What it is
This is the medical name for the result of inflammatory processes in the oral mucosa. With the help of special enzymes contained in saliva, it protects the entire digestive tract, processing food so that it is not harmful to health. Inflammation appears both in a visible place, for example, on the lip or cheek, and deep in the throat, where it is not always and cannot be immediately detected. Different people are exposed to it with different frequency: some – once every few years, others – annually, others – monthly. It depends on the strength of the immune system and the internal characteristics of the body.
12.3.3.1. Candidiasis
This disease, caused by fungi of the genus Candida, is also called candidomycosis, moniliasis, thrush, etc.
The causative agent is a yeast-like, opportunistic fungus (Candida albicans, less commonly Candida tropicalis or other types of Candida fungi), an aerobe, widespread in the environment. It is found on the surface of healthy skin and mucous membranes, in the secretions of the human body. Candida albicans is part of the resident flora of the human oral cavity and is normally found in small quantities and in an inactive state in 50-70% of cases.
The occurrence of candidiasis is promoted by:
1) prolonged use of antibiotics;
2) unsatisfactory hygienic condition of the oral cavity;
3) the presence of galvanism;
4
) inhibition of the functional activity of local protective (immunological) factors;
5) radiation therapy;
6) immunosuppressive therapy.
Rice. 12.14. Candidal glossitis, pseudo-membranous form.
In diagnosis, microbiological indicators are of paramount importance, as well as the identification of mycelial threads in native preparations from lesions obtained by scraping.
Clinical picture. There are pseudomembranous, atrophic and hyperkeratotic forms of oral candidiasis.
For pseudomembranous
form, the lesion is localized on the mucous membrane of the cheeks, tongue, palate, and gums. Less commonly, the process can spread to the larynx, pharynx and esophagus. The plaque is easily removed, after which a smooth, hyperemic surface is exposed. Plaque consists of epithelial cells, fibrin, microorganisms and yeast mycelium. Patients complain of burning, dryness, discomfort, sometimes pain, and viscous saliva may be noted (Fig. 12.14). Candidiasis occurs more often in older people, against the background of B-hypovitaminosis and decreased bite height.
With atrophic
form, the mucous membrane is sharply hyperemic (candidal stomatitis), sometimes slightly swollen. When the lips are affected (candidal cheilitis), the mucous membrane (usually the lower lip) is hyperemic, sometimes covered with whitish crusts. The localization of manifestations of candidal glossitis often coincides with the folds of the tongue. There are complaints of dryness, burning and soreness in the relevant areas.
Hyperkeratotic
the form resembles pseudomembranous, but the plaque is tightly fused to the underlying tissue, impregnated with fibrin and is difficult to remove. After removing it, the bleeding surface is exposed.
Differential diagnosis. Candidiasis is differentiated from catarrhal allergic stomatitis, diseases accompanied by keratinization (leukoplakia, lichen planus, lupus erythematosus), coated tongue, and traumatic lesions. Fungal seizures should be differentiated from seizures of other origin: streptostaphylococcal, vitamin deficiency, syphilitic, due to a decrease in the height of the bite. Candidiasis is characterized by dry or slightly weeping erosion with little discharge, surrounded by thin gray scales, and lack of compaction at the base. Candidal cheilitis should be distinguished from cheilitis of another etiology, lichen planus and lupus erythematosus. Candidiasis can be a symptom of AIDS. Therefore, in the presence of persistent candidiasis, it is necessary to conduct an examination for HIV infection.
Laboratory diagnostics. To confirm the clinical diagnosis, a microscopic examination of scrapings from the affected areas and removable dentures must first be carried out. It is advisable to take the material for research on an empty stomach before brushing your teeth and rinsing the mouth, or at least 3-4 hours after eating or rinsing.
Rice. 12.15. Cytological picture of candidiasis: 1 - spores; 2 - pseudomycelium of Candida albicans. Microphotograph, x 1200.
In the oral cavity, a yeast-like fungus of the genus Candida lives in the form of round or ovoid cells with a diameter of 1-5 microns with clear outlines, surrounded by a clearing zone, or in the form of pseudomycelium, less often mycelium (pseudohyphae and hyphae) of the fungus, which looks like threads 1-5 microns thick, which are characterized by branching figures. Both the yeast-like cells and the pseudomycelium (mycelium) of the fungus bud during parasitism. Normally, fungi of the genus Candida can be found in the form of single yeast-like cells in a preparation - a scraping. When suffering from candidiasis or a complication of candidiasis from another disease, the fungus occurs in the form of yeast-like cells and in the form of mycelium (pseudomycelium) with division figures in many fields of view (Fig. 12.15). In the acute onset of the disease, cellular forms usually predominate; in the chronic course, pseudomycelium predominates. When taking antibiotics, a similar microscopic picture can be observed without clinical signs of candidiasis. This condition is regarded as a manifestation of dysbiosis and is a signal about the possibility of candidiasis.
To clarify the diagnosis and type of fungus, a cultural study is carried out with inoculation on solid media, always taking into account the number of colonies grown from a certain amount of material. In some cases that are difficult to diagnose, especially with chronic hyperplastic candidiasis, it is necessary to resort to biopsy.
The treatment is complex. Traumatic factors should be eliminated, and first of all, prostheses made of dissimilar metals (especially if the spraying method was used). A complex of multivitamins is prescribed, especially group B. Among the general remedies, in addition to levorin or nystatin, diflucan is prescribed - 1 capsule (50 mg) per day for 7-14 days under the control of microbiological studies, nizoral - 1 tablet (200 mg) per day. day for 14-21 days.
The mucous membrane is treated with sodium bicarbonate solution or other alkaline solutions, 10% sodium borate solution in glycerin, 1% clotrimazole cream, or fluconazole is used in the form of applications 4-5 times a day. Decamine caramel and aniline dyes have a certain effect. The prognosis is favorable, however, given the chronic course of the disease, courses of treatment are repeated at intervals of 3-6 months until stable remission is achieved.
Treatment of underlying diseases is carried out by appropriate specialists. Multivitamins (B1, B2, B6, PP, C) are prescribed internally. Trauma to the oral mucosa should be excluded. Sanitation of the oral cavity can begin 2-3 days after the start of treatment.
In case of acute candidiasis, removable dentures are not worn; in case of chronic candidiasis, they are thoroughly cleaned and treated with the same means (except for dyes) as the mucous membrane.
Prevention must necessarily include oral care and denture care. For long-term treatment with antimicrobial antibiotics and corticosteroids, nystatin or levorin 1,500,000 units per day, vitamins B and C, and alkaline mouth rinses are prescribed orally. Prevention of candidiasis in newborns consists of prenatal sanitation of the genitals of pregnant women in antenatal clinics, a strict sanitary and hygienic regime in maternity hospitals, and instillation of a nystatin suspension into the oral cavity of children in the first days of life.
Forms of manifestation
There are many factors that provoke inflammatory processes, and their differences underlie the creation of a special classification.
Aphthous
Aphthae are small ulcers up to 5 millimeters in size. They usually have a white or grayish coating in the form of a small bubble, which then deflates and forms a single eroded area. These aphthae grow as a result of advanced viral, bacterial or chronic diseases of any internal organ.
This type has several forms:
- fibrinous, which occurs when blood begins to circulate poorly;
- necrotic (rare), in which tissue dies;
- granular, affecting the salivary glands;
- deforming the soft palatine part;
- scarring, damaging the acinus and connective tissue.
Herpes
Children often develop type I herpes virus, which actively develops in the epithelium and lymph nodes and then infects the skin. This can cause the temperature to rise, which kills the viral cells. But the immune system weakens, and it takes at least one to two weeks to restore it.
Gorlova
Only 20 percent of patients experience it. Yellowish-gray sores usually form on the base of the tongue, throat tissues, and the roof of the mouth. Swelling of the ligaments in this form is very dangerous, as it makes breathing and eating difficult. Pain in the larynx, cough and runny nose may occur.
Stomatitis gonorrhea – Gonorrhea
Gonorrheal stomatitis is caused by contact with Neisser's gonococcus on the damaged mucous membrane. Infection can occur in various ways: a) exogenous - introduction of gonococcus into the oral cavity from the genitals (autoinoculation), infection of a child from a sick mother during childbirth; b) endogenous - metastatic introduction of gonococcus through the blood and lymphatic routes.
Symptoms. At the beginning of its development, the disease resembles an aphthous lesion. In newborns, it is usually combined with eye damage (for more details, see the article Gonorrheal stomatitis in children).
The mucous membrane of the oral cavity is swollen, brightly hyperemic and painful. Superficial erosions are covered with a dirty gray or yellowish coating containing a large number of gonococci. There is a bad odor coming from the mouth.
After removing the plaque, the bleeding surface is exposed.
In adults, the disease is often complicated by secondary infection with the appearance of deep cracks and abrasions.
The most common locations are the anterior two-thirds of the tongue (the edges remain free), the anterior part of the hard palate, the soft palate, the transitional fold, the gums and the lower lip.
A bacteriological examination of the discharge reveals gonococcus.
Treatment
. The use of antibiotics and sulfonamides quickly cures the disease.
The prognosis with treatment is always favorable. If left untreated, the disease persists in the oral cavity for a long time. It is possible to transfer gonococci to the mucous membranes of the eyes and nose.
Sources used: www.blackpantera.ru
RELATED ARTICLES: After treatment for gonorrhea, you can get pregnant after Gonorrhea drugs Gonorrhea for 5 years Drawings of gonorrhea Does gonorrhea affect the mouth Chronic gonorrhea
Gonorrheal stomatitis
Gonorrheal stomatitis (stomatitis gonococcia) is an acute infectious disease of the oral mucosa, caused by Neisser's gonococcus.
The incubation period ranges from 1 day to 1 month or more. Gonococci that have entered the oral mucosa, after 3-4 days, reach the subepithelial connective tissue through the intercellular spaces and cause an inflammatory reaction with the formation of purulent exudate, which is considered as the migration of neutrophil granulocytes and plasma cells to the site of pathogen invasion.
Children become infected during birth, and the mucous membranes of the eyes and nose are simultaneously affected.
With gonorrheal stomatitis, the mucous membranes of the lower parts of the oral cavity (lips, gums, lateral and lower surfaces of the tongue and the floor of the oral cavity), as well as the pharynx, tonsils, and larynx are affected. It has a brightly hyperemic color and an extremely large amount of gray, sometimes with a greenish tint and an unpleasant odor of purulent plaque. However, patient complaints are usually absent.
Diagnosis of gonorrheal stomatitis
The diagnosis is confirmed by the presence of gonococcus during microscopy of the exudate.
Treatment of gonorrheal stomatitis is identical to the treatment of purulent-necrotic lesions of the oral mucosa. Local etiotropic therapy is carried out with antibiotics and other antimicrobial agents (oleandomycin, gentamicin, metrogil, sulfacyl sodium, fusidine sodium, etc.). Before recovery, it is necessary to carry out preventive measures to avoid infection of the patient’s family members.
Sources used: stom-portal.ru
Stomatitis in a child
Children, as a rule, are less resistant to bacterial and other diseases, since their body is still poorly resistant to external influences.
Viral
There are many viruses that cause this disease. It depends on which of them gets into the child’s body how hard he will endure it and how quickly he will recover. The child may feel a sore throat that gets worse when swallowing or chewing. Body temperature rises to 37-39 degrees.
This form is accompanied by swollen lymph nodes, cough and runny nose, so it is often confused with a common cold, without paying attention to mouth ulcers.
Candida
Young children love to put things in their mouths, this is how they learn about the world. Therefore, they have a higher risk of getting harmful bacteria, especially if you do not keep your hands clean. Sometimes parents forget to wash fruits bought in the store, and then it is difficult for children’s immunity to cope with germs. This leads to inflammatory processes on the mucous membrane: ulcers and areas with a white coating and a cheesy texture appear. When mechanically damaged, they begin to bleed.
Aphthous stomatitis in children: symptoms, causes and features
Aphthous stomatitis is considered a chronic recurrent disease. It manifests itself in the form of exacerbations (relapses) during periods of decreased immunity, seasonal changes in the body, or exacerbations of chronic
diseases. The following internal factors often cause aphthous stomatitis:
- Iron-deficiency anemia;
- chronic digestive diseases - biliary dyskinesia, gastritis, cholecystitis, chronic constipation, inflammation of the pancreas.
Also, one of the probable causes of aphthous stomatitis is an allergic reaction. Therefore, when treating aphthae in the mouth, antihistamines (allergy medications) are prescribed.
Aphthous stomatitis is accompanied by the formation of a small number of large ulcers (up to 1 cm in diameter). They have a round shape and are covered with plaque. The mucous membrane at the edges of the ulcers is painted bright red.
Aphthae are localized on the tongue, cheeks, anterior palate - in those places where the mucous membrane is most often injured (by a bite while eating, a burn from hot food).
Aphthae are very painful. Lidocaine rinses or irrigations can be used for temporary pain relief. But you should not use this remedy often. It causes dryness of the mucous membrane and aggravates the treatment.
In many cases, aphthous stomatitis goes away within 2-3 weeks after its onset.
. But due to the pain and great discomfort, it is possible to speed up the healing of wounds in the mouth with regenerating gels.
What is used to treat canker sores in children?
- antihistamines - relieve allergic manifestations and inflammation (Suprastin, Diazolin, Tavegil);
- antiseptic rinses - Miramistin, Cholisal (this remedy has an additional analgesic effect);
- anti-inflammatory gels with regenerating effects : Solcoseryl-gel, Stomatofit A (also additionally relieves pain).
The gel is applied to the affected areas of the mucosa after rinsing and blotting with a dry gauze swab.
What else is needed to treat aphthous stomatitis?
- Visit a dentist, remove plaque and fill existing carious holes.
- Stop taking medications (if there were any, they may have caused an allergic reaction and the appearance of aphthae).
- Normalize the microflora of the oral cavity - dissolve the contents of capsules with bifidobacteria, Immudon tablets under the tongue up to 3 times a day.
- Examine and treat the gastrointestinal tract - stomach, liver, intestines.
Where does stomatitis occur?
Finding signs of the disease right away is not so easy, since inflammation can appear in absolutely any area.
On the lip
Here the skin is very thin and sensitive, especially on the lower part. There are several causes of ulcerative formations:
- herpes virus;
- burns;
- severe chapping and dryness;
- consequences of chickenpox, measles or scarlet fever;
- pregnancy period.
On the gum
Most often this affects newborns, preschoolers and adults. In this place, the affected area is visible only at an early stage, later it spreads over the entire inner surface of the cheek and lip. At the same time, the corners of the mouth become covered with small cracks.
In the sky
Young children are more likely to experience this as they are not able to take care of their hygiene on their own. They take other people's toys, stones and branches from the ground from the floor and then gnaw them and taste them. All this leads to the formation of white plaque, especially if the body is not resistant to bacteria.
On the tongue
In this area, the disease occurs not only due to a lack of hygiene procedures, but also due to sleep disturbances. If a person, especially a small child, gets little rest and experiences a lot of stress, his health deteriorates.
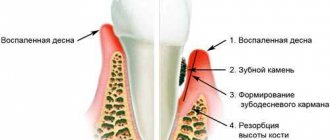
Gum inflammation
Gingivitis is the most common periodontal disease, which can cause inflammation of the lymph nodes. The disease occurs in the absence of systematic oral care, irritation of the gums by sharp edges of teeth, fillings or incorrectly selected dentures. Presence of tartar, caries, and damage to the gums during tooth extraction predisposes to the disease.
With gingivitis, gums bleed when eating or brushing your teeth. Bad breath is often observed.
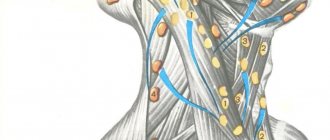
Pressing on the gum papilla leads to pain and slight bleeding. When the inner surface of the gums on the lower jaw is damaged, the submandibular lymph nodes may become enlarged, and when the gums on the outer surface are inflamed, the chin lymph nodes are affected. Gum disease of the upper jaw leads to changes in the deep cervical lymph nodes.
In an adult, gum inflammation in most cases occurs as a chronic, sluggish process. In a child, after an illness (for example, a sore throat), with a lack of vitamins, or stress, an ulcerative form of gum inflammation may occur. The disease is accompanied by the following symptoms:
- increased body temperature;
- headache;
- indigestion.
Lymph nodes become enlarged and painful. In a child, the consequence of gingivitis may be the growth of gum tissue.
When wisdom teeth erupt, acute inflammation of the gums – pericoronitis – may occur. The gums on a wisdom tooth that has not fully erupted form a kind of hood, under which food debris, microbes, and saliva accumulate. The onset of the disease is characterized by the appearance of severe, shooting pain and swelling. Body temperature rises, lymph nodes enlarge. Flux can develop as a complication of the disease. Recurrence of gum inflammation indicates the need for wisdom tooth removal.
Methods for treating stomatitis
There are many options to cope with this disease. But in any case, it is impossible to do without consulting a doctor; only he will be able to correctly identify the pathogen and correctly prescribe the necessary medications.
Home treatments
Often people do not go to the dentist, but try to relieve inflammation on their own by rinsing with various means, maintaining hygiene, and so on. Sometimes this helps, but a good result cannot be guaranteed - it is not always possible to select medications.
Therefore, do not neglect examination by a specialist, even if you manage to remove the ulcers once, they will come back again.
Folk remedies
There are some universal natural antiseptics with an anti-inflammatory effect: chamomile flowers, chicory, honey, burdock, potato fruits, yarrow, garlic cloves and others. But they are effective only when inflammatory processes are associated with decreased immunity or a lack of vitamins. If there are other pathogens, it is unlikely that you will be able to get rid of the problem in this way; first undergo a dental examination.
Treatment by a doctor
This is the most adequate method, as it guarantees the correct diagnosis. The doctor will select exactly those medications that will fight not only the symptoms, but also eliminate the preconditions for their return.
How to avoid illness
There are some preventive measures that will preserve the health of not only the oral cavity, but also the entire body:
- regular hand washing, especially before eating;
- annual visit to the dentist;
- balanced diet and avoidance of harmful high-carbohydrate foods;
- selection of suitable dental care products.
In this article, we showed what causes stomatitis in the mouth, the causes of the disease, symptoms and treatment. It depends only on you whether you encounter it or not; a responsible approach will save you from health problems.
Causes of stomatitis
A huge risk of developing stomatitis appears with a decrease in immunity, against the background of which bacterial and infectious infection of the body occurs. Risk factors are also various systemic diseases: gastrointestinal disorders, problems with hormone production, diabetes, anemia.
The immediate causes are:
- bacteria, fungi, mycoplasma, viral infection;
- complications of infectious ENT diseases;
- allergy;
- injuries, burns of the oral cavity (for example, when eating);
- the presence of massive tartar and plaque;
- poor oral hygiene;
- unbalanced diet;
- medications, toothpastes that significantly reduce salivation.