With bruxism, convulsive attacks of contraction of the masticatory muscles occur, due to which the upper jaw comes into contact with the lower jaw, and others can hear the creaking sound of teeth rubbing. According to some data, only 3% of adults and almost 50% of minors experience this pathology .
The principle of treating bruxism in a child depends on the cause of its occurrence. If you do not get rid of the pathology in time, it can provoke the development of diseases of the nervous system and oral cavity.
Features of the pathology
Bruxism is unconscious grinding of teeth , which occurs during night sleep, a little less often during wakefulness. The pathology has only a chronic form; teeth grinding occurs in attacks.
Bruxism can be divided into nighttime and daytime. The second conditionally is called “bruxiomania” and is well controlled; it rarely appears in adults. Nighttime is dangerous because it goes unnoticed for a long time and is detected only after persistent complications arise.
Why is night bruxism dangerous?
Should parents worry and take some measures if their baby grinds his teeth in his sleep? Yes, if:
- Child's age over 7 years
Most often, teeth grinding during sleep occurs in young children, and by the age of seven it usually goes away without a trace. If the child has already gone to school, but the problem remains, it’s time to take measures to eliminate it.
- A large number of repetitions of this condition are recorded or attacks last more than 15 seconds
In these cases, unpleasant sounds made by teeth during sleep may indicate serious disorders in the activity of the nervous system. The sooner the diagnosis is made and treatment is prescribed, the greater the chance of avoiding the disease becoming chronic.
- There are signs of tooth decay or gum inflammation
If you do not take action in a timely manner, you may face much more serious problems: gum disease, premature loss of baby teeth, and malocclusion.
Bruxism becomes especially dangerous when baby teeth are replaced by permanent teeth. It can cause diseases that will lead to the loss of permanent teeth at an early age.
Doctors do not consider bruxism a health-threatening disorder, especially if we are talking specifically about nighttime teeth grinding. It usually goes away with age without any treatment.
If you want to help your baby cope with the problem before he outgrows it, then first consult a dentist.
Symptoms
During night sleep, the patient usually does not experience discomfort; noticeable symptoms appear only after waking up. A person is not able to understand what exactly led to the appearance of signs of bruxism. These include:
- headache;
- feeling of weakness and fatigue;
- pain in the chewing muscles;
- discomfort in the sinuses;
- ringing or pain in the ears.
Attacks of teeth grinding last about 5-10 seconds and can be repeated an unlimited number of times throughout the night. The longer the creaking lasts, the stronger the signs of bruxism are felt the next morning.
Prevention of bruxism
It’s not for nothing that they say that the best treatment is prevention. Based on what you already know, it is easy to guess that you will have to monitor the psycho-emotional state of the children and not allow them to sit until late. We eat no later than 8 pm, go to bed no later than 10. The food must have a balanced vitamin and mineral composition. If you notice that your child is snoring or has nightmares, contact your doctor. Now somnologists (sleep specialists) are achieving amazing results in the treatment of any disorders.
The child goes to bed
Most of the baby's food is soft foods. These are soups, cereals, desserts. It is necessary for the jaws to receive additional load. Fresh carrots or apples give the desired effect. While children chew, the muscles get tired and can no longer tense too much during sleep.
3 preventative methods to eliminate bruxism:
| Photo | Method of treatment | Description |
| Drug treatment | Boiled water with boiled herbs acts as a medicinal sedative. In addition to such prevention, your doctor may recommend a baby cooling gel for teething. | |
| Folk remedies | Use fresh vegetables and hard fruits (apples, carrots) in your diet. Temporarily exclude sweets and fast food products. To protect your tooth enamel, your doctor will recommend using a mouthguard or dental splint. This will reduce stress on the teeth. | |
| Psychological aspects | “Close your lips, keep your teeth apart” - recommendations of neurologists. A walk before bed, doing puzzles, reading books will also be useful for calming the child’s nerves. |
Possible complications
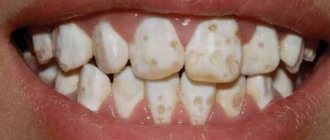
In both adults and children, bruxism is one of the most common causes of dental problems. The enamel of fragile baby teeth suffers especially: due to strong pressure, their tips are worn away, the crown is gradually destroyed, and increased sensitivity to temperature changes and sweets appears.
If you ignore the pathology for a long time, disastrous consequences will develop: the teeth can be ground down almost to the root.
Due to pressure, pathological mobility of teeth occurs. This results in gum damage and early root loss. Constant muscle tension provokes their enlargement and frequent soreness, which negatively affects the quality of life. Bruxism can also result in malocclusion.
Frequent and prolonged attacks of bruxism in children cause apnea - a short-term cessation of breathing during sleep. This is fraught with oxygen starvation, which negatively affects the functioning of the nervous system and internal organs.
Bruxism in a child - causes, possible complications and treatment methods
Bruxism is characterized by convulsive attacks of contraction of the masticatory muscles, resulting in severe clenching of the jaws and grinding of teeth. According to statistics, literally 3% of the adult population and almost 50% of children experience this pathology1. Treatment directly depends on the cause of the problem. But if therapy is not started in a timely manner, this can subsequently lead to the development of diseases of the nervous system and dental pathologies. Read further in this article about what it means if a child grinds his teeth at night in his sleep, and how to treat bruxism in children.
Causes of bruxism in children
To rid a child of bruxism, treatment must be aimed at eliminating the cause of its manifestation and preventing complications. There are ways to protect crowns from strong contact, but they will not save you from excessive tension in the masticatory muscles. It is not always possible to accurately determine the cause of the grinding noise.
Bruxism attacks can be triggered by:
- Heredity. If one of the parents has encountered such a disorder, the likelihood of teeth grinding in the child increases significantly.
- Malocclusion. Incorrect positioning of teeth affects the distribution of chewing load during eating, which causes persistent muscle tension. During sleep, the patient unconsciously tries to get rid of unpleasant sensations and “scratch” his teeth against each other.
- Unstable psycho-emotional state. Children are not able to cope with their emotions and express them correctly. Experiences accumulated during the day find a way out through the clenching of teeth at night. For the same reasons, bruxism often occurs in adults.
- Enlarged nasopharyngeal tonsils. Adenoids prevent the baby from breathing properly during sleep, resulting in night wheezing, coughing and grinding teeth.
- Unusual sensations. When a child gets his first teeth, he needs time to get used to them. At night, he may simply examine his own teeth, unconsciously touching his lower jaw to his upper jaw.
- Problems with enamel. Due to a lack of calcium, vitamins or minerals, the enamel becomes very thin and sensitive. By rubbing one jaw against the other, the child tries to get rid of unpleasant sensations.
If bruxism in a child is left untreated for a long time, night grinding can become a habit and persist for many years, including into adulthood. Therefore, therapy cannot be postponed.
The cause of the disease is indicated by the time when it manifests itself. Daytime bruxism is quite rare, and it is usually easier to deal with. Pathology is the norm for babies who have just cut their teeth. Friction helps them get rid of itching in the gums, for this reason squeaking occurs even during periods when the child is not sleeping. Over time, this pathology is “treated” on its own, without third-party interventions aimed at eradicating the habit.
The causes of bruxism that occurs at night are often considered to be stress and nervous experiences, as well as excessive physical activity immediately before bedtime. Such disorders do not need to be treated: it is enough to simply control the child’s behavior and the environment around him.
There is a myth that worms cause childhood bruxism. Parasites are active at night, causing severe itching, which causes the child to grind his teeth, expressing anxiety. The theory has not received medical confirmation.
Anti-bruxism mouth guards for children
Silicone mouth guards are perfect for children. The devices prevent teeth from touching during sleep and maintain the jaw in the correct position while awake. In addition, the mouthguard helps relax the jaw muscles. The child gradually gets used to a relaxed jaw and grinds his teeth less at night.
The habit of sleeping with a mouthguard develops after about 3 weeks . The device itself is selected individually. This takes into account the size of the teeth, the severity of bruxism and other anatomical features. The ideal option is when a mouth guard for bruxism is selected based on a dental impression of the teeth.
Basically, sleep guards are made from thermoplastics - soft polymers that are safe for the health of children. This material is non-toxic and non-allergenic, so mouth guards based on it can be used even if you have allergies. Thermoplastic mouthguards adhere well to tooth enamel, which provides protection against tooth abrasion.
Before installing a mouth guard for bruxism in your child, consult a doctor. The doctor will help you choose a device based on your child’s oral anatomy.
Diagnostics
In most cases, the child’s complaints and the testimony of parents who heard teeth grinding at night are sufficient to make a diagnosis. The condition of teeth damaged by frequent friction will also tell the doctor about the problem.
There are other diagnostic methods, many of which can be done without problems in Moscow and large cities:
Bruce-checker
Polysomnography. During the procedure, special sensors are attached to the child. When the baby falls asleep, they will record changes in the functioning of organs and vital systems.- Electroencephalography. Allows you to evaluate the electrical activity of the brain.
- Electromyography. Analyzes the work of the masticatory muscles and allows you to determine whether there is excess tension.
- Checker beam. A special mouthguard that is prepared based on a cast of the jaw. The device is worn overnight, and after just one night, specialists will be able to understand which teeth are suffering from overload, and whether there is any at all.
To determine the factor that triggered the development of bruxism in a child, visits to doctors of various specialties may be required: psychologist, neurologist, otolaryngologist, osteopath, dentist and gastroenterologist.
Diagnosis of bruxism
The initial diagnosis of bruxism is not difficult. Diagnostics consists of collecting and carefully studying the complaints of the patient himself or his loved ones.
Next, to establish a final diagnosis, it is necessary to undergo a dental examination, during which the dentist will identify the subjective symptoms of bruxism.
Objective diagnosis consists of wearing brux checkers - special medical mouthguards that are made individually for each patient. The blank of such a system is based on a cast and model of the jaw. The Brooks checker allows the dentist to determine the presence of occlusal obstructions. The mouth guard is installed for the period of night sleep, after which it is transferred for further diagnostics: with its help, the dentist determines exactly which teeth bear the maximum load.
Also, the pathology of active jaw movements can be seen on the results of electromyography or polysomnography.
If the patient has severe bruxism, then the diagnosis will indicate severe attacks of headaches, impaired functioning of the TMJ, the teeth will have uncharacteristic mobility, their sensitivity will be significantly higher than normal, and tooth enamel will be erased. Patients also often complain of tinnitus, constant nervous disorders and depression, eye fatigue, decreased appetite, and sometimes insomnia.
However, diagnosing bruxism is not as difficult as determining the underlying cause of this disease. Quite often, specialists such as a psychologist, gastroenterologist, osteopath, neurologist and others participate in the diagnosis.
Treatment of bruxism in children
To completely cure bruxism, it is necessary to eliminate its cause. At the first signs of pathology, it is advisable to visit a therapist and tell him about the problem. Only after collecting all possible complaints will the doctor be able to decide how to treat bruxism. Self-medication at best will not bring results, and at worst it will worsen the situation. The main emphasis in therapy is on the emotional state of the child.
Medicines
Officially, bruxism is not a disease, and there are no drug treatments for it - only the causes of the disorder can be corrected. Depending on the identified problem, the following may be selected for a small patient:
- vitamin B complexes;
- preparations with magnesium and calcium (Calcium D3 Nycomed);
- safe sleeping pills (Bayu-Bai, Dramamine);
- mild sedatives (Novo-Passit, Persen).
Before using any product, you should read the instructions and contraindications so that it relieves the disease and does not harm the body. If the baby develops side symptoms, further use of medications is canceled - to get rid of bruxism, you will have to select other sedatives and immunomodulators.
Psychology
Children are unable to adequately respond to stress, and negative emotions are caused by a variety of factors. Many problems seem insignificant to adults, and due to lack of attention, the child withdraws, trying to cope with the experiences on his own. If he fails to overcome his worries, night teeth grinding occurs.
If there is no good contact with the child, parents should seek the help of a psychologist to cure bruxism. It is necessary to constantly talk with the baby so that he has the opportunity to speak out and get rid of negative emotions before going to bed. Towards evening there should be no nervous situations, scandals or showdowns. Watching TV is replaced by reading a quiet book. A walk without active games or a warm bath with chamomile will help relieve tension.
It is important to explain to your child that you cannot constantly clench your teeth; they can only come into contact with each other while talking or chewing. If necessary, you will have to do a special massage or perform exercises to reduce muscle tension.
Eating before bed is prohibited. A “neglected” digestive system provokes unnecessary stress in the body, so the last meal is allowed 4 hours before falling asleep. Before going to bed, you can drink a glass of warm milk or natural rosehip decoction.
Dentistry
If teeth are damaged, they must be treated. The crown part can be restored with composite materials; fluoridation is used for strengthening. Damaged nerves will have to be removed, as will the tooth itself if it has decayed too much.
For bruxism in children over ten years of age, mouthguards can be used. This device, made of soft material, fits over the teeth and protects them from friction and subsequent damage. You can buy a ready-made mouthguard at a pharmacy, but it is better to make an individual one - based on a cast of the jaw. In the morning, the mouth guard is removed and washed from the inside with running water.
If bruxism is caused by a malocclusion, you should visit an orthodontist to find out why your teeth are clenching. At an early age, the position of the teeth is well corrected through the manufacture and wearing of special plates. For severely crooked permanent teeth, it is recommended to wear braces.
Folk remedies
A regular warm compress will help relieve tension in the masticatory muscles, which should be applied to the area of the teeth and joints several times a day, the duration of the procedure is half an hour. For an additional calming effect, add a couple of drops of essential oil with a light, unobtrusive scent to the water. The procedure should be repeated throughout the entire treatment period.
For maximum relaxation, decoctions of chamomile and valerian are added to the bath taken before bed. A glass of dry grass is poured with a liter of boiling water and simmered over low heat for 30 minutes. The liquid is filtered and poured into the bath. Regular use of soothing baths leads to normalization of the nervous system.
Soothing teas guarantee relief from excess nervousness. A complex mixture of chamomile and mint or pure lemon balm is suitable. To prepare the drink, a teaspoon of dry herb is poured into a glass of hot water, left to cool and filtered. Honey and lemon can improve the taste of this tea, but only if the baby is not allergic to them.
Bruxism triad
Bruxism is a pathology characterized by daytime and nighttime parafunctional activity, which is manifested by excessive clenching of the jaws, grinding and abrasion of teeth. And although the pathology is quite common in the daily practice of a dentist, there are still a number of controversial issues and contradictions regarding the pathogenesis and the corresponding treatment algorithm. First, there is an unresolved statistical question: how many people actually suffer from bruxism? Figures vary from 5% to 95% of the total population. Many dentists determine the degree of bruxism by the level of tooth abrasion, but this indicator only partially demonstrates changes in the dentofacial apparatus. Other clinicians associate bruxism only with the so-called sleeping bruxism, which is manifested by clenching of the jaws and abrasion of teeth due to disruption of the physiological process of sleep. The question of the pathophysiology of sleeping bruxism remains open, and researchers point to a violation of the neurochemical balance of the body, the state of the autonomic system and dyssomnia as possible causes provoking the pathology.
This article is devoted to the analysis of bruxism in sleeping people, since it is this form of pathology that causes not only the destruction of the structure of the teeth, but also compromises the general state of health. In addition, the authors also analyzed in detail the so-called triad: sleeping bruxism as a pathology, sleep disorders and gastroesophageal reflux as pathophysiological factors.
Abrasion of teeth
Abrasion of teeth (pathological abrasion), according to the literature, is defined as the loss of the structure of dental tissues, which is classified into attrition, abrasion, erosion, or a combination of these factors. Sleeping bruxism, among other things, is characterized by increased tooth mobility, hypersensitivity to temperature stimuli, and possible crown fractures. Although levels of tooth wear differ significantly between sleeping bruxers and healthy people, the effect of antagonistic attrition remains controversial. Researchers have suggested that abrasion is more related to the erosion factor than to the attrition factor. The combination of these conditions in the structure of the bruxism triad provokes an even greater level of abrasion of hard dental tissues in sleeping bruxists (photo 1).
Photo 1. The classic picture of bruxism: lateral wear of teeth, damage to hard tissues on the buccal side due to erosion and abrasion, a history of sleep disturbance.
The process of tooth abrasion is properly described in the sections of tribology - the science of the interaction of surfaces in relative motion and in contact through an intermediate lubricant or through friction and wear. Teeth placed one against the other are subject to complex tribological interactions. Friction occurs as a result of the movement of contacting surfaces. Since there are no perfectly smooth surfaces, even in cases of light load there is a slight loss of dental tissue during the period of contact. When there is an intermediate lubricant between rough surfaces, the coefficient of friction is significantly reduced. Therefore, according to this principle of tribology, a decrease in the amount of oral fluid (which acts as a lubricant) leads to an increase in the coefficient of friction, and thus provokes progressive abrasion of the surface of the teeth. In addition, factors that increase surface roughness (such as erosion) also significantly increase the rate of wear of the hard tissue structure (photo 2).
Photo 2. Asymmetric tooth wear during the bruxism triad: increased abrasion is caused by a deficiency of lubricant (saliva) due to the side effects of pharmaceuticals, surface roughness is caused by the erosive effect of reflux.
Intraoral lubricant is largely represented by saliva, which also lubricates the esophagus area, affects the buffering characteristics of the oral cavity and reduces the risk of aspiration. Salivation occurs according to the nature of the human body's circadian cycles and decreases significantly at night. During sleep, the swallowing function is episodic, and the periods of time without swallowing saliva are quite long: during the day a person swallows up to 25-60 times per hour, and while throughout the night - no more than 10 times. Salivation and salivary buffering capacity are individual parameters, and their role in the process of tooth surface abrasion is still being actively studied. Swallowing is almost always associated with microdisturbances in the physiological process of sleep, or more precisely in its light stage. Therefore, it is obvious that even microsleep disturbances have a fairly large impact on the occurrence and pathogenesis of bruxism in sleeping people. Reduced lubricant levels, erosive friction of surfaces, and contact time between opposing teeth play a key role in the tribology of tooth wear in sleeping bruxists. At the same time, the strength of the parafunctional effect turns out to be much less important than previously thought. For a long time, when studying bruxism, doctors relied on the fact that in patients with this nocturnal pathology, the force of clenching their teeth is 6 times higher than that of people with completely healthy sleep. This fact also explained why teeth wear down so much and restorations constantly break. But it turns out that real data contradicts this hypothesis. Gibbs and colleagues agreed that the bite force of some clinchers may be six times that of non-clinchers. But at the same time, during the analysis it was discovered that in most of the previously cited studies, the assessment of the bite force of bruxists was carried out only during the daytime, and no one studied the magnitude of the forces that arise during sleep. Also, in the course of such studies, specific experimental groups and comparison groups were not formed, which would differ only in the presence/absence of pathology. In fact, a study by Gibbs found that only one bruxist recorded a bite force of six times normal, and an analysis of muscle activity during sleep found that the levator mandibular muscles only in rare cases (and in most cases never at all) they reach the point of their extremum, that is, the possible maximum of action. In fact, the levels of muscle activity during sleep in bruxers do not exceed half of the maximum unconscious physiological interaction, and in only 66% of cases the level of muscle functioning at night is at a level of force equal to or greater than that generated during the act of chewing. And although patients with larger jaw muscles can indeed generate greater compressive forces with the same level of muscle activity, even in such cases the level of forces acting is within the daily norm, and certainly not six times or more.
Phases of sleep and awakening
Adequate sleep is important for physical recovery, renewal of biochemical systems, memory consolidation and emotional regulation. A typical sleep cycle ranges from 90 to 110 minutes, and the number of cycles per night ranges from 3 to 5. Sleep consists of two different states: non-REM (non-REM, restful sleep) and REM (REM, sleep) sleep. characterized by rapid eye movement, active sleep). The non-REM phase is characterized by four stages: phases 1-2 – light sleep, phases 3-4 – deep sleep. In the first third of the overall sleep cycle, non-REM stages 3-4 are the longest; they decrease or disappear altogether in the last third of the cycle, in which REM occurs. Dreams can occur at any stage of sleep, but during the REM phase they occur much more often and are more vivid in nature. Micro-awakening is a sleep shift that occurs during deep sleep. During these 3-10 seconds, increased brain activity occurs, heart rates increase and muscle tone increases. These processes occur from 8 to 15 times per hour. Bruxism is a manifestation of secondary orthomotor micro-awakenings. In 86%, the phenomenon of bruxism occurs at the stage of non-REM sleep and during physiological micro-awakenings. A significantly smaller percentage of pathology manifests itself during the REM sleep phase, however, in bruxists with a severe form of pathology, the number of episodes of parafunction increases significantly during sleep, including during its active phase.
Sleep disorders
Respiratory disorders during sleep fall into three categories: snoring, upper airway resistance syndrome (UARS), and obstructive sleep apnea-hypopnea syndrome. Snoring is determined by a specific sound produced in the upper respiratory tract by vibration of soft tissues, which is caused by air turbulence. Snoring occurs in approximately 40% of men and 24% of women, the prevalence among children does not exceed 10%. Snoring is one of the risk factors for obstructive sleep apnea. Medical consultation is mandatory in cases where snoring is accompanied by daytime drowsiness, insomnia, sleep disturbance, or hypertension, and is also advisable before the manufacture of intraoral appliances for the treatment of this pathology.
Upper airway resistance syndrome, due to the need for greater effort to inhale, increases the number of micro-awakenings and, among other things, leads to a narrowing of the pharynx. The latter factor reduces oxygen saturation to 4%. The pathology is characterized by repeated partial collapse of the upper respiratory tract during sleep and is associated with bruxism, headaches, and disorders in the temporomandibular joint. SUDDP is considered an intermediate form of disorder between snoring and obstructive sleep apnea-hypopnea syndrome.
Apnea is characterized by repeated periods of lack of ventilation with cessation of breathing for up to 10 seconds, with oxygen saturation typically exceeding 4%. Sleep apnea can be obstructive (the most common) due to blockage of the upper airway, or it can develop due to impaired chest movement due to a lack of adequate neural regulation. This type of apnea is called central apnea. There are cases when one patient experiences two types of apnea at the same time. Hypopnea is characterized by a decrease in airflow volume of more than 50%, or up to 30% when the level of oxygen desaturation exceeds 3%. The degree of obstructive sleep apnea is determined by the number of apnea/hypopnea events in one hour. The apnea/hypopnea index (AHI) classifies individuals with 5 to 15 events per hour of sleep as having a mild form of the pathology; from 15 to 30 – a moderate form of pathology and more than 30 – as a severe one. The severity of sleep apnea pathology is also determined by a combination of symptoms, which consist of AHI, daytime sleepiness and percentage of oxygen saturation. Risk factors for obstructive sleep apnea are male gender, overweight, age over 40, large neck size, large tonsil size, family history of the disease (photo 3). It is estimated that 1 in 5 adults have at least a mild form of the disorder, and 1 in 15 have a moderate form. Unlike bruxism, the prevalence of obstructive sleep apnea increases with age and can affect approximately 70% of men and 56% of women over the age of 65, three times more often than in middle-aged people. In addition, obstructive sleep apnea is a risk factor for hypertension, cardiovascular disease, daytime sleepiness and several other diseases.
Photo 3. When diagnosing bruxism caused by sleep apnea and acids, clinicians should always consider possible predisposing factors: age over 40 years, male gender, overweight, neck size > 17 inches.
Sleeping bruxism
You need to understand that a sleeping bruxist is not the same as a person who sometimes bruxes while sleeping. By definition, true bruxists experience more than 4 episodes of parafunction per hour of sleep, more than 25 urges to brux during the same time, and at least one episode of a peculiar sound per night. Sleeping bruxism is more typical for children and its manifestations decrease over time: up to 30% of cases are recorded at the age of 5 to 6 years, up to 13% at the age of 18 to 29 years, and only up to 3% in patients over 60 years of age. Unlike daytime bruxism, the pathology of sleepers is in no way connected with the theory of stress provoking the occurrence of parafunction. In addition, sleep bruxism is characterized by low variability in the number of parafunctions and urges per hour during sleep over long months and even years. In moderate to severe forms of sleeping bruxism, teeth grinding occurs almost every night.
Episodes of parafunction of sleepers are associated with disturbances in sleep architecture. Kato et al studied the effects of intentionally induced microarousals in sleep bruxers and controls. In the study group, due to provoked micro-awakenings, teeth grinding occurred in 71% of cases. Interestingly, this response was observed only in patients with bruxism, and never in healthy patients, indicating their ability to adapt to micro-arousals during sleep. Thus, it was possible to establish: everything that causes an increase in the number of micro-awakenings also provokes a greater likelihood of episodes of bruxism, teeth grinding and loss of their structure.
Airways
Researchers have found that increased episodes of sleep apnea are associated with increased episodes of bruxism. Considering the connection between micro-awakenings and bruxism of sleepers, it can be summarized that the frequency of bruxism episodes increases in parallel with the frequency of micro-awakening episodes caused by the apnea factor. At least one third of patients with bruxism also have breathing problems during sleep, resulting in episodes of apnea, periodic leg movements, and headaches. Obstructive sleep apnea is also characteristic of 30% of patients with temporomandibular joint disorders, and more than 50% with obstructive upper airway syndrome also complain of bruxism. Prospective research suggests that episodes of bruxism are directly related to sleep apnea. And although a direct cause-and-effect relationship has not yet been established, obstructive apnea syndrome is still identified as the most influential risk factor provoking the occurrence of parafunction. Most episodes of sleeper bruxism occur in the supine position, so they may be associated with either a decrease in airway passage or an increase in airway resistance. During resumption of ventilation after apnea, the combined activation of the jaw elevator and depressor muscles causes the upper airway to dilate. This allows you to increase the volume of air flow during inspiration and reduces the resistance of the upper respiratory tract. It has been established that 99% of the rhythmic activity of the masticatory muscles is associated with changes in the amplitude and frequency of respiratory movements. Thus, it is possible to answer another question regarding changes in the lateral contours of the tongue in sleeping bruxists: the patient, in an attempt to ensure airway patency, activates the tongue muscles and positions the tongue directly opposite the teeth to free up space for air to enter the larynx (photo 4). The high prevalence of sleeping bruxism is typical for 5-6 year old children and gradually decreases with age. Hypertrophy of the adenoid tonsils in childhood explains airway obstruction and, thus, explains the high prevalence of bruxism. As airway patency improves with age, the prevalence of bruxism in the general population decreases, but within its triad it continues to progress. That is, if bruxism is a reflexive mechanism to improve or protect the airway, then more frequent episodes of bruxism reduce the negative impact of apnea. Sjöholm concluded that there was a limited correlation between bruxing and apnea, as patients with mild apnea had more frequent episodes of bruxism than patients with moderate apnea. However, if bruxism is a protective reflex, doctors might then predict a decrease in the risk of apnea in the younger population of bruxers, since aggressive bruxism in 20-40 year olds is simply a mechanism to clear the airway. As people age, their neurochemical ability to regulate bruxing weakens, so maintaining a clear airway during sleep becomes increasingly difficult due to loss of muscle tone, weight gain, etc.
Photo 4. Changes in the lateral surfaces of the tongue caused by its unconscious disposition to the lingual surfaces of the teeth in order to ensure airway patency.
GERD (gastroesophageal reflux disease)
Gastroesophageal reflux disease (GERD) is characterized by the passage of stomach contents into the esophagus. This pathology affects approximately 40% of Americans. GERD is usually associated with heartburn or indigestion, although 50% of people who complain of throat irritation, hoarseness, or trouble swallowing have been diagnosed with silent GERD. In asymptomatic patients, sleep disturbance may be the only symptom of GERD. At the same time, we should also not forget about the differential diagnosis with peptic ulcer, angina pectoris and Barrett's disease of the esophagus (which often precedes adenocarcinoma). Some of the acidic elements in the stomach can reach the oral cavity. Such substances have extremely destructive acidity with a pH of 1 to 2 (for comparison, recall that dietary acids have a pH greater than 3). The most common site of acid damage is the palatal surface of the upper molars (Figure 5 and Figure 6). Reflux mainly occurs in the supine position: the back of the tongue pushes acids towards the maxillary molars during the act of swallowing to unconsciously minimize the effect of acids. Although the palatal surfaces of the molars are most susceptible to the action of acids in such cases, the overall picture of damage depends on the position that the patient takes during sleep. The activity of the tongue, associated with ensuring patency of the airway and the pathomechanism of regurgitation, can provoke damage to the lingual surfaces of the lower teeth (as in bulimia), and even reach the area of the anterior teeth of the upper jaw (photo 7). Patients with GERD are more often diagnosed with symptoms of xerostomia and feelings of heartburn in the oral cavity, and a deficiency of saliva (as a lubricant) in combination with the action of acids that provoke greater surface roughness, increase the risk of frictional wear of the tooth structure during episodes of night bruxism.
Photo 5. Roughness of the palatal surface of the maxillary molars may be the first signs of gastroesophageal reflux.
Figure 6. Signs of progressive erosion due to GERD: Areas of erosive damage depend on the patient's sleeping position.
Photo 7. Patients in whom the frontal disposition of the tongue (to ensure airway patency) is combined with signs of GERD have specific damage to the lingual surfaces of the teeth, reminiscent of bulimia, which can extend to the incisor area.
Triad: sleeper bruxism, sleep disturbance and gastroesophageal reflux disease
The triad of bruxism in combination with nocturnal hyposalivation or xerostomia significantly increases the risk of pathological tooth wear and erosive damage. The triad of bruxism consists of teeth grinding caused by micro-arousals, sleep disturbances associated with airway deficiencies, and sleep architecture disorders caused by GERD (Photo 8 and Photo 9).
Photo 8. A young man with signs of the bruxism triad: lateral wear of teeth, erosive and abrasive damage to their structure, a history of moderate apnea.
Photo 9. Extensive erosive damage to teeth. Improving airway patency can reduce the symptoms of GERD, and stopping GERD can affect the repression of parafunction.
Although a direct cause-and-effect relationship has never been established between these factors, the significant correlation justifies the need to diagnose these criteria in dental patients. Sleeper bruxism is closely associated with sleep apnea. Thus, if the level of apnea can be reduced, the result will be a reduction in episodes of bruxism. Oksenberg and Arons found that with continuous positive airway pressure, the symptoms of apnea completely disappeared and only minor signs of hypopnea remained. At the same time, all episodes of bruxism also disappear. The lower jaw disposition technique helps overcome the symptoms of bruxism in 50-83% of cases. The variability in the success of this technique is most likely due to the methodology of the technique itself, and, of course, the disposition of the jaw cannot provide equally effective results as treatment with continuous positive airway pressure. But the mandibular disposition technique can be used effectively in patients without respiratory problems. A statistically significant reduction (39% and 47%) in the number of episodes of bruxism in sleepers was recorded with protrusion of the lower jaw by 25% and 75%, respectively, which only proves the key importance of airway patency for the prevention of bruxism. It is important to note that traditional occlusal stability splints may have a negative impact in the treatment of sleep apnea sleep bruxers. A prospective study of 10 patients with mild to moderate obstructive apnea with and without a stabilizing splint found the following results: six out of ten patients had a significant increase in the apnea/hypopnea index. In addition, patients with obstructive apnea who wore complete dentures were found to have significantly better airway patency when the dentures were worn at night compared with the results obtained when the dentures were removed from the mouth at night. Studies have found that in patients with obstructive sleep apnea, improved airway patency is observed in cases where the lower jaw is in a more protrusive position. Conditions that make it difficult to achieve this jaw position significantly worsen airway patency and increase the number of episodes of bruxism during sleep. This may explain the level of wear on the surfaces of occlusal splints in night bruxists. It was also noted that in patients with difficult airways and GERD, wear rates of orthopedic devices were significantly higher, regardless of their design (photo 10 and photo 11).
Photo 10. Extensive wear of the occlusal tray. It has been suggested that signs of aligner wear are a pathognomonic symptom of progression of the bruxism triad.
Photo 11. Long-term wear of aligners during parafunction does not depend on the features of their design.
GERD may also be associated with other elements of the triad. Patients with GERD had higher apnea/hypopnea index scores and shorter periods of second stage sleep. Research has also shown that more severe stages of sleep apnea are accompanied by more severe stages of GERD. Although the issue remains controversial, the fact remains that during an episode of apnea, negative intrathoracic pressure increases, which can lead to regurgitation of stomach acids into the esophageal space. When the pH of the esophagus decreased, episodes of bruxing occurred significantly more often in patients. Miyawaki studied 10 night bruxers with GERD and 10 controls without GERD. The pH of the esophagus was monitored even during sleep, which made it possible to record the following data: when the pH of the esophagus was 4 or lower, episodes of bruxing began, which were resolved by a tonic impulse and the act of swallowing. Apparently, this reflex is an attempt to buffer the acidic contents of the stomach that have entered the esophagus. Interestingly, the pH threshold of 4 was reached exclusively in patients suffering from nocturnal bruxism. In the control group, esophageal pH did not reach a low enough level to trigger an episode of parafunction.
Proton pump inhibitors are a group of medications that reduce the production of stomach acid. The use of these drugs by patients with GERB reduced the frequency of bruxism episodes in 40% of cases. Other drugs that relieve GERD are H2-histamine blockers, when taken by patients, a decrease in respiratory disorders, symptoms of daytime sleepiness and other related disorders was observed. However, the apnea/hypopnea index did not decrease. Reducing intrathoracic pressure by providing positive continuous airway pressure reduces clinical signs of GERD in patients with and without bruxing symptoms. Studies using mandibular advancement devices have reported similar results, further supporting their positive effect on airway management.
Diagnosis of the bruxism triad in patients
The dentist must be able to diagnose signs of bruxism in a patient of any age category. Early diagnosis will help ensure normal development of the body, improve physical well-being and reduce the level of tooth wear. Below are some distinctive aspects of diagnosing parafunction in different age groups.
Children's period – 3-12 years
Hypertrophy of the adenoids and tonsils provokes sleep disturbances, including obstructive apnea syndrome. The degree of hypertrophy causing obstruction is somewhat greater for children with obesity than for children without it. GERD can often be diagnosed in children with adenotonsillar hypertrophy and obstructive sleep apnea. Five-year-old children with obstructive apnea also exhibit characteristic differences in growth, which is caused by individual characteristics of the posterior inclination of the mandible, anterior facial height, and the degree of retroinclusion of the incisors (photo 12).
Photo 12. The triad of bruxism in childhood: erosive and attrition wear of primary teeth, narrowing of the dental arches, class II deep bite. The examination revealed symptoms of GERD in combination with enlarged adenoids and tonsils.
Adolescence - 13-19 years old
Dentists usually explain to parents how most children outgrow bruxism when they reach puberty, overcoming problems associated with adenoids and tonsil hypertrophy. At the same time, thanks to orthodontic treatment, the palate area expands so much that it ensures sufficient patency of the upper respiratory tract. Any signs of pathological tooth wear are most likely associated with sleep disturbances, reflux symptoms and bruxism, as the last link in the pathophysiological mechanism (photo 13).
Photo 13. Triad of bruxism in adolescence: abrasion of the anterior teeth in a 16-year-old patient with changes in the surface of the teeth due to erosion and abrasion. The history indicates the presence of a triad of bruxism.
Youth age – 20-40 years
Pathological tooth wear or relapse of orthodontic treatment is usually resolved with the help of an occlusal guard. The wear of the mouthguard itself is a direct sign of the progression of the bruxism triad. The results of the analysis of possible stress factors, internal discomfort and tension due to sleep disturbances must also be taken into account. Signs of GERD can be found on the teeth or in the roof of the mouth. Bruxism in such cases may be a protective reflex to ensure airway patency (photo 14). There is a statistically significant relationship between the wear of primary molars and canines in youth and the level of wear of all teeth over a subsequent 20-year period (Figure 15). For bruxers with occasional sleep disturbances and reflux symptoms, researchers recommend using an anterior jaw repositioning splint, which can provide fairly successful results. It should be remembered that splints that provide protrusion of the lower jaw by no more than 40% guarantee a much lower risk of occlusal disorders than those that position the lower jaw in a more protrusive position (photo 16 and photo 17). The maxillary orthopedic device ensures airway patency due to the protrusive position of the lower jaw, but is not as bulky as most devices of similar action.
Photo 14. Bruxism triad in a young adult: pathological tooth wear has spread from the area of the front teeth to the area of the lateral teeth. The patient reported sleep problems that worsened along with symptoms of GERD during pregnancy.
Photo 15. Increased wear of the patient's primary molars increases the risk of bruxism in adulthood. Narrowing of the dental arches, crowding of the front teeth of the lower jaw and deep bite provoke problems with the airway. History of GERD in combination with erosive wear of teeth.
Photo 16. The plane of the orthodontic aligner demonstrates the path of disposition of the anterior teeth from the central to the anterior position.
Photo 17. Jaw protrusion by 40%.
Average age – 40-65 years
At this age, the symptoms of bruxism begin to subside, but the risk of obstructive apnea increases. Signs of dental attrition appear less during this period, but the risk of complications of sleep apnea/hypopnea syndrome and GERD steadily increases. Symptoms of age-related dental aging and damage to existing dental restorations may also occur. Relieving respiratory problems becomes a more complex process, given the physical changes in the body in middle age (photo 18). According to the literature, airway management during sleep improves all factors of the bruxism triad. Treatment by providing positive airway pressure is the gold standard, but for patients who are unwilling to accept this algorithm, mandibular protrusion orthoses can be manufactured as their potential effect can reduce the level of apnea/hopopnea index, signs of bruxism, sleep disturbances and symptoms GERD (photo 19 and photo 20).
Photo 18. Middle-aged patient: pathological abrasion due to bruxing during sleep and erosive damage to the surfaces of the teeth. GERD was treated with proton pump inhibitors. The patient reported a decrease in signs of bruxism, but symptoms of snoring and apnea increased. As a result of polysomnography, the AHI was determined to be 34.
Photo 19. Thornton 3 Adjustable Positioner (APT), custom made for the treatment of sleep disorders. The front connector allows for airway control.
Photo 20. Fixed position of the Thornton adjustable positioner.
Mature age - 65 and older
Most patients in adulthood usually have a moderate degree of sleep apnea, and most medical aspects related to general health can be directly associated with obstructive sleep apnea. Bruxism as a protective mechanism may manifest itself in some changes, but in essence it no longer provides the necessary airway patency and a compensatory reduction in the signs of GERD by activating the act of swallowing. Patients at this age have to deal with pathological tooth wear, which arose due to the chronic action of provoking factors over a long period of time (photo 21 and photo 22). A comprehensive assessment of signs and symptoms of obstructive sleep apnea and polysomnographic studies are mandatory at this age. Patients with dentures and sleep disorders should be encouraged not to remove their dentures at night, since then the signs of the triad are less pronounced (photo 23 and photo 24).
Figure 21. An elderly patient with signs of the bruxism triad: a history of long-term symptoms of bruxism, snoring, interrupted sleep, and GERD. The results of a sleep study indicate the presence of severe apnea.
Photo 22: Appearance of the incisal edge as a result of abrasion due to bruxism and erosive wear due to the presence of GERD.
Photo 23. The position of the tongue in edentulous patients limits the airway (view with a retractor). Wearing dentures at night helps achieve better airway patency.
Photo 24. On many dentures, wear facets can be found, indicating the presence of the bruxism triad. For a detailed diagnosis, it is necessary to analyze the symptoms of bruxism, sleep disturbances and signs of GERD.
conclusions
During this analysis, it was found that although the majority of dental patients suffer from pathological tooth wear, only a very special group of patients can be called bruxists. Bruxism in sleepers is caused by micro-awakenings, which can be either natural or triggered by obstruction of the airway or a significant decrease in the pH of the esophagus. The bruxism triad is one of the concepts that attempts to explain the close relationship between bruxism, breathing and the erosive factor of acidity. Night bruxers suffer from pathological tooth wear due to increased friction of antagonist surfaces due to insufficient amounts of lubricant (saliva) and surface roughness caused by acids. A comprehensive diagnosis of such patients is mandatory in order to prescribe in the future the most effective treatment option, taking into account the possibility of providing positive pressure in the space of the upper respiratory tract, protrusion of the lower jaw with the help of orthopedic equipment and pharmaceuticals that relieve symptoms of GERD.
Author: Jeffrey S. Rouse, DDS
Features of the disease in adults
The symptoms and causes of bruxism in children and adults are very similar. Older patients also experience jaw weakness and pain in the morning, and their teeth become worn and damaged. The problem also manifests itself in the form of constant bleeding of the gums.
If the causes of bruxism are not identified, dental treatment in adults often becomes impossible. Dentists do not recommend installing crowns or dentures - they will increase friction in the mouth, and the impact on the opposite jaw will increase significantly, which will lead to even faster destruction of a healthy tooth.
To avoid bruxism, you need to control your emotional state and promptly get rid of dental problems and ENT diseases. During nervous work, it is advisable to take light sedatives that do not affect the functioning of the nervous system: valerian, Persen, Patrimil, Herbion, Sedavit, Afobazol. If you have to deal with premature tooth loss, you need to place an implant so that the chewing load is distributed evenly.
What is bruxism?
Bruxism is the medical term for the habit of teeth grinding.
Most people grind their teeth from time to time, which usually does not cause any harm, but when it becomes a habit and occurs regularly, the habit can cause permanent damage to the teeth. It can also cause headaches, ear pain, and jaw discomfort in some people.
Teeth grinding usually occurs subconsciously during sleep. For most people, stress and anxiety are contributing factors to bruxism.
Types of Bruxism
Bruxism is often classified as:
- Wake-up bruxism , where you habitually clench your teeth and jaw while awake (but typically don't grind your teeth). Most will do this subconsciously through concentration.
- Sleep bruxism is when you subconsciously grind your teeth against your teeth and clench your jaw muscles while you sleep. Partners may hear an unpleasant grinding or knocking noise that may irritate them.
Bruxism is also divided into:
- primary bruxism , which occurs without any underlying disease;
- secondary bruxism , which is caused by another condition such as depression or anxiety, treatment with medications such as antidepressants, or drug use such as cocaine and ecstasy.
How common is tooth grinding?
It is not known exactly how many people have bruxism, but up to 8-10% of the population suffer from it at some point in their lives.
It can occur in both children and adults, but is most common in adults aged 25 to 44 years.
It is estimated that up to 15-33% of children grind their teeth, although the habit tends to stop once their adult teeth are fully formed. For most children, the habit develops during growth and does not have long-term effects.
It is believed that stress and anxiety cause teeth to grow more often or worse during sleep. Bruxism is also more common in people who regularly drink alcohol, smoke tobacco, or drink caffeine (more than six cups per day).
Who is most at risk?
You are more likely to suffer from bruxism if you:
- lead a busy lifestyle;
- drink large amounts of alcohol;
- smoke;
- take medications for sleep, depression, or anxiety;
- drink six or more cups of tea or coffee a day;
- have sleep apnea, snore, or talk in your sleep.
How to treat Carolini syndrome?
In the vast majority of cases, treatment of bruxism in children comes down to normalizing the daily routine, improving the quality of nutrition and correcting the emotional state.
Psychological help
Children of any age are limited from watching movies, cartoons and TV shows, and their time using the computer and other gadgets is reduced. It is useful to increase the time spent outside, especially during daylight hours. To the mandatory daytime walk, a daily walk is added 1-2 hours before bedtime (duration from 30 minutes to 1 hour).
Psychological assistance to a child
To improve the psycho-emotional state of a child, art therapy, audio therapy, aromatherapy, and relaxing massage are useful. Contacts with people who cause the child to feel internal rejection, constraint and anxiety must be limited. If parents often spend time visiting or in crowded places and take their child with them, it is better to avoid such trips for a while.
In the case of daily chronic stress due to conflict situations, it is extremely important to identify the source of the conflict and help the child find a way out of the current situation. In some cases, this may require working with a psychologist, and in order to achieve a stable positive response, the situation is studied simultaneously with all parties to the conflict.
Child psychologist
Other methods of relaxation and normalization of psycho-emotional status include the following types of treatment:
- hypnosis treatment;
- acupuncture (a type of reflex effect on the body with the aim of relaxing muscles and stimulating biologically active points);
- psychotherapy.
Among medications, it is permissible to use plant-based sedatives (Tenoten, Novopassit, Persen). Heavier medications (psychotropic drugs, antipsychotics) are prescribed strictly by the attending physician.
"Tenoten"
Note! For mild to moderate psycho-emotional disorders in childhood, soothing herbal infusions help well. Every day it is useful to give your child a decoction of chamomile and thyme, as well as an infusion of oregano, calendula and valerian (1 glass 2-3 times a day).
Oregano infusion
Dental treatment
Dental treatment of bruxism includes the elimination of existing defects and pathologies in the oral cavity: correction of the bite using orthodontic structures, grinding of sharp edges and uneven surfaces of the cusps, treatment of caries, periodontitis and periodontitis. It is also important to check the already installed seals and, if they are deformed, replace them in a timely manner.
One of the measures for dental correction of odonterism is wearing a special mouth guard. This is a device in the form of a toothbrush, which is made of soft and flexible plastic individually taking into account the anatomical characteristics of the patient. The mouth guard is worn over the upper teeth while sleeping at night and prevents their interaction with the lower jaw, preventing deformation and abrasion of the enamel.
Mouth guards for bruxism
Important! Dental guards help cope with the manifestations of bruxism, but they do not eliminate the cause of its occurrence, so treatment at the dentist is always supplemented by consultation with specialized specialists to diagnose existing pathologies and correct them.
Mouth guards for bruxism
Drug correction
Medications are necessary to normalize the tone of the facial muscles. The treatment regimen for each child is selected individually; a standard course of therapy usually contains the following drugs:
- calcium and magnesium preparation;
- muscle relaxants;
- preparations containing B vitamins;
- mild sleeping pills;
- sedatives (mainly herbal based);
- tranquilizers (only in severe cases);
- Botox injections (only for adolescents over 14 years old with strict indications).
Muscle relaxants
The treatment regimen may additionally include drugs necessary to treat the provoking disease, for example, osteochondrosis or neurological disorders.
Symptoms
If a child begins to grind his teeth in a dream, parents begin to look for possible signs of illness. It is important to understand the variety of symptoms. Among the main ones, experts identify the following symptoms of bruxism:
- There are severe headaches in the morning after waking up.
- Children may experience ringing in the ears or complain that their ears feel blocked.
- Your back or neck may hurt in the morning.
- Many children experience sleep disturbances and loss of appetite.
Negative consequences include rapid wear of teeth, damage to enamel , causing caries, and malocclusion and subluxation of the jaw become a common complication.
The most dangerous consequence is the potential for stopping breathing during sleep. It can occur when a child clenches his or her teeth tightly during sleep. In some cases, the child may begin to suffer from somnambulism, that is, walk in his sleep.
Such a wide range of symptoms shows the difficulty of clearly identifying which doctor treats this condition. The first step in solving the problem for each parent is to contact the treating pediatrician. An experienced doctor will examine the child and identify the probable cause of the teeth grinding.
Next, the little patient will be sent to a specialist:
- If the problem is caused by a malocclusion, your dentist will determine treatment options.
- In case of psychological disorders, therapy will be determined by a psychologist.
- In some cases, teeth grinding can become a symptom of complex neurological disorders . For example, muscle spasm that causes bruxism may accompany cerebral palsy or mental retardation. Depending on the type of cause diagnosed, the young patient may be referred to a neurologist or psychiatrist.
After a consultation, a treatment method is determined that will help reduce nighttime bruxism in a child, regardless of the underlying cause.
Doctors pay attention to the high likelihood of such manifestations occurring in hyperactive children. Such babies often begin to sit and walk earlier than their peers.
In this case, the pediatrician may prescribe calming herbal remedies for the little patient. The method is recommended for children who are at least three years old. For infants, sedatives can be recommended only if there is a high need to choose this particular method of treatment.
Reasons for development
Doctors point to the following factors leading to involuntary teeth grinding:
- the presence of braces - the child can strongly clench his jaw due to discomfort while wearing the devices;
- period of teething;
The period of teething is one of the likely causes of bruxism in children.
- severe stress or emotional stress;
- anomalies in the location and structure of teeth: supernumerary rows, malocclusion;
- neurological disorders.
Classification of bruxism
The pathological condition is usually divided into 2 types:
- daytime type - appears during emotional overstrain;
- nocturnal type - clenching of teeth occurs involuntarily.
The greatest difficulty is the nocturnal attack of bruxism, since the child cannot control his condition during sleep.
In addition, a distinction is made between noisy (with grinding) and quiet (with squeezing) bruxism. In the first case, the creaking is accompanied by a characteristic sound. In the silent form of the pathology, teeth clenching occurs silently. Sometimes mixed bruxism occurs.