Treatment of pulpitis: stages, methods and means
As a rule, we do not think about the fact that there are nerve endings and blood vessels inside each tooth.
However, acute inflammation can remind you of this at any time. Pulpitis is a pathology that everyone encounters at least once in their lives. The good news is that modern dentistry has proven treatment methods that can solve the problem quickly and effectively. But maybe everything is not so scary and you can just endure the pain?
After all, sometimes you really don’t want to go to the dentist! Let's figure out what processes occur inside the tooth during pulpitis and why a visit to the doctor should not be postponed.
The process of cleaning tooth canals and filling
Cleaning the tooth canals is a complex microsurgical operation, coupled with high-quality filling of the tooth canals, it determines how long the tooth can serve you. At the same time, the operation of cleaning the tooth canals is completely painless and there is no need to be afraid of the procedure itself. The first step to treating tooth roots is diagnosis and radiography. An x-ray allows you to see the shape of the root canal and determine if there are any signs of infection in the surrounding tissue.
Next, to isolate the tooth from saliva during treatment, a rubber dam (rubber film) is placed around the tooth. Now you can conveniently create access to the pulp chamber. It is unlikely that the cleaning of the tooth canals itself needs to be described in detail; in short, it is the removal of dead tissue and deep antiseptic treatment of the cavity of the tooth roots. We repeat - it is painless.
Once the tooth is thoroughly cleaned, it is sealed. If the tooth is not neglected, then the entire treatment will take just one visit. However, if an infection is detected, you have to put in medicine and cover it with a temporary filling for a period of 2 to 4 weeks. You can’t walk around with a temporary filling anymore, there is a high risk of re-infection!
A temporary filling is placed for a period of 2 to 4 weeks, but staying with a temporary filling for more than this period is highly not recommended (unless it is prescribed by a doctor)!
The medicine that is placed under the filling may vary. Moreover, it could be arsenic! But they may not give you a temporary filling. These are all old treatment methods, which, unfortunately, are still used in many regional dentistry or by old-school doctors. In any case, the doctor knows how it works and you need to follow all his recommendations. This means that they very often ask: “What could they give me?” and “how long should I go with this?”, and “did my doctor forget something?”, etc., etc. A third-party doctor and the Internet have no answers to these questions!
Only your doctor knows what medicine he put in the tooth! Any canal treatment method, even an outdated one, can take place and be effective if you follow the recommendations, treatment plan and stay in touch with your doctor.
At the final stage, the tooth canals are filled. For this, gutta-percha (special resins) with a sealer (filler) is most often used. The culmination of tooth canal filling is a control x-ray of the tooth.
Processes in an open and untreated tooth occur very quickly, and you can get complications or even lose the tooth.
If you have lost contact with your doctor or are worried about your feelings and doubts about your current treatment, then the best solution would be to contact your dentist as soon as possible for control and a second opinion.
General characteristics of the disease
Pulpitis is an inflammation of the dental nerve (pulp), which is located in the dental cavity and root canals. The pulp is extremely sensitive, and if a tooth is deeply damaged by caries, there is a crack in it, or a filling has fallen out of it, then the likelihood of developing pulpitis is quite high. Inflammation can also occur during treatment or preparation for dental surgery if the doctor is not careful enough. In rare cases, a previous infectious disease becomes a provoking factor.
Pain can occur when the tooth is exposed to cold or heat, sour foods, alcohol, or sugar. If you see a doctor right away, the inflammation can be suppressed. However, patients often try to relieve pain with analgesics, wasting precious time. As a result, nerve damage becomes irreversible and the pulp must be removed. The danger of pulpitis is that without treatment, inflammation can spread to the tooth root, which increases the risk of tooth loss. Sometimes the pain goes away spontaneously, but this is not an indicator of recovery. This situation may indicate that the nerve is irreversibly damaged by harmful bacteria and a purulent mass begins to form in the tooth cavity. The latter, if it gets into the base of the tooth root, can cause gumboil - a purulent lesion of the jaw.
If the inflammatory process has been causing you discomfort for a long time, you should not delay going to the doctor: removing the nerve in time will help avoid complications. Of course, there is a psychological factor: many patients do not like going to the dentist, are afraid of pain, and do not want to waste time and money. It is important to make a sound decision here so as not to aggravate the situation, especially since modern dentistry is accessible and practically painless.
How to treat pulpitis: modern approaches and methods
Treatment of pulpitis involves eliminating inflammation. This can be done in two ways: either by performing healing and restorative procedures on the pulp, or by completely removing it. The choice of doctor will depend on the condition of the pulp and the stage of inflammation.
Conservative treatment of pulpitis (biological method)
If the patient consults a doctor immediately after the onset of acute pain, it is possible to stop the inflammation while preserving the nerve. The pulp is exposed, treated with an antibacterial drug, a micro-bandage with calcium hydroxide is applied on top and the hole is closed with a temporary filling. After a few days, an x-ray is taken, the condition of the pulp is assessed and, if the inflammation has stopped, a permanent filling is placed. It must be borne in mind that this method is not always applicable and requires a highly qualified doctor, so conservative treatment will not be offered to you in every dental clinic.
Surgical treatment of pulpitis
A traditional method that has different implementation options depending on the specific case and the age of the patient. Consists of complete or partial extraction of pulp from the tooth cavity.
• Extirpation. Used in the vast majority of cases. Represents complete removal of the pulp.
- Vital. Under anesthesia, living pulp tissue is removed. First, the dental tissue affected by caries is removed, treated with an antiseptic, then the infected nerve is removed and the cavity is filled. The procedure requires just one visit to the dentist; it is universal for any form of pulpitis, but is not applicable for patients with allergies to anesthetics.
- Devital. If it is not possible to carry out vital extirpation, the pulp is exposed to paste-like toxic substances (for example, arsenic) so that it can then be painlessly removed. The paste is applied for 24–48 hours, if the patient can come for a second appointment quickly enough, or for up to 14 days - in this case, mildly acting formulations are used. The cavity is closed with a temporary filling until the next procedure. At the second appointment, the doctor removes the dead pulp, cleans the canals and places a permanent filling. For purulent pulpitis or tissue necrosis, the method is not used.
• Amputation. In this case, only the coronal part of the pulp is removed, the root part remains in place. For teeth with one root, amputation is not suitable, since in this case it is almost impossible to isolate individual elements of the pulp. Amputation is usually prescribed for acute pulpitis or accidental mechanical damage to a tooth.
- Vital. The necessary part of the nerve is amputated under anesthesia in one procedure. The method is indicated for patients under the age of 45 with healthy periodontium.
- Devital. After exposing the pulp to a toxic paste, the dead area is removed, and the healthy one is deliberately mummified, for example, with an antiseptic paste based on zinc oxide-eugenol, so that the infection cannot develop again. Devital amputation is used in difficult cases when it is impossible to reach the desired area of the pulp. The modern arsenal of dentists includes flexible nickel and titanium instruments. With their help, you can treat even the most curved canals, which eliminates the need for complex techniques.
Read also: How wisdom teeth hurt, symptoms
The use of arsenic to treat pulpitis was proposed only at the end of the 19th century. Before this, the inflamed pulp was destroyed with hot oil or burned with a hot iron. These methods were used by ancient Greek and ancient Egyptian dentists.
Stages of pulpitis treatment
Let us dwell in more detail on the extirpation method - as the most common and longest-lasting. The procedure requires two to three visits to the doctor, depending on the number of roots of the diseased tooth.
- Removal of tissue affected by caries. The tooth is cleaned, opened and the pulp chamber is exposed. With the devital treatment option, arsenic is placed in the tooth cavity, a temporary filling is placed and a date for the next appointment is set. If the pulp can be removed immediately, treatment begins with the next stage.
- Pulp removal. A special pulp extractor is used.
- X-ray. An image is necessary to determine the length and shape of the canals.
- Cleaning the canals and the tooth in general. This stage is necessary to exclude new inflammation.
- Installation of a seal. First, the canals are filled, then the coronal part.
The last stage can be completed in two visits. In some cases, anti-inflammatory drug therapy is prescribed.
After installing a filling, so-called post-filling pain when biting is possible. It is considered normal unless it lasts more than a week. Some dentists consider it unacceptable. She shouldn't be strong anyway. If you experience serious discomfort, you should further consult your doctor.
Features of treatment of different forms of dental nerve damage
In the modern classification, pulpitis is divided into acute and chronic. In each of the two forms it is easy to identify characteristic stages.
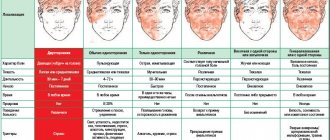
• Acute pulpitis . One of the most common complications of deep caries. It manifests itself as severe pain, which can intensify with pressure on the tooth, exposure to heat or cold, sour or spicy food. Attacks of pain often occur at night. In children, due to the peculiarities of the jaw structure, acute pulpitis practically does not occur; in adulthood, men and women are equally susceptible to it. The disease occurs in two stages, after which, in the absence of treatment, it becomes chronic.
- Focal. The initial stage lasts up to 2 days. The inflammatory focus is located close to the carious cavity. The pain is sharp, “shooting” in nature, attacks last for 10–30 minutes with breaks of several hours. At this stage, it is not difficult to identify a diseased tooth, since the pain is point-like.
- Diffuse. The second stage, which occurs when the coronal and root parts of the pulp are damaged. The pain is diffuse, radiating to different parts of the jaw, the temporal and occipital parts of the head, and cheekbones. The attacks are longer, and the pauses between them are only 30–40 minutes. Acute diffuse pulpitis lasts no more than 2 weeks. If during this time the patient does not see a doctor, the disease becomes chronic.
• Chronic pulpitis. It can last, without disturbing the patient too much, for up to several years. Toothache is significantly dulled, you can get used to it, although chewing is difficult, and with external influences the pain intensifies. Exacerbations are possible from time to time. The treatment method depends on the type of chronic pulpitis.
- Fibrous. It is characterized by the presence of a deep carious cavity, which does not always reach the pulp chamber. The pain is mild, intensifies only when pressing on the tooth, and blood appears from time to time.
- Gangrenous. If an infection is added to fibrous pulpitis, the pulp atrophies, becomes dirty gray, the pain intensifies, and the carious cavity expands. There is a smell from the mouth.
- Hypertrophic. It is characterized by the fusion of a carious cavity with a tooth cavity and the formation of a polyp from granulation tissue, which bleeds and hurts when pressed. But there is usually no pain.
- Exacerbation of chronic pulpitis. Simultaneous manifestation of signs of acute and chronic pulpitis. The patient experiences attacks of sharp pain, which intensifies when pressing on the tooth. Possible destruction of bone tissue and periodontal infection.
Most often, patients with fibrous chronic pulpitis turn to dentists. Gangrenous is less common, and hypertrophic is in last place. If pulpitis has become chronic, surgical treatment is required in 90% of cases. Acute forms can also be treated with conservative therapy. In any case, you will need a reliable clinic, where they will not only expertly carry out the procedure for restoring or removing the pulp, but also install a high-quality permanent filling. Losing a filling can cause damage and pulpitis to adjacent teeth.
How to choose a reliable dental clinic?
Many patients, under the influence of acute pain, choose a clinic spontaneously, and then continue to go there for years, without thinking about the quality of the services provided. Of course, there is no time to search and compare data in such a situation. We asked a representative of the Dental Association to comment on this problem:
“Of course, if you have acute pain, you can go to your nearest dentist, this is a natural solution. However, try to pay attention to the following details:
- Dialogue with the doctor - the dentist should ask you in detail about your feelings, check the tooth’s reaction to various influences. Next, the patient is informed about possible treatment methods.
- A clear treatment plan - after talking with your doctor, you should understand how many procedures will be required, at what interval and why.
- The possibility of an unscheduled appointment - in the event of a sudden complication, you should be seen at a time convenient for you.
If you don’t like something, you can go through the next stages of treatment in another clinic, which you choose in a calm state, when the pain has passed.
Our Association has opened a hotline for dental treatment issues. 24 hours a day, seven days a week, specialists from various fields of dentistry will consult you free of charge by phone, tell you about a possible treatment plan, and suggest a particular clinic. When receiving treatment from the Association, guarantees are given for materials and services provided, and competitive prices are offered. Our dentists have extensive experience in therapy and surgery of various forms and stages of pulpitis, and you can be sure that after treatment the tooth will not cause you any trouble.”
PS The website of the Dental Association presents prices for all-inclusive treatment, which will allow you to avoid unexpected expenses during treatment.
Read also: Resection of the apex of the tooth root
License No. LO-77-01-014630 dated August 3, 2020, issued by the Moscow Department of Health.
How is tooth pulpitis treated?
Tooth pulpitis is treated in two main ways - biological and surgical. The method of therapy is selected depending on the severity of the symptoms, the type of pathology, as well as the progression of the inflammatory process. Treatment is prescribed based on the results of the preliminary examination. The specialist always faces the task of saving the patient from unpleasant sensations and, if possible, preserving the damaged tooth, so everything will depend on the situation.
How do dentists treat the disease?
It is advisable to begin treatment of pulpitis in a timely manner, as this can lead to negative consequences and certain complications, for example, periodontitis. Dentists immediately try to relieve the patient of pain, inflammation, eliminate the infection and gradually restore the functionality of the pulp, if possible.
As soon as a patient with acute pulpitis sees a specialist, an anesthetic is injected into the carious cavity, and an analgesic is taken orally. After a thorough examination of the oral cavity, a treatment method is selected - conservative or surgical.
Conservative treatment - helps to get rid of pain, inflammation with the help of medications and physiological methods of therapy that are aimed at preserving the pulp. In such a situation, a biological method is used. Sometimes the patient undergoes partial removal of the pulp, but its viability remains.
Conservative treatment is considered a one-session treatment in most cases, but it may take several days to resolve the problem. There are such indications for the biological method of therapy as focal pulpitis in the acute stage, exposure of the pulp when the dental crown is broken, chronic fibrous pulpitis, the patient’s age is not more than 29 years, no changes in the area of the apical foramen, there is no possibility of prosthetics, and others.
Conservative therapy includes the following steps:
- Anesthesia.
- Treatment of carious cavity with instruments and medications.
- Degreasing procedures, drying the cavity.
- Applying an insulating gasket to the bottom of the pulp and installing a filling.
It is possible and advisable to treat pulpitis surgically only if conservative treatment is impossible. It involves removing the pulp completely, then filling the canals and, accordingly, the dental crown. This method of therapy is considered the most reliable and is carried out in several visits to a specialist:
- Use of anesthesia.
- Removal of carious tissue from the cavity.
- Protecting the tooth from moisture using a rubber dam.
- Removing pulp from the crown and canals.
- Measuring the length of canals, their processing, expansion and filling.
- Rinsing the canals with antiseptics, applying an antiseptic, then placing a temporary filling.
- Removal of temporary filling and preparation from the canals.
- Rinsing the canals and drying them.
- Filling canals with gutta-percha.
- X-ray examination, which helps to track the correctness of the canal filling.
- Installation of a permanent filling.
How long does it take for treatment?
How long does it take to treat the disease to get a positive result from therapy? In this situation, everything will depend on many factors. First of all, attention is paid to the stage of the disease and the inflammatory process. The general condition of the patient and other severe symptoms must also be taken into account. Do not forget about the destructive process and the possibility of restoring a damaged tooth.
If it is possible to leave the pulp and not remove the tooth, then a conservative treatment method is used, which includes several visits to the dental office. If a patient is diagnosed with an advanced stage of pulpitis, it is recommended to undergo surgical treatment, which also involves several visits to a specialist.
Why do they place a temporary filling for pulpitis?
Temporary filling is recommended for conservative treatment of pulpitis and caries. It is installed in order to prevent the leakage of the anti-inflammatory drug from the root canal, as well as to prevent the entry of pathogenic microflora and pieces of food.
What medicine is put into the tooth for pulpitis?
It is impossible to treat tooth pulpitis without the use of various drugs. The medicine is placed under the filling to eliminate the infection and inflammatory process.
Various anti-inflammatory drugs may be used. Very often, arsenic is placed in the tooth to kill the nerve and numb the problem area.
The fourth reason is the individual reaction of the body
The reason is rare, but do not forget that each person is individual. A long-term or acute painful reaction can occur both to arsenic anhydride itself and to the auxiliary components included in the paste. Most often, pain occurs due to a lowered pain threshold and the patient’s tendency to allergic reactions.
Pain may occur due to allergies and individual intolerances
“Once in my youth I had pulpitis, the doctor put medicine inside to kill the nerve and didn’t even say whether the tooth with arsenic should hurt. He told me to come for an appointment only in a few days. There was no Internet back then, and we took the doctors’ word for it. I came home in blissful ignorance, and after about two hours the pain began to be so severe that I wanted to climb the wall. Analgin did not help to remove it, so the next day I ran back to the hospital begging them to do something. And the doctor looked at me in such surprise, saying, I’m kind of wild, and he almost pushed me out of the office, saying, I have to walk for another day. But it turns out that there were only flowers at home - the berries started at the follow-up appointment. The pain not only did not go away, but became even stronger than before. I don’t know how I survived that day. Since then I’ve been trying not to let my teeth get into trouble like that, because... the thought of pulpitis causes terrible experiences.”
Arsenic paste for nerve death
Treatment for some dental diseases requires removal of the nerve. This is pulpitis, severe tooth decay, periodontitis, a cyst, and also the nerve is deadened before permanent prosthetics.
This procedure can be carried out in one visit to the dentist, or first, medicine is placed in the tooth, a temporary filling is placed, and after a few days the dead nerve is removed from the organ cavity.
The medicine can be an arsenic-free paste or with arsenic.
Previously, the nerve was killed only with arsenic, but now this treatment has shown many disadvantages. After arsenic has been placed in a tooth, it may hurt, and its untimely removal leads to a toxic effect on the surrounding tooth tissue.
Read also: Tooth under crown reacts to heat
Correct treatment eliminates any complications, but we will still look at why arsenic is placed in the tooth cavity, and what complications may follow, in particular, when the tooth hurts after treatment.
Why treat a dental canal?
The main method of treating tooth canals is to remove the infected pulp. This has to be done because after the death of the pulp, bacteria begin to multiply in the tooth cavity. Bacteria and their breakdown products can lead to infection and cause the formation of granulomas on the root of the tooth.
A granuloma (cyst) is a pus-filled pocket that forms at the end of a tooth root. In addition to granuloma, infection at the root of the tooth can cause:
- Swelling that may spread to other areas of the face, neck or head.
— Loss of bone tissue around the tip of the tooth root.
- Fistula or fistula (a channel that allows pus to escape through the gum or cheek).
- Death. Yes, people still die from this, even in the 21st century...
We are writing this not to suppress your appetite or to scare you, but only so that you do not push the disease to its extreme and we do not encounter such consequences in our work.
Why arsenic in dentistry
The use of arsenic is not very common now; modern treatment is carried out with arsenic-free pastes that contain an analgesic. After this paste is applied to the nerve, it should remain for several days. Throughout this period, the crown does not hurt, the nerve gradually dies, then it is also painlessly removed.
In case of severe carious destruction of the crown or in cases of pulpitis, the dentist will perform depulpation.
The dental nerve will be removed with arsenic in the following cases:
- contraindications to anesthesia, allergies to painkillers;
- characteristics of the body when existing anesthetics do not work;
- emergency dental treatment.
Arsenic cannot be used for treatment in the following cases:
- age up to 2 years;
- arsenic intolerance;
- poor access to the dental cavity;
- root disconnection;
- increased intraocular pressure;
- tooth root disease;
- systemic diseases of the genitourinary system.
Paste with or without arsenic is used only when pain relief cannot be performed. As soon as arsenic is added and a temporary filling is placed, the dental nerve begins to gradually die, causing the organ to hurt for some time, it may be painful to press on it and it reacts to temperature stimuli. After applying the arsenic paste, it should remain in the tooth for 24 to 48 hours.
If for some reason you cannot visit the dentist after the specified time to remove the nerve, complications may arise, even to the point where you will have to have the crown removed. To prevent this, you need to properly plan the treatment and do everything according to the dentist’s instructions.
Why does pain occur?
There are many reasons why a tooth may hurt under a temporary filling. In fact, there is nothing strange in this phenomenon, since the treatment has not yet been completed, the disease has not yet been completely eliminated, and, accordingly, its course is associated with a number of uncomfortable sensations.
True, the fact that a tooth with a temporary filling hurts is also explained by pathological factors. For example, during dental procedures, the doctor could make certain mistakes, the consequences of which led to acute pain syndrome. Partial removal of a nerve is a common factor that causes pain after filling.
So, if the root cause of the problem is not the disease itself, then the tooth hurts when pressed after installing a temporary filling for the following reasons:
Tooth pain after nerve removal
- during filling, the composite material went beyond the root apex;
- pain is a kind of “protective” reaction of the tooth to the presence of a foreign body;
- perforation of the tooth root;
- the nerve was not completely removed;
- an allergic reaction to the material from which the temporary filling is made;
- displacement, breakage, loss of “protection”;
- failure by the patient to comply with the recommendations given by the dentist after installing the composite.
After removal of nerve endings (for example, during pulpitis), small natural holes remain in the roots of the tooth. In most cases, the doctor covers them with special gutta-percha pins, but if this step was skipped, the filling material “leaves” the root and enters the oral mucosa. The body “interprets” the composite as a foreign body and begins to actively fight it—toothaches occur.
Damage to the integrity of the composite due to the patient’s negligence also leads to pain.
During dental procedures, if safety rules are not followed, elements of instruments may remain inside the canal. The same applies to consumables (cotton wool, medicines). As a result of the described actions, an active inflammatory process accompanied by pain develops at the site where the temporary filling is installed.
The sharp needle-like objects used to remove nerves can puncture the root of the tooth - this happens almost unnoticed by both the dentist and the patient. The pain syndrome manifests itself after the anesthesia has worn off (soft tissues richly penetrated with nerve endings are also affected).
The most common indication for temporary filling is the treatment of pulpitis. The most common mistake in this case is incomplete removal of the nerve of the “damaged” tooth. The fact is that nerve endings can be branched and have a considerable length, so it is not always possible to extract them in one go. So, if after a temporary filling a patient’s tooth begins to hurt badly after a day or two, this is a reason to check whether all the nerve endings have been removed.
An allergic reaction to the components of the supplied composite composition (or to pastes with arsenic, which are placed inside the tooth during temporary filling) is also a common occurrence. The main symptoms are severe hyperemia and swelling (compression of nerve endings). The solution to the problem is simple - one temporary filling is replaced by another.
It is strictly forbidden to touch the filling with your tongue or touch it with your fingers - this can lead to its damage or even loss. Sometimes, to answer the question why a tooth hurts under a temporary filling, it is enough to check its integrity.
Why does a tooth hurt?
There are no unpleasant sensations during the procedure itself, but there are exceptions. In the case when treatment is carried out without anesthesia, the dental nerve hurts greatly. In dentistry, of course, not pure arsenic is used; the nerve is killed with a multicomponent paste. After the medicine is administered, the organ should not hurt much, since the paste contains an anesthetic substance.
In addition to arsenic, medications contain:
- antiseptic to neutralize pathogenic microflora and disinfect necrosis;
- anesthetic to relieve pain during nerve necrosis;
- an astringent to prolong the action of the paste and slow down the penetration of arsenic into soft tissues.
Representatives of such pastes with arsenic anhydride are Septodent, Kaustinerv, Pulparsen.
My tooth hurts with medicine, what should I do?
I went to the dentist today, he did not treat my tooth, he said that he needed a picture of the tooth and put me on medicine or arsenic for a while. I didn’t drill anything, I just laid it down and sent for a photo. After the doctor, I came home, and after a few hours the tooth began to hurt.
What should I do - endure it or pick out the medicine?
Picking it out will not solve the problem, since the nerve is alive and already open. Most likely, the arsenic is not located quite correctly. In any case, the tooth must be depulped, since the pain will not go away or will go away for a short time, but the dynamics will intensify.
Read also: Arsenic color
Contact phone number
Consequences of devitalization
Arsenic is a strong toxin and most often leads to complications. The tooth may hurt and the surrounding tissues may become inflamed if the dose is not calculated and more paste is applied than necessary.
After the medicine is placed, the crown hurts for the following reasons:
- inflammation of periodontal tissues or drug-induced periodontitis - in this case, it is painful to press on the crown, swelling of the surrounding tissues occurs and you will need to clean the canals, followed by filling and treatment of soft tissues;
- swelling of the nerve bundle – it may be painful to press on the crown due to the fact that a highly concentrated paste was applied for a long time;
- osteonecrosis is a serious consequence of pulp removal using arsenic paste, when bone tissue becomes necrotic, the jaw hurts, it is painful to press on the tooth and urgent treatment is required;
- intoxication of the body is the most complex consequence, which occurs a few days after the medicine is put in, it becomes painful to press the crown, but the main symptoms relate to poisoning of the whole body;
- blackening of dentin - with this complication it can be painful while chewing, the crown reacts to temperature stimuli, changes in color, black dentin is visible through the enamel.
If complications arise, when the organ hurts and changes color, it is necessary to wash the canals, symptomatic treatment and root filling.
The second reason is leakage of the temporary filling and burn of the mucous membrane
As mentioned earlier, the pain usually goes away after a few days. However, if you have been diagnosed with arsenic, and the tooth hurts unbearably, the pain occurs after some time, or first went away and then returned, then you need to be wary.
First, conduct a visual examination of the oral cavity. Perhaps the doctor did not install the temporary filling hermetically or its integrity was damaged (for example, you started eating earlier than 2 hours after visiting a specialist and did not allow the materials to harden). If the protective barrier is depressurized, particles of the drug can enter the oral cavity, causing a burn to the mucous membrane and surrounding soft tissues. During a visual examination, hyperemia of the mucous membrane and its redness will also be noticeable.
One of the causes of discomfort may be a burn to the oral mucosa
In such a situation, you need to thoroughly rinse your mouth with an antiseptic, close the opened cavity with a cotton swab and visit a doctor as soon as possible. Remember that you should not remove arsenic from the tooth yourself, because... this may make the situation worse. Next, to treat the wound, it will be necessary to use products that promote rapid restoration and tissue regeneration - vitamin A, rosehip or sea buckthorn oil.
Remember that leaving the paste on the gums for too long can lead not only to burns, but also to tissue necrosis. From an open cavity, arsenic can enter the stomach, which will lead to gastrointestinal upset and the appearance of symptoms of intoxication of the body: a metallic taste in the mouth, abdominal pain, nausea and headache.