A number of periodontal diseases occur with characteristic
clinical signs. The main task of the doctor is to make an accurate diagnosis, on the basis of which treatment will be prescribed to the patient. From this review, you will learn about the features of dystrophic and inflammatory periodontal diseases, learn to distinguish between them, get acquainted with the main diagnostic techniques used by modern doctors, and find out how accurate they are. With a competent approach, the periodontist makes the correct diagnosis with a 95% probability; problems, as a rule, arise due to medical negligence (and not due to the low quality of laboratory and instrumental diagnostics).
History taking
Taking an anamnesis when diagnosing periodontal disease includes:
- Survey (collection of complaints).
- Dental examination to assess the condition of the jaw system.
- Determination of local factors that may contribute to the development of the disease.
- Identification of common causes of pathology (additional examinations may be required, including from related specialists).
Children usually do not complain about anything other than pain. In the case of periodontal pathologies, you need to ask specific questions about bleeding gums, bad breath, dryness, etc.
Also, when collecting anamnesis, it is necessary to take into account the child’s developmental characteristics, previous history, concomitant diseases of systems and organs, and medications taken. The hereditary factor, bad habits, timing of teeth changes, and the nature of chewing and breathing are taken into account. The doctor must find out exactly when the first signs of the disease made themselves felt, how the pathology proceeded, whether there were improvements or deterioration.
The patient must tell the specialist how he was treated and whether such therapy gave the required results.
Schiller test in dentistry. Functional tests
> Family
Periodontal diseases are widespread, so it is necessary to use advanced methods to make the most accurate diagnoses and differentiate one pathology from another.
For this reason, various periodontal indices have been developed that make it possible to monitor the dynamics of pathology development over a given time period, assess the prevalence and depth of the pathological process, and compare the effectiveness of different treatment methods.
In this review we will talk about this method of research as the Schiller-Pisarev test, its advantages, disadvantages and features.
Methods for clinical and epidemiological assessment of periodontal condition
RMA index. — Schiller-Pisarev test. — Gingival index GI. — Communal periodongal index CPI. — Complex periodongal index KPI. — Gum recession index. — Gingival attachment loss index. — Diagnosis of risk factors for the development of periodontal pathology and drawing up a plan of preventive measures.
When assessing the condition of the periodontium using visual and tactile methods, pay attention to the condition of the gums (color, size, shape, density, bleeding), the presence and location of the periodontal junction relative to the enamel-cementum border (i.e., the presence and depth of pockets), on tooth stability.
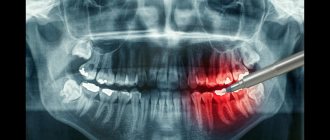
For more detailed studies of the condition of the periodontium, radiography is used (parallel technique, orthopantomogram, tomogram), electronic devices are less often used to determine the degree of tooth mobility, and diagnostic bacteriological tests are performed (see below). In periodontological practice, a special card is filled out, in which the degree of pathological changes in the area of each tooth is recorded during the initial examination of the patient, and the dynamics of the condition during treatment are noted.
To standardize and simplify registration records produced for clinical and epidemiological purposes, in our country and in the world it is common to use gingival and periodontal indices, which more or less fully describe the condition of the entire periodontium or its “sign” areas.
Schiller-Pisarev test
Designed to clarify the boundaries and degree of inflammation using vital tissue staining.
During inflammation, glycogen accumulates in the tissues, the excess of which can be detected by a qualitative reaction with iodine: a few seconds after the application of an iodine-containing preparation (most often this is Schiller-Pisarev solution), the tissues of the inflamed gums change their color in the range from light brown to dark brown. depending on the amount of glycogen, i.e. on the severity of inflammation.
The sample can be assessed as negative (straw-yellow color), weakly positive (light brown color) or positive (dark brown color).
This test cannot be used to diagnose periodontal pathology in children under 6 years of age, since their healthy gums contain a large amount of glycogen.
Gingival index GI (Loe, Silness, 1963)
The index involves assessing the condition of the periodontium based on clinical signs of gum inflammation - hyperemia, swelling and bleeding when touched with an atraumatic probe in the area of six teeth: 16, 21, 24, 36, 41, 44.
The condition of four areas of the gums near each tooth is studied: the medial and distal papilla on the vestibular side, the edge of the gums on the vestibular and lingual sides.
The condition of each section of the gum is assessed as follows: 0 - gums without signs of inflammation; 1 - slight discoloration, slight swelling, no bleeding during examination (mild inflammation); 2 - redness, swelling, bleeding during examination (moderate inflammation);
3 - severe hyperemia, edema, ulceration, tendency to spontaneous bleeding (severe inflammation).
GI for the periodontium of one tooth as an average value calculated from data on the condition of each section of the gum:
If we sum up all the GI values of the teeth and divide by the number of teeth examined, we obtain the GI value of the examined individual:
Interpretation: 0.1-1.0 - mild gingivitis; 1.1—2.0—moderate gingivitis;
2.1-3.0 - severe gingivitis.
Which specialist should I contact?
Periodontal diseases are dealt with by a periodontist - he has sufficient knowledge, experience, special equipment and research tools, so he can make an accurate diagnosis.
If there is no periodontist in the district clinic or private medical institution in your area, you can contact a general dentist. He will also be able to examine the oral cavity, identify characteristic symptoms and make a diagnosis. Carrying out additional research (samples, x-rays, etc.) in most cases is mandatory. They can be used separately or complement each other.
Diagnostic methods
Let's look at the main techniques used to diagnose periodontal diseases.
Schiller-Pisarev test
The Schiller-Pisarev test is used in dentistry to determine the intensity of the inflammatory process in the gums. To do this, the gums are lubricated with a solution containing 1 g of crystalline iodine, 2 g of potassium iodide, 40 ml of distilled water.
Completely healthy gums turn yellow with a straw tint, while inflamed gums turn brown. Taking into account the degree of the inflammatory process, the shade can be light beige, normal or dark brown.
Sample Parma
The Parma test (benzidine) allows you to accurately determine the amount of pus in periodontal pockets. Its main principle is to change the shade of the reagent when interacting with purulent contents.
For this purpose, a drop of a 3% peroxide solution is mixed with a drop of a solution of benzidine, polyethylene glycol, acetic acid, and the mixture is injected into the pocket on a turundum. The cotton wool begins to turn blue, bluish-green or green, depending on the nature of the purulent exudate.
Aldrich blister test
The blister test is used to determine the degree of tissue hydrophilicity, as well as to diagnose hidden edema of the oral cavity. It is based on the difference in the rate of resorption of an isotonic sodium chloride solution introduced into the tissue. 0.2 ml of the product is injected with a thin needle under the epithelium of the mucous membrane of the lower lip, gum or cheek until a transparent bubble appears.
Normally, this bubble should resolve within an hour; if this period is shorter, we can talk about increased tissue hydrophilicity, and if it is longer, we can talk about decreased tissue hydrophilicity.
The Aldrich blister test can be single or multiple, but to obtain accurate data, it is recommended to do several bubbles at the same time.
The blister test determines the sensitivity of tissues to histamine (a component involved in various allergic reactions). The technique is based on the relationship between the size of the histamine papule and the histamine content in the blood. In this case, papules are measured on the forearm - the norm is 5 mm, the redness area can be up to 20 mm.
Fedorov-Volodkina Index
The Fedorov-Volodkina index determines the presence of plaque on the teeth of the lower and upper jaws. The sum of points obtained when studying the condition of each tooth is divided by the number of teeth. Results:
- 1.1-1.5 points – good hygiene;
- 1.6-2.0 points – normal hygiene;
- 2.1-2.5 points – unsatisfactory care;
- 2.6-3.4 – poor oral hygiene;
- 3.5-5 points – very poor care.
Orthopantomography
Reduced radiation exposures make it possible to obtain enlarged images of all parts of the dentofacial apparatus. If the study conditions are met, identical images are obtained that are necessary to assess the effectiveness of the activities being carried out.
To assess the condition of the dental system, you will need to make at least 8 contact intraoral orthopanotomograms of the teeth.
Echoosteometry
Ultrasound osteometry (or echo-osteometry) is a technique for quantitatively assessing the physiological state of bone tissue density by measuring the time it takes for ultrasound vibrations to pass through the area being studied. In dense environments, sound travels quite quickly, and vice versa. Echoosteometry is very sensitive to changes in the saturation of bone tissue with minerals, therefore it provides objective information about bone density indicators and allows one to evaluate its mechanical properties in the area under study.
Schiller-Pisarev and Kulazhenko test: used for determination and carried out for the purpose of solution
Periodontal diseases are widespread, so it is necessary to use advanced methods to make the most accurate diagnoses and differentiate one pathology from another.
For this reason, various periodontal indices have been developed that make it possible to monitor the dynamics of pathology development over a given time period, assess the prevalence and depth of the pathological process, and compare the effectiveness of different treatment methods.
In this review we will talk about this method of research as the Schiller-Pisarev test, its advantages, disadvantages and features.
Differential diagnosis
The main differential diagnostic symptom of gingivitis is the absence of changes in the bone base of the periodontium. The severity of gingivitis is determined taking into account the totality of changes occurring in the body and the involvement of gum tissue in the pathological process.
Severe ulcerative and chronic catarrhal gingivitis is characterized by damage to the interdental gums, moderate - marginal and interdental, and severe - the entire gum, including the alveolar. Moderate hypertrophic gingivitis is accompanied by severe gingival hyperplasia - up to a third in mild cases, up to half in moderate cases and more than half in severe cases.
Differential diagnosis of catarrhal, hypertrophic, chronic gingivitis is associated with the commonality of the clinical picture - all patients complain of severe bleeding and changes in the gingival margin. The poroliferative process in hypertrophic gingivitis is usually preceded by catarrhal inflammation, which is why the signs on the jaws may be different. The differences lie in the difference in general somatic diseases - catarrhal gingivitis is caused by pathologies of the heart and blood vessels, gastrointestinal tract, blood, hypertrophic gingivitis is caused by hormonal changes.
Differential diagnosis of ulcerative-necrotic type gingivitis and generalized periodontitis lies in the difference in unique symptoms. In both cases, the patient complains of weakness, there are signs of intoxication, the gums become swollen and red, and pain appears in the oral cavity. In this case, with ulcerative necrotic gingivitis, there will be a gray coating on the edge of the gums, and the papillae may die. Removing plaque is painful and may cause bleeding. With periodontitis, pockets are formed, often with purulent contents, the transitional fold is smoothed, and fistulas may appear. There will be no changes in bone tissue on an x-ray only with ulcerative necrotizing gingivitis.
You also need to be able to distinguish generalized chronic gingivitis from generalized periodontitis . Common complaints are bleeding gums, hyperemia of the gums, swelling, formation of soft plaque and hard stone, high indices of IH, RMA, positive Schiller-Pisarev test. Differences - with periodontitis, periodontal pockets will be identified, usually there is resorption of bone tissue of the interalveolar septum.
Functional methods - rheoparodontography, polarography - are powerless in differential diagnosis.
A differential diagnosis of hypertrophic localized gingivitis and epulis is mandatory. General signs are proliferation of the gums in a small area (area of 1-2 teeth). The shape of the tumor is mushroom-shaped or leaf-shaped, the color is bright red, with bluish or brown tints, and there is a rarefaction in the bone tissue at the stem of the epulis. Localized periodontitis affects no more than 5 teeth, generalized periodontitis occupies a larger area. Chronic periodontitis in most cases is preceded by hypertrophic or catarrhal periodontitis for several years. The degree of severity is determined taking into account bone resorption, the depth of the periodontal pocket, and pathological mobility of teeth.
Acute or aggravated chronic periodontitis and acute periodontitis are differentiated as follows. General points - the patient’s general condition worsens, soreness of individual teeth develops (increases when clenching the jaw, eating food), swelling of the mucous membrane, hyperemia becomes noticeable, and an infiltrate or abscess may develop. But with periodontitis, abscesses periodically appear in different areas, are single in nature, follow each other with an interval of 5-7 days, are located at the edge of the gums and do not overlap with the periodontal pocket. Such abscesses are combined with a fistulous tract; X-rays reveal resorption of bone tissue of the alveolar processes with a pronounced predominance of vertically located pockets.
The differentiation of generalized chronic periodontitis from periodontal disease, which is complicated by inflammation, is determined by the commonality of some symptoms. Among them are hyperemia, swelling of the gums, the presence of periodontal pockets, plaque, tartar, sometimes discharge comes out of the pockets, the teeth become mobile. The difference is that with periodontal disease there will be areas of retraction of the gingival margin without periodontal pockets; there are almost always wedge-shaped defects. X-ray shows a mixed type of resorption, the bone pockets are vertical, shallow, and there are areas of horizontal atrophy.
Let us consider the principles of differential diagnosis of hyperesthesia in chronic pulpitis and periodontitis. General signs are sensitivity to thermal irritants, prolonged pain. In case of periodontitis, only exposed cement will be detected, most often in multi-rooted teeth; in case of pulpitis, carious cavities are present, masked by a swollen gingival papilla.
Differential diagnosis of generalized chronic periodontitis and eosinophilic granuloma is based on the commonality of the following symptoms - mobility of a pair of premolars, two or three molars, bleeding gums, the presence of periodontal pockets. Differences - with eosinophilic granuloma there is no local cause, there is no purulent discharge in the periodontal pockets, the pathological process itself takes up to two months, x-rays show resorptions of a clear rounded or oval shape.
Differential diagnosis of periodontal disease and involutive processes is based on the commonality of retraction of the gingival margin, tooth mobility, and bone resorption. Differences - in old age, the retraction of the gingival margin is often uneven, as is the mobility of the teeth; pathological abrasion of the enamel of varying severity may develop. There is no focal, diffuse osteoporosis localized in the alveolar process of the jaws.
When performing differential diagnosis of periodontal pathologies, it is necessary to take into account blood diseases, tuberculosis, and syphilis. At the moment, a number of research methods are known that are used in periodontal diseases, most of them are functional.
Schiller test: how they do it, decoding | University Clinic
Many diseases of the female reproductive organs are asymptomatic, especially in the early stages. Some of them can be detected using the Schiller test performed during colposcopy.
Therefore, the main way to timely detect and successfully treat gynecological pathologies is preventive diagnostics. It includes a whole range of measures (laboratory tests, ultrasound of the pelvic organs, gynecological examination), which allows you to assess the health of a woman’s genitourinary system.
One of the mandatory elements of preventive diagnostics in gynecology is the Schiller test, which allows you to detect pathological areas of tissue indicating the development of the disease.
Indications for the test
The procedure is recommended for all women of reproductive age once a year. Patients who are at increased risk should undergo the Schiller test twice a year.
Women during menopause, after miscarriages and surgical abortions, sexually transmitted diseases, and with a family history of various gynecological pathologies should monitor their sexual and reproductive health more closely.
An indication for an extraordinary procedure is suspicion of genital cancer, cervical dysplasia, HPV, sexually transmitted infections, colpitis, vulvitis and other gynecological pathologies, which are accompanied by the following alarming symptoms:
- pathological vaginal discharge (with blood, pus, unpleasant odor, etc.);
- menstrual irregularities (delays, profuseness, scarcity, pain, etc.);
- pain and bleeding during sexual intercourse:
- rashes in the genital area (hyperthermia, ulcers, erosions);
- itching in the external genital area;
- problems with pregnancy and bearing a baby.
DischargeItching of the genitalsIrregularities in the menstrual cycle
The Schiller test is a mandatory procedure during or preparation for in vitro fertilization.
Features of preparation
The reliability of the results of a colposcopic examination using the Schiller test largely depends on the quality of preparation for the procedure. Gynecologists recommend paying attention to the following areas of life:
- Sexual contacts - you must refuse sex 2-3 days before your appointment with the gynecologist. Substances that are released during sex can affect the results of the procedure due to disruption of the natural vaginal microflora;
- Intimate hygiene - before visiting a gynecologist, it is enough to wash the external genitalia with clean water. Douching, intimate gels, lubricants, creams, deodorants, and any other cosmetics can change the composition of the sexual microflora;
- Nutrition – a few days before your doctor’s appointment, follow a light diet, give up flour, sweets, and foods that increase gas formation. This will make you feel light and confident during your visit to the doctor;
- Bad habits - give up alcohol and smoking a day before the procedure. Excess of harmful substances and toxins in the body can also distort the results of the procedure;
- Medications – 2 days before the study it is necessary to avoid taking medications. Antibiotics and hormonal drugs should be stopped at least a week in advance;
- Physical and emotional stress affects the state of the body and can negatively affect the results of iodine staining.
The planned procedure is carried out in the first 3-7 days after the end of menstruation. This period is most favorable for detailed study and targeted identification of even minor transformations in the structure of tissues and mucous membranes.
Schiller test procedure
During extended colposcopy, the gynecologist performs the Schiller test. The uterus and vagina are first cleaned of excess mucus and secretions using sterile tampons. Next, the specialist exposes the cervix using special gynecological mirrors.
Using a sterile swab, an iodine solution (2-3%) is applied to the areas of the genital organs (usually the cervix) that need to be examined. The cervix should be completely immersed in the solution. After complete immersion, the solution is removed and the uterus is dried with cotton swabs.
Within a few seconds, the epithelium turns brown, and the doctor can conduct an examination.
Schiller test
In the process of examining stained areas under a microscope, the doctor evaluates the uniformity of color, structure, color of the epithelium, mucous membranes, the nature of vascular patterns, and the general reaction of the tissue to the contrast agent.
Multiple optical zoom allows you to see the most minor changes and identify atypical cells in the tissues of the vagina, uterus, and cervix. If iodine-negative lesions are identified, the gynecologist examines them in detail: recording the area, quantity, contours, and localization.
This is necessary for reliable conclusions about a possible disease.
The procedure is absolutely safe, painless, does not cause discomfort and takes no more than 10 minutes.
The study has virtually no contraindications (individual iodine intolerance, postoperative period) and is easily tolerated by patients.
The test is highly informative and reliable, since it allows one to suspect malignant transformation and severe inflammatory processes at an early stage.
After the procedure, brown vaginal discharge may be observed for several days. Gynecologists consider this to be the norm - the body is simply cleansing itself of excess iodine. To avoid damaging your underwear, use panty liners.
Interpretation of results: transcript
Examination of the colored areas under a microscope allows a specialist to draw the following conclusions:
- The uniform dark brown color of the treated areas indicates that the patient is healthy. In this case, the Schiller test is assessed as positive;
- Uneven color, various light spots, spots, specks, unpainted segments indicate the presence of gynecological problems. For example, with atrophic vaginitis, uneven coloring and light areas indicate the development of an inflammatory process. If there are suspicious areas, the sample is assessed as negative. A negative test is typical for diseases such as human papillomavirus, cervical erosion, leukoplakia, genital oncology, and precancerous conditions.
A negative Schiller test indicates the need for a comprehensive examination of the patient using laboratory and instrumental techniques. Comprehensive diagnostics is necessary to clarify the diagnosis, draw up an effective treatment regimen, and minimize possible complications and risks.
In a modern medical facility, you can undergo a comprehensive gynecological examination with a Schiller test in comfortable conditions. High-tech equipment for clinical diagnostics and the experience of our specialists guarantee fast and reliable results. Take care of your health today with the University Clinic!
link:
Source: https://unclinic.ru/proba-shillera-pri-kolposkopii-zachem-provoditsja-i-chto-vyjavljaet/
Possibility of medical error
Using clinical and laboratory indicators, a set of differential and diagnostic criteria, the doctor will be able to make an accurate diagnosis, avoiding the most common mistakes that specialists make when diagnosing periodontal diseases.
At the stage of planning the research scheme, it is possible and necessary to give a prognosis of the disease - in general for the oral cavity and individual teeth. Please note that the prognosis of mild to moderate periodontitis and chronic gingivitis does not cause difficulties in older people, but is not always obvious when making a diagnosis in young women and men, and adolescents. Aggressive, severe forms of the disease are always difficult to predict.
Medical error when making a diagnosis cannot be completely excluded, but a competent approach can reduce it to a minimum.