Active use of adhesion allows you to restore dentition with various defects. All damage and destruction can be easily repaired, and the smile will again become aesthetically attractive. Adhesion, translated from Latin, means “sticking” of various types of solid surfaces to each other. Adhesive systems have been actively used in dentistry for decades, but their composition has been somewhat improved in recent years. Thanks to this solution, it was possible to identify the latest methods for adhesion of substances to tooth tissue, making it possible to use adhesives for many indications.
The term "adhesive"
An adhesive is a complex chemical substance. It helps ensure a tight bond between the filling material and the etched enamel. Before installing a filling, the substance is applied to the enamel and dentin, because without it, the materials used in dentistry will not be able to adhere properly. Dentin tissue and adhesive systems used in dentistry are bonded together to resist separation by transmitting load through bonding surfaces. To carry out high-quality filling, you cannot do without adhesion. Filling materials will not be able to adhere to the dentin tissue on their own, and there are several reasons for this:
- high viscosity of materials;
- lack of chemical similarity with dentin tissue, lining and enamel.
It is impossible to use only mechanical fixation of the filling, because its service life in this case will be significantly reduced.
Operating principles of adhesive systems
Composite materials require additional substances to be more securely fixed to dental tissue. It is these materials that are considered modern adhesive systems, which are also called bonds. They are similar in their chemical composition to dentin tissue and have the micromechanical ability to bond with it.
If adhesives are not used during tooth filling, then the bond between the dentin and the composite will be disrupted. Such treatment during polymerization of the composite material will shrink and a marginal gap will appear.
Such consequences lead to the patient developing secondary caries or, even worse, the pulp being damaged. Many types of composite materials have good adhesion to the enamel surface. But the dentin tissue is wet and does not allow the filling to reliably adhere to the surface.
Adhesive bonding can be divided into three stages:
It is possible to carry out high-quality dental restoration only using modern adhesive systems in dentistry. To reliably glue materials, many different techniques and means have been created. The requirements for adhesive quality can be compared with industrial ones.
Basic requirements for adhesive systems
Adhesive systems are a complex of complex liquids that help attach composite and other types of materials to the hard surface of the tooth. That is why a lot of serious requirements are placed on them. Among them:
Today, a large number of adhesive systems have been developed, the problems of application of which are minimized. Most of the new generation helps ensure the strongest adhesion of the composite to tooth tissue and other materials used in dentistry: metal, plastic, porcelain and others.
5th generation adhesive systems
In the 5th generation adhesive systems, the mixing problem was eliminated - the “one bottle” concept was implemented, i.e. the adhesive and primer were placed in one container (they became one-component).
The use of one-component systems also involves total etching of enamel and dentin. The mechanism of their connection is similar to the mechanism of adhesion of 4th generation systems. These materials have good adhesion rates to enamel, dentin, ceramics and metal (at the level of 20-25 MPa), but their most important advantage is the absence of the component mixing stage, the poor performance of which led to a decrease in adhesion rates in fourth-generation systems.
Fifth generation adhesive systems are still the most popular because they are easy to use and give predictable results. Postoperative sensitivity when using them is also low. But the strength of adhesion, whatever one may say, is worse than that of our “gold standard” - the fourth generation.
Principles of working with adhesive systems
There are no special principles for working with adhesive systems, unlike the previous ones, but still consider
I understand that this should be stated.
- Etching the enamel surface for 15 seconds using 37% phosphoric acid, which is part of the etching gels, adding the gel to the dentin for 15 seconds;
- Removing the etching gel with a stream of running water for 30 seconds;
- Drying enamel and dentin (quality control of etching - etched enamel has a matte tint, dentin should not be overdried - moist, shiny);
- Application of the adhesive system to the enamel and dentin of the carious cavity using an applicator (exposure 15 seconds);
- Distribution of the adhesive system using a weak air stream;
- Photopolymerization of the adhesive system;
- Addition of composite material.
6th generation adhesive systems
The next task of developers when improving adhesive systems was the need to remove the etching stage from the list of procedures performed. In sixth generation systems this problem has been solved.
Generation 6 adhesive systems are one-step, self-etching systems that come in 2 bottles and require mixing immediately before use. The system is then applied to the enamel and dentin. At the same time, etching, diffusion into the tooth tissue and the formation of a hybrid zone are ensured.
Compared to adhesive systems of the 4th and 5th generations, they are easier to use, working with them requires less time due to the reduction in the number of steps, and the risk of technical errors is reduced.
However, adhesion to dentin (18-23 MPa) remains virtually unchanged over time, while adhesion to enamel deteriorates.
Stages of working with 6th generation adhesive systems:
- outside the oral cavity, the components of the adhesive system are mixed (inside a disposable package or in a special cell);
- applying the adhesive system to the enamel and dentin of the carious cavity using an applicator (exposure 15 seconds);
- distribution of the adhesive system using a weak air stream;
- photopolymerization of the adhesive system;
- introduction of composite material.
Classification of adhesive systems in dentistry
Today, experts specifically highlight two types of adhesive systems:
As modern technology has developed, adhesive materials used for dentin tissue have also improved. Today, scientists offer several types of them, which in dentistry are considered to be generations. Each of them differs from the others in the technique of bonding to dentin and the strength of the ligament.
Generations of adhesive systems
All seven generations have their own characteristics and properties:
Today, thanks to modern technologies, new generations are constantly being developed and in the near future it is planned to release the 8th generation, which will be even more reliable and practical.
Adhesive systems for dentin
Ensuring good adhesion of a hydrophobic material to a hydrophilic one is quite a difficult task, which they have been trying to solve for many years. In a fairly short period of time, several generations of adhesive systems for dentin have changed, with development going in two directions - simplifying the procedure for use and improving the adhesion itself. But we all know that simple and high quality are far from synonymous. The term “generation” does not, by and large, have any scientific basis; nevertheless, it allows us to structure in a certain way the whole variety of adhesive systems present on the market today. Belonging to a particular generation is determined by the chemical composition, mechanical adhesion indicators and ease of use.
1st generation adhesive systems
The first generation of adhesive systems has fairly strong adhesion to enamel, but minimal adhesion to dentin. The adhesion mechanism is carried out due to the interaction of calcium, which is part of the teeth, and the bond. After some time, postoperative sensitivity appeared, because the restoration in the dentin was “dangling”, holding on to the enamel with all its might. These generation adhesive systems have been recommended for use with Class III and V cavities only.
2nd generation adhesive systems
The main difference between the second generation adhesive system and the first is that this adhesive will interact with the smear layer, which was not previously involved. But this improvement only helped to slightly increase the period of stay of the restoration in the oral cavity. Postoperative sensitivity was still observed and about one third of the restorations required replacement after a year.
3rd generation adhesive systems
After some time, scientists were able to develop a two-component adhesive system that ensured adhesion of the composite to both enamel and dentin (adhesion values of 8-15 MPa), but apparently it was still not good enough. Postoperative sensitivity decreased significantly, the service life of the restoration increased, but most restorations required replacement after 3 years.
4th generation adhesive systems
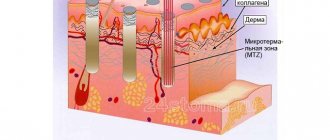
4th generation adhesive systems were quite a big leap in the entire history of adhesive systems and are still the “gold standard”. As I said, simple and high quality are far from synonymous. Postoperative sensitivity decreased even more, and the adhesion rate doubled. The technique of total etching and wet dentin bonding appeared for the first time. These adhesive systems owe much to the hybrid layer that forms between the dentin and the composite. After etching, the adhesive interacts with the collagen fibers of dentin, penetrating the dentinal tubules and forming an intermediate layer that is neither dentin nor adhesive, which is called hybrid.
The main disadvantage of these systems is the difficulty of use, because All the necessary components (there are three of them) must be mixed in precise proportions. It was due to these inaccuracies that problems arose when using these systems.
As we have already said, these adhesive systems contain 3 components:
1) Conditioner (phosphoric acid in the form of a gel for etching enamel and dentin);
2) Primer (a mixture of hydrophilic low molecular weight compounds that penetrate wet dentin, saturate it and form a hybrid layer);
3) Enamel adhesive system (unfilled resin that ensures the bond of the composite with the hybrid layer and tooth enamel).
Stages of working with 4th generation adhesive systems Type 1:
Provides for cleaning only enamel.
- Etching the enamel surface for 20-30 seconds using 37% phosphoric acid, which is part of the etching gels;
- Removing the etching gel with a stream of running water for 20-30 seconds (you need to wash it off for the same number of seconds as you etched it).
- Drying the enamel and controlling the quality of the etching (etched enamel has a matte tint);
- Applying primer to the dentin of the carious cavity using an applicator (exposure 10 seconds);
- Distribution of the primer using a weak stream of air (in this way, excess is removed and the primer penetrates more deeply into the dentinal tubules).
- Introducing the enamel adhesive system into the carious cavity using an applicator (applied to prepared enamel and dentin);
- Distribution of the enamel adhesive system using a weak air stream;
- Photopolymerization of adhesive and primer;
- Addition of composite material.
Type 2:
Provides for complete dissolution of the smear layer by etching dentin with phosphoric acid.
Stages of working with 4th generation adhesive systems Type 2:
- Etching the enamel surface for 15 seconds using 37% phosphoric acid, which is part of the etching gels, adding the gel to the dentin for 15 seconds;
- Removing the etching gel with a stream of running water for 30 seconds;
- Drying enamel and dentin (quality control of etching - etched enamel has a matte tint, dentin should not be overdried - moist, shiny);
- Applying primer to the dentin of the carious cavity using an applicator (exposure 10 seconds);
- Distributing the primer using a gentle stream of air;
- Introducing the enamel adhesive system into the carious cavity using an applicator (applied to prepared enamel and dentin);
- Distribution of the enamel adhesive system using a weak air stream;
- Photopolymerization of adhesive and primer;
- Addition of composite material.
What are the advantages of these systems?
Modern adhesive systems in dentistry help to recreate the integrity of the dentition and have many other advantages that make them so popular:
- The negative impact on dental units is minimized, which serves as a reliable support for the structure. There is no need for pulp removal, and surface treatment is orthopedic reversible. Due to this, it is possible to preserve the sensitivity of healthy teeth.
- The procedure is completely painless and does not require the use of painkillers.
- The time for prosthetics is significantly reduced.
The main advantages of adhesive systems include low cost. The use of these systems helps restore damaged teeth for a minimal amount, which is why many patients with dental defects choose this type of prosthetics.
Procedure for the bonding procedure
In most cases, the bonding procedure is not long (it takes less than 1 hour to process one tooth) and does not require prior preparation. In this case, most often, all manipulations associated with the application of composite material to the surface of the restored teeth are carried out without anesthesia: anesthesia is required only in cases where the drawn up treatment regimen provides for the preparation of the resulting carious cavity.
The bonding procedure includes several stages:
- selection of a composite material, the shade of which most closely matches the natural color of the patient’s tooth enamel;
- cleaning the edges and giving the surface of the enamel layer a slight roughness using a specialized dental instrument;
- etching the surface layer of enamel with an acid-containing gel, which promotes the appearance of microscopic irregularities on the enamel, which subsequently ensure the most reliable adhesion of the composite to the surface of the teeth;
- treating the tooth with a special conditioning compound that moisturizes the enamel layer and ensures reliable adhesion to the composite;
- layer-by-layer application of composite material to teeth;
- aligning the contour, giving its coronal part the required shape;
- irradiation of treated teeth with ultraviolet light;
- removing excess composite and grinding the enamel surface.
Most popular adhesives
Since the first developments began and the first adhesives appeared, about 50 years have passed. During this period, many unique systems have appeared that allow solving even the most complex problem. Among this huge variety, dentists distinguish several adhesive systems, the characteristics of which are slightly different:
This is a small list of adhesive materials and systems in dentistry that are actively used to help patients eliminate all dental defects. They have been widely used in dental practice in recent years and have proven that they do not cause any unwanted manifestations or discomfort.
How are adhesive systems selected?
It is better to give preference to materials that can provide a strong bond between composite substances and tooth tissue. It is very important that adhesion occurs within seconds of application. The primer should spread easily and penetrate the structure of collagen fibers.
A useful system is one that can be used in a variety of clinical situations. Saving time and wasted materials can only be achieved if you use innovative composites, which, when exposed to a stream of air, dry immediately and do not form unevenness.
In their daily work, many specialists prefer the 4th generation of adhesion in dentistry; its interaction with the hard tissues of the tooth is simply ideal.
As for the 7th generation adhesion, which appeared relatively recently, it can be used for indirect and direct restorations. Whatever system the patient chooses, it is important not to deviate from the instructions for using the adhesive, because the manufacturer precisely prescribes the limitations and principles of interaction with other materials.
Adhesive fixation in orthopedic dentistry ua:12143
Adhesive fixation in prosthetic dentistry
The need to find an alternative to amalgam and the growing interest of patients in highly esthetic restorations has led to an increase in the popularity of composite materials in restorative dentistry. The effectiveness of these materials in terms of aesthetic results and biomechanical properties has already been proven. The main disadvantage of composite materials remains polymerization shrinkage, which directly depends on the content of fillers. When working with large cavities, especially in cases where the cervical edge lies in the thickness of the dentin, polymerization of a large volume of filling material can cause increased shrinkage, leading to a violation of the marginal seal and other marginal defects that open the way to bacterial infiltration, relapse of caries, and irritation of pulp tissue , and contributing to the occurrence of postoperative sensitivity and color changes at the edges of the restoration.
A promising method to address the problem of polymerization shrinkage has been the use of a thin layer of composite luting material in combination with indirect restorations such as veneers, onlays, inlays and onlays. This thin layer remains the only part of the restoration that shrinks.
Today, adhesive luting is a predictable procedure that can be used for both indirect composite and all-ceramic restorations and endodontic posts. This procedure is extremely important as it guarantees a favorable long-term prognosis. However, in this article its discussion concerns mainly the criteria for selecting the most suitable materials and methods of their application. When choosing cement for fixing inlays, the following must be taken into account:
criteria:
Mechanical: for the formation of micromechanical and chemical adhesive bonds.
Structural: to increase the strength of the restoration.
Biological: to seal the boundary between the hard tissues of the tooth and the restoration.
Aesthetic: for an ideal shade match between the natural tooth structure and the restoration.
Cementation of indirect restorations can be performed using light-curing, self-curing, and dual-curing materials.
Light-curing composite cements are usually produced in the form of a paste, enclosed in an opaque syringe with a light-protective coating. They are very easy to use, allow better control of the curing time and provide high-quality edge shaping due to their high filler content. However, photoactivated curing is a disadvantage when working in large cavities, as ultraviolet light may not penetrate deep enough to activate the benzoyl peroxide, resulting in only a small portion of the cement being converted. And this affects the mechanical properties of the material. An additional disadvantage can be considered the high polymerization shrinkage characteristic of this group of materials.
Among the advantages of self- or dual-curing composite cements are optimal monomer conversion rates even at low light intensity; Their disadvantages include exceptional fluidity.
Moreover, the need to mix two components (for example, a powder and a liquid or two pastes) leads to pore formation, which, in turn, compromises the adhesion strength between the material and the natural tissues of the tooth.
Self-curing cements allow less control over the polymerization time, but are characterized by reduced polymerization shrinkage, which was achieved in particular due to their viscous consistency. Dual and self-curing composite cements can also cure in areas where ultraviolet light does not penetrate. But in this case, the countdown of the polymerization time begins from the moment the two components are mixed. The physical and mechanical properties of composite materials are closely related to the level of conversion of monomers to polymers. When working with light-curing materials, it is important to remember that the conversion level decreases as the distance from the light source to the filling material increases, since the light radiation partially loses intensity as it passes through the restoration. Such results (confirmed by studies of the level of polymerization conversion of light-curing flowable resin-based composites during the cementation of inlays of various thicknesses) clearly demonstrated that the materials included in this group cannot be considered adequate due to the lack of evidence of high-quality curing when attempting to cement restorations with a thickness of 3 mm or more . The only indication for the use of such materials is the fixation of veneers, the insignificant thickness of which does not prevent the penetration of light radiation into the thickness of the composite material and the start of the polymerization process. Preheating light-curing composites has been shown to increase monomer conversion rates and thus improve material properties, allowing for greater uniformity and ease of application.
In vitro studies have shown that the conversion rates of self-curing microhybrid composites preheated in an oven to 54°C and then used to luting restorations of varying thicknesses (2, 3 and 4 mm) are similar to those found in for dual-curing cements with the same light radiation, regardless of the light source (LED or halogen lamp). Therefore, this technique is particularly interesting because it combines the advantages of photoactivatable materials and a high level of monomer conversion. Moreover, this technique is used when fixing restorations on teeth of both the frontal and lateral groups.
Maxcem Elite™
Self-etching, self-adhesive composite cement for indirect restorations
Maxcem Elite™ cement is Kerr's latest innovation in self-adhesive cementation. While the market continues to gradually embrace technological advances in this relatively new product category, there remains some concern regarding the adhesion strength of systems that eliminate the need for a separate adhesion procedure. Maxcem Elite™ has been formulated to address these concerns by scientifically substantiating the principles of self-adhesive cements and improving the chemical composition, resulting in high adhesive strength and superior esthetic results.
NX3™
Permanent cement
NX3™ is a versatile permanent luting system for all indirect restorations, featuring an innovative chemistry to provide unrivaled esthetic results and adhesion. Thanks to a special amine-free initiation system and a perfectly balanced matrix, NX3™ cement has all the properties of an ideal composite cement - color stability, high adhesion strength, excellent mechanical properties, reduced solubility and excellent translucency. NX3™ dual- and light-curing cements are versatile, suitable for the luting of all types of indirect restorations, including veneers, and provide unsurpassed esthetics, ease of use, excellent adhesion to all substrates and the widest range of applications. In addition to excellent adhesion to dentin, enamel, ceramics, porcelain, composites and metals, NX3™ cement also has excellent adhesion to CAD/CAM blocks.
#Orthopedics
Kerr 4529 • 04/05/2012
Reviews
There are also many good reviews of other materials from specialists who work with them easily. Patients respond well to the latest generation systems, because they do not feel them at all. But after interviewing the majority who had their teeth restored using one of the adhesive systems, it became clear that most of the materials provide reliable adhesion to the enamel. The systems do not cause side effects and retain their original appearance for a long time. Therefore, patients who have already tried adhesive systems recommend them to all those who have problems with their teeth. Of course, there are those who are dissatisfied with these systems for various reasons, but their percentage is negligible compared to the number of positive reviews about adhesive systems.
Positive and negative aspects of this method
Like any other medical procedure, bonding has its strengths and weaknesses. However, the advantages of treatment in this way are much greater than the disadvantages:
- the main advantage is minimal, compared to the installation of crowns and veneers, damage to the enamel;
- the procedure does not require strong boring of the surface of the tooth undergoing the procedure and the adjacent chewing organs;
- often the entire process is completed in one visit to the doctor and does not require any preparatory work in the dental laboratory;
- After the procedure, no traces of the dentist’s intervention remain on the treated teeth.
However:
- polymer materials are not as strong as crowns or fillings, so after bonding the likelihood of chipping or even complete destruction of the structure may be somewhat greater than after tooth restoration using other methods.
- Also, the gels used are not as resistant to changes in shade as crowns.
Thus, the balance of advantages and disadvantages of the procedure makes bonding a good option for correcting small chips and damage, as well as for eliminating cosmetic defects. However, to deeply restore the tooth surface and give it greater strength, it is better to use crowns.