Orthodontist-dentist Nikolaeva Nadezhda Nikolaevna
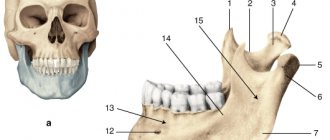
The temporomandibular joint (TMJ) is a paired joint formed by the head of the mandible, the mandibular fossa and the articular tubercle of the temporal bone.
The heads of the mandible meet at an obtuse angle at the anterior edge of the foramen magnum. The TMJ ensures the movement of the lower jaw and represents a complex activity of the body in the form of chewing, swallowing, talking, yawning. The muscles of mastication ensure precise movement of the joint in an error-free manner, unless there is dysfunction (TMJ dysfunction). According to WHO, about 40% of the population aged 20-50 years suffer from TMJ dysfunction. But not every person seeks help from a gnathologist or osteopath with complaints about the joint, preferring to visit other doctors with headaches, fatigue, attacks of fear, pressure... Dysfunction manifests itself in the form of a neurological clinic: headache, dizziness, clicking and crunching joint, muscle tension, spasms in the head, neck, throat. Otology clinic: noise, ringing, ear congestion, hearing loss. But there are other, hidden and long-term consequences of TMJ dysfunction:
- Cervical lordosis. Poor posture, when the neck is excessively straightened or, on the contrary, the head protrudes noticeably relative to the person’s body.
- Curvature in the sacroiliac joint (pelvic bones) as a result, a change in the length of the limbs.
With pain and dizziness, it would seem clear: head, ear, joint. Everything is close, everything interacts. But what effect does TMJ have on the entire musculoskeletal system, especially on the length of the limbs?
The TMJ is the structure of one complex - the DENTAL GNOSTIC system. The dental system is a complex of interactions between the structures and functions of the head and neck. Includes components of the bones of the skull, lower jaw, hyoid bone, clavicle and sternum, muscles and ligaments, joints, vascular, lymphatic and nervous systems, as well as soft tissues of the head and teeth. In addition, it has a connection with the sacrum and coccyx through the dura mater. Everything in the system is interconnected and depends on the normal functioning of all its parts.*
Main functions of the dental system:
- Providing basic body functions: chewing, swallowing, biting, speaking, breathing.
- Participation in maintaining statics: gait mechanism, cervical, vertebral and muscle balance, pelvic balance, equilibrium.
- Effect on cranial (cranial) function - especially the temporal bone.
- Influence on the functions of the nervous, endocrine, lymphatic systems.
Let's look at the basic functions of the body: chewing, swallowing, speaking, breathing. These basic body functions are performed through the movement of the lower jaw. The movement of the lower jaw is ensured by the movement of the head of the lower jaw in the articular fossa of the TMJ, with the help of the temporal, masticatory, pterygoid, hypoglossal and other muscles. The line of closure of the teeth - the occlusal plane, or simply the bite, should normally be parallel to the planes of the entire musculoskeletal system. The main planes of which pass through the pupils, the line of closure of the teeth, the second and third cervical vertebrae, shoulder blades, iliac crests, knees and ankles. The parallelism of the lines indicates the health of the musculoskeletal system and the dental system. A change in any of the planes leads to changes in the other planes. Therefore, a violation of the occlusal plane relative to others can cause pain and negative changes in completely unexpected parts of the body.
Violations of occlusion as a result of tooth wear, congenital malocclusion, and more often, inadequate dental treatment or prosthetics, inept use of braces, illegal removal of healthy teeth, lead to response disorders in the cervical spine and spasm of the muscles of the back of the neck. Prolonged spasm causes structural changes in the muscle, shortening it and causing it to lose its ability to contract and relax. Muscle spasm leads to spasm of the chewing and facial muscles. Thus, for the body, muscle spasm on one side is a pathological process that leads to spasm in another area. For example, the temporal muscle is involved in supporting statics; the masticatory muscles are its synergist. These muscles contain a large number of proprioceptors (sensory fibers). A constant flow of nerve impulses from proprioceptors is involved in the regulation of the vertical position of the body. Violation of occlusion (bite) leads to unbalanced movement of the lower jaw and maxillofacial muscles, incl. masticatory and temporal muscles. A change in the flow of nerve impulses, due to dysfunction of the TMJ, causes curvature of the spine in the cervical region and sacroiliac joint, which leads to twisting of the pelvis and changes in the length of the limbs.
An imbalance in the TMJ sends a negative stimulus to the nervous system 24 hours a day, 7 days a week. Any malocclusion changes the direction of force in the skull. For example, premature contact on the lateral teeth causes uncoordinated muscle movement and distortion of nerve impulse transmission to the brain. Uncoordinated muscle movements often cause tension in the fascia of the neck. The nodes of the sympathetic trunk of the autonomic nervous system lie anterior to the prevertebral fascia of the neck. Thus, dysfunction of the TMJ, causing tension in the fascia of the neck, can irritate cervical sympathetic communications, provoking a reflex spasm of the vessels of the head. Spasm of the blood vessels in the head causes a disturbance in the blood supply to the cerebellum, which is manifested by a lack of coordination, dizziness - as a result of anxiety. TMJ dysfunction causes torsion (torsio; Latin “rotation, twisting”) of the temporal bone, in which the labyrinth with the vestibular apparatus is located. Changes in the vestibular system lead to imbalance and dizziness. Nasal congestion may also be associated with TMJ dysfunction. Due to the shortening of the fascia of the neck muscles, there is a violation of lymphatic drainage and the outflow of venous blood from the head. This may manifest itself in the form of tissue edema in the area of the nasal passages, since this area is rich in blood vessels. Diseases of the temporomandibular joint have the following causes:
- Malocclusion (occlusion) is a closure of the teeth, which disrupts the shape and function of the dental system. This manifests itself in the form of deformation of the occlusal surface of the teeth with blockade of the movement of the lower jaw. Which can lead to pathological wear of teeth, functional overload of the TMJ and chewing muscles. The most common TMJ problem is a decrease in bite height. This is due to several factors: impaired teething, bruxism, premature loss of milk or permanent teeth, congenital absence of a group of teeth, microdontia (small teeth), pathological abrasion of enamel, violation of the vertical size of teeth due to the work of the dentist. Changes in the position of the TMJ due to illiterate orthodontic treatment, illegal or forced removal, tooth decay.
- Stress (overexertion, strong clenching of teeth).
- Jaw trauma (fractures of facial bones and jaw).
- Endocrine, metabolic disorders, infectious diseases.
- Excessive physical activity.
- Bad habits (biting nails, holding the phone incorrectly, etc.)
Symptoms of temporomandibular joint diseases:
- Headache, spasms in the facial muscles and jaw area.
- Clicking, crunching, grinding when the jaw moves.
- Pain, congestion and ringing in the ears.
- Enlarged submandibular lymph nodes.
- Dizziness.
The impact of TMJ diseases on human health has not been studied, in contrast to the methods of diagnosis, treatment and restoration of TMJ by a gnathologist. In most cases, a transparent corrective aligner is enough to save yourself from many present and future health problems.
With dysfunction of the temporomandibular joint, a violation of its coordinated activity occurs as a result of changes in the closure of the jaws, the location of its elements and muscle function. According to experts, about 3/4 of patients suffer from this disease, which is difficult to diagnose and treat. Ignoring the symptoms of pathology is extremely dangerous, since dysfunction of the temporomandibular joint in an advanced form can provoke the development of serious illnesses. To prevent undesirable consequences, you need to be able to identify signs of pathology and eliminate them in a timely manner.
Causes of dysfunction of the temporomandibular joint
The appearance of temporomandibular joint dysfunction (TMJ) can be caused by a large number of factors. Most often, the disease occurs for the following reasons:
- stress;
- malocclusion;
- excessive tension of the masticatory muscles when chewing too hard food;
- pathological abrasion of tooth enamel;
- intense physical activity associated with overstrain of a certain muscle group;
- unsatisfactory quality of dental intervention during the installation of fillings or dentures;
- damage to the lower jaw.
Often, it is medical errors that lead to the development of TMJ pain dysfunction syndrome. For example, a crown or filling that is too high provokes an asymmetrical position of the jaw, as a result of which the load on it becomes uneven and, over time, leads to a malfunction of its functioning.
Types and degrees of disease
There are two forms of the disease depending on the origin: primary and secondary. The primary form of degenerative arthropathy is generalized, which means multiple joint damage. The secondary type of disease is associated with a previous injury or illness. The lesion is monoarticular. Doctors distinguish 4 degrees of development of degenerative-dystrophic pathology:
- In the first degree, there is slight instability in the joint.
- At the second stage of the pathology, more pronounced changes appear, the symptoms become stronger, accompanied by sclerosis and ossification of the condylar process of the mandible.
- The third degree is characterized by the beginning degeneration of cartilage tissue, osteophytes and flattening of the articular fossa appear.
- The last degree is the fourth, with which fibrous tissue begins to grow.
Osteoarthritis of the maxillofacial joint is distinguished by its course. Acute and chronic course occurs with this disease. In medical practice, two more types of disease are distinguished: sclerosing and deforming. In the first type, sclerosis of the cortical plates of the articular bone surfaces is noted. The sclerosing type of the disease is characterized by narrowing of the gaps between the joints. The deforming type of degenerative disease is manifested by flattening of the articular fossa, head and tubercle.
Symptoms of TMJ pathology
Pathological disorders of the structure of the joints, including the maxillary and mandibular, can negatively affect the patient’s quality of life. Symptoms of TMJ dysfunction are extensive and manifest as:
- The appearance of clicking sounds in the area of the mandibular joints. This symptom primarily indicates the described disease. Clicking sounds when opening the mouth, yawning or chewing food are loud enough that others can hear them. This phenomenon is not always associated with the presence of pain.
- Headache attacks. Often, painful sensations are localized in the back of the head and temples. Some patients report prolonged unbearable pain, as a result of which experts often mistakenly attribute this symptom to manifestations of brain diseases or migraines.
- Jamming of the temporomandibular joint. When opening the mouth, the uniformity of movement of the lower jaw is disrupted. This phenomenon can be described by a more precise definition - blocking. Often, to eliminate jammed jaws, it is enough to simply move them in different directions or try to open your mouth until a characteristic clicking sound is heard.
- Painful sensations in the ear area. Since the temporomandibular joint is located next to the ears, pain often occurs in them when its function is impaired. Along with this, patients may complain of ear congestion.
- Bite disorders. Malfunction of the temporomandibular joint can lead to changes in the closure of the dentition. This phenomenon is associated with displacement of the discs, when the location of the bones and their joints does not correspond to the anatomical norm.
- Hyperesthesia. Grinding your teeth and clenching your jaw can provoke the development of enamel hypersensitivity. There are often cases when, when a patient complains of severe toothache, the doctor, without suspecting the connection of this symptom with the presence of TMJ dysfunction, resorts to removing or depulping the tooth, which ultimately does not solve the problem.
In some cases, the disease may be accompanied by inflammatory processes, tissue swelling, pain, weakening of the body, malaise and hyperthermia.
Along with these symptoms of dysfunction of the TMJ joint, there are other signs. Among them are:
- pain in the back and shoulder blades;
- attacks of dizziness;
- sleep disorder;
- loss of appetite;
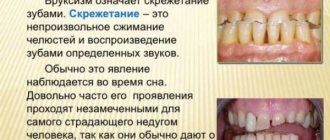
- involuntary grinding of teeth during sleep – bruxism (we recommend reading: why do people grind their teeth at night?);
- snoring and apnea;
- photophobia;
- depressive syndrome;
- dry mouth;
- disorder of the function of swallowing food;
- burning tongue.
If these signs are identified, you need to begin eliminating them as quickly as possible. Due to the characteristics of the described pathology, its treatment requires the joint efforts of specialists in the field of dentistry, neurology, psychology and, in some cases, maxillofacial surgery.
Symptoms
The connection between TMJ dysfunction and hearing pathologies was first discovered by J. Costen in the thirties of the last century. It was he who also described the traditional complex of symptoms of this disease, after which it began to be called Costen syndrome. However, almost a century has passed since those times, and by now the symptomatic description of the disease has expanded and become more detailed. Now there are several groups of characteristic symptoms:
- Difficulty in movement, accompanied by a characteristic “locking”. For example, if a patient tries to open his mouth, he needs to first move his jaw several times and catch the place where the joint opens.
- Noisy phenomena in the ears initiated by the joint. The most characteristic thing is clicking sounds when chewing and opening the mouth, and they are not always accompanied by pain. Sometimes the clicking sound is so loud that it reaches the ears of people nearby. Complaints of popping and crunching sounds may also be heard.
- Painful phenomena in certain places (hyoid muscles, temples, masticatory muscles, neck, ears, teeth and jaws, eyes). Migraine-like pain also occurs.
- Jet lag and eating disorders. Often encountered: photophobia, lack of appetite, snoring and attacks of suffocation during sleep, difficulty falling asleep, dizziness, low mood.
Position of the mandibular joint relative to the face
Diagnostic and treatment methods
The extensive symptoms of the disease significantly complicate its diagnosis, so patients are often observed for a long time by specialists of different specializations - an otolaryngologist, a neurologist, a therapist, and a rheumatologist. If you suspect the described dysfunction, you should contact your dentist.
At the initial examination, the doctor finds out the nature of the patient’s complaints, features of his lifestyle, and the presence of any chronic diseases. Next, the specialist palpates and listens to the joint area, assesses the degree of mouth opening and mobility of the lower jaw.
An obligatory stage of diagnosis is obtaining an occludogram (wax impression of jaw contacts) to assess the closure of the dentition. To determine the condition of the temporomandibular joint, the doctor prescribes the following laboratory tests:
- orthopantomography is a type of radiography that allows you to obtain a detailed image of all teeth and jaws;
- ultrasonography;
- x-ray of the temporomandibular joint;
- computed tomography and magnetic resonance imaging, which allows us to identify the nature of injury to the tissues surrounding the joint;
- Dopplerography or rheoarthrography, on the basis of which indicators of arterial hemodynamics are determined;
- gnathodynamometry - determination of the force of the chewing load when clenching the jaws;
- electroneuromyography – assessment of the peripheral nervous system;
- phonoarthrography - listening to sounds arising in the joints.
After making a final diagnosis, the doctor develops a treatment plan. First of all, the patient is prescribed a special diet, including food that does not require thorough chewing. At this time, it is recommended that the jaws be at maximum rest; for this, speech load should be limited. To relieve pain, the following are used:
- non-steroidal anti-inflammatory drugs;
- antidepressants;
- sedatives.
Along with this, the treatment regimen includes botulinum therapy and intra-articular injections of glucocorticosteroids. To eliminate the symptoms of the pathology, the patient is prescribed a course of physiotherapeutic procedures, which may include:
- myogymnastics (we recommend reading: myogymnastics in orthodontics: exercises to correct the bite);
- massage;
- laser therapy;
- inductothermy;
- electrophoresis;
- ultrasound therapy.
Treatment often includes psychotherapy and biofeedback (neurotherapy), which are aimed at relaxing the muscles of the masticatory group. Dental treatment is based on correcting the bite. If there is no result of conservative treatment, surgical intervention is resorted to.
According to statistics, almost 20% of all visits to the dental clinic are associated with dysfunction of the temporomandibular joint (TMJ). The temporomandibular joint is the point of articulation between the temporal bones of the skull and the heads of the lower jaw. The TMJ is one of the most mobile joints in the human body. Approximately every 60 seconds, that is, when eating, talking, yawning or any other manipulation in which the jaws are involved, the joint begins to move.
TMJ dysfunction is pathological changes in the jaw joint and facial muscles that are involved in all processes associated with jaw movement. In the structure of diseases associated with jaw pathologies, more than 80% is occupied by dysfunction of the temporomandibular joint (Costen syndrome, dysfunction of the lower jaw, TMJ myoarthropathy, etc.).
Treatment of TMJ dysfunction is always complex, since this disease is a multidisciplinary pathology and requires the participation of various specialists. Complex therapy usually includes:
- drug therapy;
- myogymnastics;
- physiotherapy;
- orthodontic, orthopedic and surgical treatment of dysfunction.
If you are looking for the best place in Moscow to get treatment for TMJ dysfunction, contact the Canadian Center for Innovative Dentistry and Neuromuscular Therapy. Experienced specialists will conduct a comprehensive diagnosis, determine the exact cause of the problem and help quickly restore the proper functioning of the muscles and joints of the jaw.
The combination of advanced technologies, deep scientific knowledge and many years of experience in the field of neuromuscular therapy allows our doctors to cope with even the most complex and difficult to diagnose cases in the shortest possible time.
Treatment
Due to the complexity of the syndrome being described, the doctors to whom different patients may be referred overlap only partially. Typically, the treatment of patients with this dysfunction involves:
- Dentists, including dental surgeons and orthodontists.
- Osteopaths - in cases where the pathological process affects bone tissue to a significant extent.
- Neurologists.
- Chiropractors - for certain muscle pathologies.
The patient needs to minimize jaw tension, that is, to abandon inappropriate speech. Those categories of persons whose specific professional activities contradict this will have to temporarily give up their profession.
During therapy, the patient must take care of his lifestyle. He should make up the most balanced diet of soft foods that require little jaw work. To compensate for the lack of microelements, patients take mineral and vitamin complexes.
What is conservative treatment?
Conservative therapy for articular dysfunction includes:
- Pharmacological effects:
- taking non-steroidal anti-inflammatory drugs orally or by injection to relieve symptoms of inflammation;
- the use of steroid hormones that quickly relieve inflammation - if NSAIDs are contraindicated due to erosive damage to the gastrointestinal tract;
- botulinum therapy;
- injections of painkillers and muscle relaxants.
- Dosed exercises for the jaw muscles as prescribed by a doctor.
- Physiotherapeutic procedures (only in the absence of an inflammatory process):
- laser treatment;
- ultrasonic influence;
- electrophoresis with medications.
- Dental treatment, sometimes with preliminary wearing of special splints:
- elimination of overpriced fillings;
- installation of braces;
- repeated or primary prosthetics;
- other types of orthopedics and orthodontics procedures.
- Massage.
- Psychotherapy.
Operation
If, in the opinion of doctors, the listed measures are not effective enough to treat a given patient, he undergoes surgery. The most common types of intervention in this case are removal of the lateral pterygoid muscle, arthroplasty procedures and condylotomy of the articular head of the mandible.
The structure of the maxillotemporal joint
Causes of TMJ dysfunction
The main reasons for the development of dysfunction of the lower jaw include articulatory-occlusal, myogenic and psychogenic disorders:
- malocclusion;
- jaw injuries (including birth injuries);
- dental defects;
- incorrectly performed prosthetics;
- pathological abrasion of teeth;
- various dental anomalies, which are accompanied by a decrease in the height of the alveolar process;
- bruxism;
- chronic microtraumas of the components of the TMJ;
- excessive mechanical load of the masticatory muscles;
- physical and neuropsychic stress, causing disruption of articular kinematics and function of the maxillofacial muscles.
Most researchers believe that the following negative factors underlie functional disorders of the temporomandibular joint:
- changes in the tone of the masticatory muscles;
- violation of occlusion;
- incorrect position of the jaws.
When the temporomandibular joint stops functioning normally, it affects all aspects of a person's daily life. TMJ dysfunction becomes the root cause of constant pain and discomfort (first in the joint area, and then in the neck, shoulders and throughout the spine). If you do not start timely therapy, the condition will only get worse.
Therefore, at the first signs of dysfunction of the temporomandibular joint, you should immediately contact your dentist.
Causes of TMJ arthrosis
Today, doctors identify a number of main reasons that can provoke the appearance and development of arthrosis of the TMJ:
- Infectious infection in one way or another
- Problems with the endocrine system
- Malfunctions of the metabolic system
- Lost one or more teeth
- Jaw injuries
- Inflammation where joints meet
As a rule, arthrosis of the TMJ occurs when several factors from this list are combined, but sometimes it can occur only against the background of one, for example, inflammation or injury. Also, the occurrence of TMJ arthrosis is influenced by poor nutrition, especially food with an abundance of chemical flavors and preservatives.
Symptoms of muscle-joint dysfunction
Temporomandibular joint dysfunction is quite difficult to diagnose, since the clinical symptoms are similar to those of many other diseases. Experts consider the following group of symptoms to be diagnostic criteria for muscular-articular dysfunction:
- sound phenomena in the TMJ area - crunching, clicking, popping in the joint that appears when chewing, opening the mouth, yawning and any movement of the jaw;
- blocking of the temporomandibular joint - restriction of joint movements when opening the mouth (to open the mouth wide, you first have to move the jaw from side to side);
- pain syndrome – pain of a different nature in the area of the jaw joint, face, shoulders and neck, in the ear area when chewing, opening the mouth wide, talking;
- difficulty chewing;
- swelling of the face on one side;
- dizziness, hearing loss, ringing in the ears, sleep disturbance, etc.
The symptom complex of TMJ dysfunction is very similar to the clinical signs of cervical osteochondrosis, trigeminal neuralgia, otitis media and many other diseases. The variety of symptoms and their similarity to other pathological conditions make diagnosing the disease difficult. This is why many patients first turn to an otolaryngologist, therapist, neurologist or other specialized specialists and do not receive adequate treatment.
TMJ dysfunction requires a comprehensive examination and differential diagnosis. There is no need to steadfastly endure the pain caused by muscle-joint dysfunction, perceiving it as something inevitable. Come for a consultation with specialists from the Canadian Center for Innovative Dentistry and Neuromuscular Therapy, who will quickly conduct a comprehensive examination, determine the nature of the discomfort and prescribe adequate therapy.
Mechanism of disease development
The whole essence of the pathological process comes down to the natural processes of malnutrition of the joint, which leads to its regular traumatization, reduces the ability to regenerate and resist damage. Along with the articular cartilage, the ligamentous apparatus along with the muscles are also affected.
There are quite a lot of trigger factors for the development of this complex joint disease. They include long-acting predisposing factors in which regenerative processes and normal tissue nutrition decrease over time, triggering a chain of irreversible reactions that cause arthrosis of the jaw with its characteristic symptoms, which requires immediate treatment.
The main reasons for the development of arthrosis of the TMJ:
- Injuries;
- Congenital disorders of maxillofacial proportions;
- Long-term or frequent arthritis (direct inflammation of the temporomandibular joint);
- Bite disorders;
- Low quality dentures;
- Complete or partial absence of teeth;
- Maxillofacial surgical interventions;
- Changes in hormonal levels during menopause;
- Genetic predisposition;
- Other arthrosis;
- Long-term open mouth (frequent visits to the dentist, prosthetics);
- Poor quality dental fillings, leading to asymmetry in the functioning of the joint;
- Bruxism is the unconscious grinding of teeth at night, leading to the gradual wearing away of tooth enamel.
Diagnostics
Symptoms of temporomandibular joint dysfunction may resemble the clinical manifestations of many other pathologies (diseases of the paranasal sinuses or teeth, arthritis, inflammatory gum disease, etc.), so the dentist carefully examines the medical history and conducts a comprehensive clinical examination to accurately determine the cause of the patient’s symptoms. symptoms.
Diagnosis of TMJ dysfunction includes:
- collecting a detailed medical history;
- palpation and auscultation of the temporomandibular joint for pain, the presence of sound phenomena (clicking, crunching when moving the jaw);
- assessment of the range of movements, the presence of “jamming” of the jaw when closing and opening the mouth;
- determining the type of bite and assessing the functionality of the facial muscles.
To assess the condition of the TMJ, an instrumental study is carried out:
- orthopantomography (a full-facial survey image in which a specialist simultaneously sees the entire dental system, which makes it possible to diagnose various pathologies of the dentition, assess the condition of periodontal tissues, identify any abnormal changes in the temporomandibular joint, etc.);
- Ultrasound;
- radiography, MRI or CT of the joint;
- rheoarthrography or Dopplerography - to determine arterial hemodynamics;
- electromyography;
- Gnathodynamometry.
Based on the results of the examination, the specialist decides to choose a treatment method that will most effectively cope with the problem. In some cases, conservative therapy is sufficient, but TMJ dysfunction may also require the intervention of maxillofacial surgery.
Treatment methods for temporomandibular joint dysfunction range from simple recommendations for caring for the affected joint and prescribing conservative therapy to surgical intervention. The treatment plan is drawn up individually in each clinical case and depends on the severity of symptoms and progression of the disease. But in all cases, therapy begins with sanitation of the oral cavity - treatment of periodontal disease, teeth, oral mucosa, and correction of dentures.
During the entire period of the main treatment of TMJ dysfunction, patients are prescribed a gentle diet and limited speech load to reduce the load on the temporomandibular joint. Depending on the root cause of the disease and the symptom complex, not only dentists of various specializations, but also chiropractors, osteopaths, vertebrologists, psychotherapists, and neurologists can take part in therapy.
To relieve pain, drug therapy is prescribed - painkillers, sedatives, intra-articular injections and blockades. Special myogymnastics, physiotherapy, massage to relax the masticatory muscles are indicated.
Physiotherapy is an effective conservative method of treating muscle-joint dysfunction. The choice of technique depends on the clinical picture of the pathology, the results of electromyographic, radiological and other research methods, the patient’s tolerance to medications and physical methods of influence.
For painful TMJ dysfunctions, it is quite effective to prescribe microcurrent therapy to the area of the joint and masticatory muscles, as well as infrared magnetic laser therapy, electrophoresis, inductothermy, etc.
In addition, treatment of TMJ dysfunction includes (according to indications):
- selective grinding of teeth;
- correction of prosthetics or re-prosthetics;
- refilling;
- correction of malocclusion;
- wearing special orthopedic splints or mouth guards, as well as other methods aimed at restoring proper closure of teeth.
If there is no effect from conservative methods of treating temporomandibular joint dysfunction, surgical intervention is required. Surgical therapy offers a number of effective treatment methods, including myotomy of the lateral pterygoid muscle, arthroplasty, condylotomy of the head of the mandible, etc.
To treat dysfunction of the temporomandibular joint, various orthodontic and orthopedic structures are widely used, for example, a simulated joint splint. This design relieves the temporomandibular joint, eliminates pain and creates conditions for the articular head to occupy the correct position. These splints are designed for daytime wear; they cause virtually no discomfort and allow a person to communicate freely without experiencing pain or muscle tension.
Specialists at the Canadian Center for Innovative Dentistry and Neuromuscular Therapy use the latest developments in conservative therapy to treat temporomandibular joint dysfunction and resort to surgical treatment only as a last resort. An integrated approach allows our doctors to treat even the most complex cases of TMJ dysfunction in a short time, while achieving the best results.
Treatment for TMJ dysfunction is, without a doubt, mandatory and necessary. This problem cannot be neglected, since further development of the disease is fraught with the occurrence of severe complications - dystrophic changes in the temporomandibular joint and even its complete immobilization (ankylosis). An integrated approach and combination of treatment methods guarantee a positive result.
The Canadian Center for Innovative Dentistry and Neuromuscular Therapy is one of the most progressive dental clinics in Moscow. A competent approach, the use of the latest technologies and developments in the field of neuromuscular dentistry make it possible to quickly eliminate all manifestations of TMJ dysfunction and restore normal, adequate functioning of the dental system.
The temporomandibular joint, or, as real osteopaths say, “TMJ,” is actively involved in adaptive posture. Let's consider postural phenomena corresponding to TMJ dysfunction. It is important to note that we are not necessarily talking about changes in the body that occur with temporomandibular joint disorder. We will try to describe the postural picture into which TMJ dysfunction harmoniously fits, and the cause of all this can be, as usual, anywhere.
"TMJ Dysfunction"
What is “TMJ dysfunction”? As in all our osteopathy, where we do not like the one that moves poorly, we will not like the temporomandibular joint that moves poorly, i.e., the hypomobile temporomandibular joint. Hypomobility of the joint area can be at different levels: ligaments, muscles, the joint itself, cranial-sacral rhythm, fascial, intraosseous restrictions of mobility, and all sorts of others. The second TMJ in such cases usually compensates for the hypomobile one, and gradually “stretches, loosens” and becomes hypermobile. As a result, we will have a smile where one joint is hypomobile and the other is hypermobile. The range of motion of a hypomobile TMJ is less than that of a hypermobile one, and therefore, when opening the mouth, asymmetry will occur: the lower jaw will not descend along the midline, which is sad.
Rice. The right joint is hypomobile, the left is hypermobile. Based on Guido Mazzoni (um 1445–1518), Kopf eines Franziskaners, Terracotta, originale Fassung, Höhe 24.5 cm, Museo dell'Osservanza, Bologna. Asymmetrical movement in the TMJ with deviation of the lower jaw when opening the mouth can be of two types:
- Deviation is the deviation of the lower jaw from moving along the midline, but with its return to the straight initial axis in the final stage of mouth opening.
- Deflexion is also a deviation of the lower jaw, but without returning to the midline at the end.
Rice. With the physiological opening of the mouth, the lower jaw descends along the midline. Rice. With deflexion, when opening the mouth, the lower jaw deviates and the interincisal line moves away from the middle. Rice. With deviation, the lower jaw deviates from the midline, but then returns to it again. Postural dysfunction of the temporomandibular joint is included in the pathological adaptive posture. Below are other elements of this pathological posture. It turns out that in most cases, deviation (deviation, deflexion) of the lower jaw when opening the mouth occurs towards the hypomobile temporomandibular joint - a joint in dysfunction. Stiffer and less mobile tissues in the hypomobile TMJ region do not allow the same freedom of movement and “pull” the lower jaw towards itself. Some more primary dysfunction, manifested by tissue hypomobility in the TMJ, also often “pulls on itself” other parts of the body.
Posture in the frontal plane
Cervical region. At the level of the cervical region, TMJ dysfunction corresponds to a tilt of the head in the direction of dysfunction and a turn in the direction opposite to TMJ dysfunction. Tilt is realized to a greater extent at the C0-C1 level, and rotation at the C1-C2 level. Dynamically, rotation of the head in the direction of TMJ dysfunction will be limited, and in the opposite direction it will be free. Shoulder girdle. At the level of the shoulder girdle, the shoulder girdle and scapula rise on the side of the TMJ dysfunction. In addition, the hand on the dysfunctional side will be functionally “strong”, while the one on the opposite side will be “weak”. Rice. Posture with dysfunction of the right temporomandibular joint: tilting the head to the right, turning to the left, raising the right shoulder girdle. Taz. At the pelvic level, there is a rise of the cranial pelvic bone on the side of the TMJ dysfunction. This triggers adaptation of the pelvis and legs, causing in turn a series of adaptive changes in the form of functional lengthening of the leg on the side of the “high” pelvic bone (so that this pelvic bone can be high). In the figure below we see that the cup from which the girl drinks is a functional fulcrum for her posture. The body is aligned in an arc around the physiological functional center - the point of contact with the bowl. Posture is organized in a similar way around pathological fulcrum. Rice. Adaptation of the pelvis is expressed in the elevation of the right pelvic bone on the side of the dysfunction of the right TMJ. Based on Girl Drinking from a Shell, Edward McCartan, plaster garden figure, photographer Louis H. Dreyer, photograph from Archives and Special Collections, Smithsonian American Art Museum. In the last example, the position of the head does not fit into the postural phenomena we described earlier, so let's ignore it.
Features of treatment
Treatment of arthrosis of the jaw joint is often carried out not by a rheumatologist (a specialist in joint diseases), but by a dentist, or both specialists. As with other types of osteoarthritis, it is necessary to change your lifestyle, reduce the load on the joint, give up bad habits and stick to a diet. A specific feature of the diet for this localization of arthrosis: you can only eat soft, liquid, pureed food. Medications include NSAIDs and chondroprotectors; for painful muscle tension, muscle relaxants.
Along with medication and physiotherapy, orthopedic or surgical treatment of arthrosis of the maxillofacial joint is indicated. The choice of method depends on the stage and etiology of the disease. Directions of orthopedic treatment:
- elimination of contact disorders between the teeth of the upper and lower jaws;
- restoration of the normal shape and anatomical integrity of the dentition;
- bite correction using palatal plates;
- using mouth restrictors to minimize stress on the joint and prevent more serious problems.
Methods of surgical treatment:
- removal of the articular head;
- removal of an intraarticular disc;
- replacement of the articular head with a graft;
- endoprosthetics.
Maxillofacial arthrosis occupies a special place among non-inflammatory diseases of peripheral joints. Specific local factors can lead to its development. It manifests itself not only with symptoms characteristic of osteoarthritis of any joints of the extremities, but also with a number of special signs.
Treatment of this disease is prescribed and carried out mainly by dentists; orthopedic and orthodontic methods play a crucial role in it. A patient with an advanced form of TMJ arthrosis cannot eat or communicate normally, and these are very important functions. Often the problem can only be corrected through surgery.
Source artroz-help.ru
Note. In this block, the term “osteoarthritis” is used as a synonym for the term “arthrosis” or “osteoarthrosis”. The term "primary" is used in its usual clinical meaning.
Excludes: spinal osteoarthritis (M47.-)
Included: arthrosis of more than one joint
Excludes: bilateral involvement of the same joints (M16-M19)
Excluded:
- arthrosis of the spine (M47.-)
- rigid big toe (M20.2)
- polyarthrosis (M15.-)
ICD-10 alphabetical indexes
External Causes of Injury - The terms in this section are not medical diagnoses, but rather a description of the circumstances under which the event occurred (Class XX. External Causes of Morbidity and Mortality. Heading Codes V01-Y98).
Medicines and chemicals - table of medicines and chemicals that have caused poisoning or other adverse reactions.
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997 No. 170
The release of the new revision (ICD-11) is planned by WHO in 2022.
Abbreviations and symbols in the International Classification of Diseases, 10th Revision
NOS
- without other instructions.
NEC
— not classified in other categories.
†
— code of the main disease. The main code in the dual coding system contains information about the underlying generalized disease.
*
- optional code. An additional code in the double coding system contains information about the manifestation of the main generalized disease in a separate organ or area of the body.
Source mkb-10.com