissue, the metal rod is exposed due to severe gum loss. Pain accompanies every touch to the place where the rod is installed.
Peri-implantitis of the fourth stage is accompanied by severe destruction of bone tissue, which can no longer support the implanted parts. The source of inflammation often spreads to healthy teeth, and the patient’s health condition worsens.
Common methods of osteoplastic surgery
As we have already found out, there will be a need to build up bone only in cases where the patient is indicated for a two-stage implantation technique, that is, you are missing one or more teeth that were lost more than a year ago. In all other cases, approaches are applicable that allow one to abandon procedures that are so traumatic and require long-term rehabilitation.
So, if before implantation you were informed about the need to build up the bone due to atrophy, then the options may be as follows.
Sinus lift
Suitable only when it is necessary to restore the teeth of the upper jaw. Doctors distinguish open sinus lifting in dentistry and closed one. What it is? These are procedures that involve changing the height of the jaw bone, so as not to subsequently injure the maxillary sinuses and have the necessary volume of tissue for reliable fixation of the implant.
The photo shows a diagram of the sinus lift operation
What is a closed sinus lift in dentistry? A closed procedure is performed if it is necessary to increase a small amount of tissue. In some clinical cases, it allows the simultaneous installation of an implant, which 4-6 months after surgery (after complete engraftment) can be loaded with a fixed prosthesis.
Open surgery is required if the bone has lost significant height. The operation is quite traumatic, so it is impossible to install an implant at the same time. First you will have to undergo rehabilitation, which will take up to 6-8 months. And only after this, if there are no complications, you can begin installing artificial roots.
The photo shows a diagram of an open sinus lift
Autotransplantation
Expensive and traumatic procedure. It involves not one, but several surgical interventions at once. First, donor material is taken from the patient himself (for example, from the chin area), which is then planted in the place where atrophy is present. Why so many complex manipulations? It is believed that one’s own material takes root better and faster and is not rejected by the body. However, after the procedure there will be a long rehabilitation period, and it will be possible to begin installing implants only after complete engraftment of the tissues.
In this operation, the patient's own tissue is transplanted
Guided bone regeneration
The best option among those presented, as it is less traumatic and allows for the simultaneous installation of implants. The operation uses artificial bone chips and synthetic materials, as well as self-absorbing membranes that do not cause allergic reactions.
Artificial bone chips are used for the operation.
Possible complications after bone grafting
Modern researchers have come to the conclusion that the operation has more disadvantages than advantages. There are often cases when planted material does not take root. In addition, even in the case of successful engraftment, the implanted structure usually has a lower density, implants are less well fixed in it, which, in turn, leads to their rejection.
Situations are common when, due to insufficient qualifications, the doctor who performed the procedure makes a number of mistakes that lead to complications for the patient. Thus, in the upper jaw, the maxillary sinuses can be damaged and thereby cause an acute inflammatory process, chronic sinusitis.
Notice
: Undefined variable: post_id in
/home/c/ch75405/public_html/wp-content/themes/UltraSmile/single-item.php
on line
45 Notice
: Undefined variable: full in
/home/c/ch75405/public_html/wp-content /themes/UltraSmile/single-item.php
on line
46
Rate this article:
( 2 ratings, average: 5.00 out of 5)
prevention
- Nikolsky V.Yu., Veldyaksova L.V., Maksyutov A.E. Assessment of the degree of atrophy of the jaw bone tissue after tooth extraction in connection with dental implantation // Saratov Medical Scientific Journal. – 2011.
Expert “Bone atrophy also occurs in cases where the patient restored the tooth in a timely manner after extraction, but only did it with bridges or removable dentures. Such orthopedic devices restore only the supragingival, that is, the coronal part. They put pressure on the mucous membrane and, one might even say. compact it. Today, it is possible to avoid the problem and significantly slow down atrophy only by using prosthetics on implants, because implants are analogues of roots, performing all their functions and starting the normal processes of nutrition and blood supply to cells.” Dentist-therapist, orthopedist Emil Menirovich Makaev
Consulting specialist
Grigoryan David Sergeevich
Specialization: Implant surgeon, orthopedist Experience: 8 years
Comments
Can I take any vitamins to prevent bone atrophy?
Marianna (04.10.2020 at 14:36) Reply to comment
- Dear Marianna, taking vitamins as an independent measure will not solve the problem. However, vitamins, in particular vit. D, help improve the quality and structure of bone tissue. This vitamin is often prescribed in postoperative periods, for example, after tooth extraction or after installation of implants, also after bone tissue augmentation.
Editorial staff of the portal UltraSmile.ru (07.10.2020 at 09:24) Reply to comment
I want to install mini-implants, because... they have a very good price. Will they save you from atrophy?
Makarchenko (10/29/2020 at 6:27 pm) Reply to comment
Write your comment Cancel reply
Stock
-6%
BASAL COMPLEX - Restoration of teeth on 1 jaw in 3 days 265,000 rub.
250,000 rub.
get -37 %
Osstem dental implant and metal-ceramic crown RUB 63,000.
40,000 rub.
get -44 %
Osstem implant + zirconium dioxide crown 80,000 rub.
45,000 rub.
get -40 %
Teeth cleaning and whitening RUB 5,000.
3000 rub. get