Indications for use
Lidocaine is a popular local anesthetic and antiarrhythmic agent. It is a transparent, colorless, odorless liquid. The drug is used for all types of local anesthesia (injections, applications, irrigation, drops), as well as as part of the complex treatment of heart diseases.
Lidocaine can be produced in the form of:
| Release form | Application area |
| Ampoules | The main area of application of ampoules (2%) is all types of dental procedures requiring pain relief. Also, compositions of this concentration are sometimes used for simple surgical operations, when local anesthesia is sufficient, and in otolaryngology during painful examinations. Ampoules (10%) required:
|
| Spray | Can be used in dentistry for simple operations on the oral mucosa. It is used in therapy:
|
| Drops | Anesthesia with eye drops is a practice used in ophthalmology when it is necessary to:
|
| Adhesive sheets or patches | They are used for the symptomatic treatment of pain in:
|
Indications and effect of Lidocaine on the human body
This drug is widespread and is used mainly in medical institutions. The mechanism of action of Lidocaine is to block nerve conduction. It is indicated for pain relief during painful procedures or studies. The scope of application of the drug is very wide - it is used in dentistry, for spinal anesthesia during childbirth, suturing, gastroendoscopy, and so on.
For each of these and other procedures, a specific dose with a specific percentage of the active substance is indicated. Thus, a 2% drug is used in dentistry or ophthalmology, and 10% Lidocaine is already considered an antiarrhythmic agent. The drug exists in the form of an injection solution of different percentages, eye drops, anesthetic gel, and spray.
When administered intramuscularly, Lidocaine acts almost instantly. Vasodilation occurs, but irritation does not occur. The rate of absorption depends on the injection site, and the duration of action of the drug depends on the dose. Thus, the effect of Lidocaine administered intramuscularly begins after 5 minutes, intravenously - after 40-60 seconds, applied to the skin - after 15 minutes.
The duration of action depends on the dose of the drug and the percentage of the active substance, and the average half-life of the active components of Lidocaine is 4-5 hours. The dose of the medicine is calculated exclusively by the doctor, and before the first administration of the medicine, the patient is asked about the body’s allergic reactions and is required to undergo an allergy test.
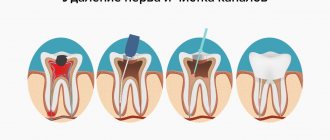
Lidocaine is effectively used in dentistry
Compound
In its original form, lidocaine (white crystalline powder) is poorly soluble in water, so the drug of the same name uses lidocaine hydrochloride as an active component.
This is a water-soluble substance that has the properties of lidocaine and is capable of:
- as an anesthetic: reduce the permeability of the cell membranes of neurons to sodium ions, under the influence of which the neuron enters an excited state. Due to this, the signals received from the receptors located at the site of action of the drug lose their intensity, which is perceived by the person as a feeling of numbness;
- as an antiarrhythmic: increase the absorption of potassium ions by cardiomyocytes, causing a slowdown and normalization of the heart rhythm, thereby eliminating the manifestations of arrhythmia and tachycardia.
An isotonic saline solution (sodium chloride and distilled water) is present in the liquid preparation as an auxiliary solvent. Lidocaine patches contain auxiliary thickeners, preservatives and components that ensure the adhesiveness of the composition.
In what form is it produced?
Lidocaine can be produced in the form of:
- 2 ml ampoules containing 2% lidocaine solution. Each ampoule contains 40 mg of active substance. These can also be ampoules of 2 ml containing a 10% solution of lidocaine (200 mg of lidocaine hydrochloride). Glass ampoules for injection (10 pcs.), having a breaking point and a green code ring, are in 2 mesh blisters (5 pcs. each), placed in a cardboard box. Package price – 28 rubles. (2% solution), 37 rub. (10% solution);
- spray in a plastic spray bottle with a capacity of 38 g (650 doses), placed in a cardboard box. Price – 28 rubles;
- 2% eye drops in dropper tubes with a capacity of 5 ml. Price – 30 rubles;
- plasters. The medicinal composition (lidocaine with the addition of thickeners and adhesive ingredients) is applied to a fabric base and covered with a PET film, which is removed before use. Plasters of 1, 2 or 5 pcs. packed in boxes, price – 50 rub.
Lidocaine in any dosage form is available only by prescription.
Reviews
Alina, Ulyanovsk: “During the entire period of pregnancy and breastfeeding, I had 2 nails removed! Of course, with local anesthesia, a 2% lidocaine solution was used. The doctor convinced me that nothing terrible would happen, the effect of the medicine would end as soon as I felt my leg again. So it happened???? She ran home, fed her doll and fell asleep cuddling until the morning. There is nothing to be afraid of!”
Victoria, Moscow: “I needed urgent dental treatment, otherwise all my gums would simply become infected. My son was 5 months old at the time and was breastfeeding. I just calculated in advance that there would be 2 hours between feeding and injection.”
Pharmacodynamics
Lidocaine is a local anesthetic that provides a short-term anesthetic effect. Pain relief is achieved by temporarily blocking the transmission of signals coming from the area treated with the drug. This is felt by the patient as a feeling of numbness.
The nature of the drug’s action depends on the method of administration: with intravenous injection, 1 minute is enough for kidocaine to exhibit analgesic properties.
The effect lasts for 1 hour. When administered intramuscularly and with superficial local anesthesia, tissues lose sensitivity after about 15 minutes, and it takes about 20 minutes to restore it. Eye drops begin to act within 2-3 minutes, providing an analgesic effect for 5-6 minutes.
Prevention
Prevention to prevent dental pain from occurring should be approached in advance, even at the stage when pregnancy planning occurs.
- A visit to the dentist before conception is necessary because he will perform all necessary oral procedures, including cleaning and stone removal. Questions should be asked regarding oral care during pregnancy, including pain relief for breastfeeding and toothache.
- Visiting the dentist during pregnancy is carried out in the first three months or as recommended by a specialist. Doctors notice that due to changes in the composition of saliva, there is an increased accumulation of plaque in pregnant girls. In this case, you need to use special threads and gels every day.
- It is an incorrect statement that dental treatment is contraindicated during pregnancy because painkillers will have a bad effect on the baby. Caries not only causes toothache during lactation, but also causes infectious complications. The latter leads to deterioration and difficult illnesses. The latest drugs, the use of which is permitted in this process, can help. If you are worried about your teeth, then it makes sense to go to the doctor and have your teeth treated in the first stages.
- Don't forget about the dentist after the birth of your child. You need to come for an appointment for preventive maintenance or have your teeth treated as a priority, so that you don’t waste time and effort on healing later.
A healthy mother is important to a child, who will always help him and will not be exhausted by painkillers for toothache while breastfeeding.
It is important not to forget to think through the details of going to the doctor, especially when you need to treat not ordinary caries on the surface, but rather complex dental diseases.
- Who can be with the child while the mother undergoes dental procedures.
- How long will the mother be away from the baby? You may need milk specially expressed for the next feeding. It is also possible for the mother to pick up the baby together with a relative or other accompanying person. This will be relevant if the dental department is located far from home. This will allow you to feed your baby right before dental procedures. However, there is an unpleasant point: there is a large flow of people in public or private clinics. Because of this, the likelihood of contracting dangerous infections increases. It is better to feed the baby in the car and not bring him to the clinic so that he does not get sick. And the person who accompanies the child goes with the baby when the mother is undergoing dental treatment.
- Often quite serious interference may occur, which is accompanied by complex actions. All this leads to the fact that the mother needs help in terms of caring for the child even after she has returned from the dental clinic. This is also an important point that requires elaboration.
- If you have had a tooth removed or need surgery to remove a cyst, you need to prepare food in advance that will be as gentle as possible. This will not require its preparation later, especially if a nursing mother is unwell after undergoing the procedure for toothache.
| action | possible/not possible |
| use painkillers | Can |
| breast-feeding | Can |
| take ibuprofen and similar medications | Can |
| use aspirin, analgin | it is forbidden |
| take steroids | it is forbidden |
| feed the baby after anesthesia | it is forbidden |
It is not prohibited to use painkillers that contain paracetamol and ibuprofen. It is not necessary to stop breastfeeding or take a break, except in cases where strong anesthesia is used.
Even when the tooth has stopped hurting, you must immediately contact your dentist. Remember, the sooner you see a doctor during lactation, the sooner you can avoid the unpleasant consequences of toothache and its complications.
Since most women suffer from dental problems during pregnancy and breastfeeding, it is necessary to take preventive measures:
- appear in the dental office at least once every two months to treat diseased teeth and prevent their destruction;
- strengthen the gums using rinses based on herbs, mumiyo and minerals, use pharmaceutical pastes;
- do not abuse sweets and baked goods, soda, sour and salty foods;
- eat warm food, avoid scalding and icy foods and drinks (especially alternating them, which contributes to cracks in tooth enamel);
- Maintain oral hygiene, brush your teeth and tongue twice a day, use herbal rinses and dental floss after meals.
A mandatory item for maintaining a healthy mouth and teeth is the introduction of dishes containing large amounts of calcium into the menu.
During breastfeeding, due to hormonal changes, gum bleeding increases and teeth become more sensitive. If you provide the body with support, increase immunity, take care of the oral cavity and eat right, you can prevent pathologies of teeth and gums at the initial stage.
Pharmacokinetics
Depending on the dose of kidocaine received and the characteristics of the body area undergoing anesthesia, the maximum concentration of the drug in the tissues is achieved after 10-20 minutes.
Next, lidocaine is absorbed into the blood. The absorption time is determined by the intensity of blood flow in a given area (on average, 5-15 minutes). In this case, about 60-80% of the active substance loses its properties, entering into a biochemical reaction with blood proteins.
The remaining amount of lidocaine goes first to the organs that are most intensively supplied with blood (brain, liver, heart), and then to muscle and fat tissue. After this, most of it is metabolized by the liver with the formation of 2 types of metabolites and removed from the body. A small amount of lidocaine (5% to 20%) is excreted unchanged in the urine.
What else is important to know about breastfeeding after anesthesia
If a nursing mother is planning to undergo surgery, it will also be important to consider a number of issues:
- Is it possible to postpone the operation until the child is older?
- Is it possible to perform the operation on an outpatient basis (one-day surgery)?
- Can the surgery be performed under local or regional anesthesia?
- If the operation or recovery from anesthesia is expected to take a long time, would it be possible to express milk before the operation (and place it in the refrigerator) so that your loved ones can then bottle feed your baby?
- What medications will be used during and after surgery/anesthesia?
Use reference literature to check these medications to see if they can be safely fed to your baby with breast milk. On the following English-language website you can get comprehensive information on this issue: https://toxnet.nlm.nih.gov/cgi-bin/sis/htmlgen?LACT
Here is some information from this site regarding drugs for anesthesia, namely the safety of their use and the optimal time for breastfeeding after anesthesia and anesthesia:
- Halothane (fluorothan), isoflurane, sevoflurane (Sevorane), desflurane, nitrous oxide, thiopental, propofol, etomidate, fentanyl, sufentanil, alfentanil, bupivacaine (Marcaine), lidocaine, ropivacaine (naropine). When using these drugs, breastfeeding can begin immediately after anesthesia.
- Midazolam (dormicum). Some experts believe that it is possible to feed a child no earlier than 4 hours after the last administration of midazolam, taking into account the relatively long time of destruction of the drug in the mother’s blood, some penetration into breast milk, as well as relatively high absorption in the child’s gastrointestinal tract (about 36%).
- Diazepam (Relinium). This drug is excreted from the body for a long time and penetrates well into mother’s breast milk. The recommended feeding time for a child is 6-8 hours after the last administration of diazepam.
- Articaine (ubistesin, ultracaine), mepivacaine, procaine (novocaine), prilocaine, levobupivacaine, benzocaine, remifentanil. The effect of these drugs during breastfeeding has not been studied, so the use of alternative drugs is recommended.
Use during breastfeeding
Any medicine taken by a woman during breastfeeding inevitably enters the child’s body.
The degree of harm it causes depends on:
- drug concentrations in breast milk;
- the mechanism of its action;
- the time required to remove the remaining drug from the mother’s body.
Lidocaine, taking these factors into account, has the following advantages during breastfeeding:
- it enters the internal organs in small doses, since most of it, absorbed into the blood from the injection site, binds to blood proteins. There will be a negligible amount of it in breast milk;
- when used correctly, lidocaine does not affect the functioning of the central nervous system and does not interfere with the functioning of other body systems and cannot harm the baby;
- the duration of action of the drug is usually limited to half an hour: the disappearance of the feeling of numbness means that it has already lost its properties;
- There are lidocaine-based gels intended for children of the 1st year of life, which are used, for example, during the eruption of baby teeth. Its concentration in these products is several times higher than in breast milk after injection of the drug.
Lidocaine can be considered a drug that is safe for both a nursing mother and her baby.
You can reduce the risk of complications by following simple rules:
- Do not try to use lidocaine yourself;
- if it is necessary to perform anesthesia, be sure to notify the doctor about the fact of breastfeeding: then he will use a composition with the lowest possible concentration of the active substance or select a safe method of anesthesia;
- To be on the safe side, skip the next feeding, replacing it with an artificial formula, and express the milk. By the next meal, there will be no likelihood of lidocaine being present in breast milk.
Optimal doses, which virtually eliminate the risk of complications for a nursing mother and infant, depend on the method of anesthesia and the site of drug administration.
In the absence of contraindications, they are:
- 100-200 mg (½ ampoule or 1 ampoule of 10% solution) – for general anesthesia. These are intramuscular injections into the area located next to the nerve fibers through which signals are transmitted from the area that needs to be numbed;
- 40-60 mg (2-2.5 ampoules of 2% solution) - with intramuscular administration of lidocaine, preceding simple operations on the finger, ear, nose;
- 6 drops in each eye (three times 2 drops with an interval of 1 minute) – when performing diagnostic ophthalmological procedures;
- 2-20 ml (1 ampoule of 2% solution) – for thermal anesthesia of the oral mucosa (applications with lidocaine);
- 400 mg – by injection to normalize heart rhythm during arrhythmia. Injections are performed according to the following scheme: first, 50-100 mg of a 2% solution intravenously. The next day, with an interval of 3 hours - 2 injections of 100 mg of a 10% solution intramuscularly.
The maximum safe dose for an adult is 200 mg per day.
After feeding
When the child has been fed after using lidocaine, it is recommended to observe the child and his reactions. Deviations in the baby's behavior are only possible if large doses of analgesics were used during the operation or if the analgesics were reused.
It happens that anesthesia is prescribed not only for dental treatment.
For example, sudden inflammation of the appendix, mastitis and other much more serious operations require anesthesia and the use of stronger drugs.
In such cases, you need to consult your doctor and get answers to a number of questions:
- Is it possible to postpone surgery until breastfeeding stops?
- Is it possible to use local anesthesia instead of general anesthesia?
- After what time is it possible to resume lactation if it had to be stopped at the time of the operation?
It is very important to discuss all questions with the doctor, since there are a number of anesthetics that, if they enter the baby’s body, can cause drowsiness and weakness, disrupt the sucking reflex, disrupt the functioning of the nervous system and liver, and also change the chemical composition of the blood.
If surgery is still necessary, and the use of a more gentle drug for a nursing mother and her baby is impossible, doctors strongly recommend interrupting breastfeeding.
Contraindications
Lidocaine during breastfeeding can harm the woman herself or her baby if there are contraindications to the use of the drug. For this reason, before using it, a tolerance test must be carried out and the medical history must be carefully studied.
Pain relief with lidocaine is not possible under the following circumstances:
- excessive sensitivity to the drug;
- previous adverse reactions to lidocaine;
- liver diseases that prevent the complete metabolism of this substance;
- a number of heart pathologies during exacerbation;
- myasthenia gravis is a neurological disorder manifested by pathological fatigue and weakness of certain muscle groups.
The drug is prescribed with caution to people with:
- existing chronic cardiovascular disease;
- conditions that are accompanied by impaired blood flow in the liver;
- renal dysfunction;
- the patient is over 65 years old.
For the use of plates, sprays and applications with lidocaine, any damage to the skin in the treated area is a contraindication.
During pregnancy, the question of the advisability of using lidocaine should be decided by a doctor, taking into account the following factors:
- the possibility or impossibility of postponing a procedure requiring pain relief to a later date;
- threat to a woman’s health if treatment is refused;
- harm to the unborn child when performing anesthesia.
If there are (if there is a suspicion of) contraindications to lidocaine in an infant, combined with the need for anesthesia for a nursing mother, the doctor, depending on the circumstances, chooses one of the following solutions:
- postpone a procedure that requires pain relief for a while;
- use a different type of anesthetic;
- It is recommended to skip one feeding after the procedure, offering the baby a formula appropriate for his age, and expressing the milk.
When can you start feeding your baby after using lidocaine anesthesia?
The common belief that breastfeeding is prohibited for a long time after the use of local anesthesia is incorrect. Natural lactation and the painkiller Lidocaine are completely compatible, so nursing mothers need not worry at all.
Let's once again give the reasons why lidocaine is safe for hepatitis B:
- only a small amount of this drug reaches the systemic circulation;
- the contents of the medication are quickly eliminated through the kidneys;
- when breastfeeding, the doctor selects a low concentration for a woman;
- if the child is not allergic to the composition of Lidocaine, the residual amount of the product will not harm him;
- Sometimes the anesthetic may wear off before you even get into your home.
Did you know that this drug is also present in children's pain-relieving gels? This once again suggests that the use of this local anesthetic is appropriate.
You can breastfeed your baby immediately after lidocaine.
Let the baby’s age also give you confidence: the older the child, be bolder when treating teeth with this drug.
The question “should I express milk before breastfeeding?” is also relevant for many. You can do without using this procedure. As soon as you feel that the numbness in your mouth has passed, this means that Lidocaine has been removed from both the blood and mother’s milk. It turns out that upon returning home you can already feed the baby. If you are very worried about this, we advise you to stock up on expressed milk for the first time after using the anesthetic.
Overdose
When performing superficial anesthesia, an overdose is practically impossible.
Its concentration in the blood, tissues and internal organs increases with:
- administration of large doses of the drug intramuscularly;
- its repeated use;
- disruption of lidocaine metabolism.
Depending on the injection site, this can lead to the following undesirable effects:
- long-term loss of tissue sensitivity in nearby areas of the body;
- paresthesia: tingling, burning sensation;
- hyperacusis, in which any sound causes pain and discomfort;
- numbness of the tongue, impaired articulation;
- temporary decrease in visual acuity;
- tremor;
- dizziness;
- convulsions;
- cardiac dysfunction;
In severe cases, when high doses of the drug are administered intravenously, apnea and bradycardia may develop. If symptoms of overdose appear, stop administering the drug.
To normalize the patient’s condition, the following means are used:
- relieving cramps;
- supporting the functioning of the heart and lungs;
- accelerating the removal of lidocaine from the body.
External manifestations of an overdose do not require treatment; with a decrease in the concentration of the drug in the body, they gradually weaken and disappear.
If there are signs of an overdose, a nursing mother should temporarily stop breastfeeding, and when it resumes, carefully monitor the baby’s behavior.
Dental treatment and breastfeeding. How to combine?
milkmomstory queen_of_jazz
Nursing mothers often ask questions about dental treatment during lactation.
The lactation consultant's answer: “It is possible, and even necessary, to treat!” Don’t put off solving the issue of your dental health “for later.”
After all, it is easier and faster to eliminate the problem at the initial stage, and advanced cases require more serious interventions!
❔Basic questions about pain relief in the dentist’s chair:
1. Is it possible? 2. How soon can I resume breastfeeding after the procedure? 3. Do I need to express milk?
❗We answer:
1. You can! Don't endure the pain!
Currently, there are many new generation anesthetics that can be used during pregnancy and breastfeeding. They are practically non-toxic and the risk of allergic reactions is reduced to zero. However, we should not forget that an allergy can develop to almost any anesthetic, and if there have been cases of allergy to anesthetics in the past, you should definitely tell your doctor about it.
2. You can feed the baby right away.
The basic rule that applies when using any medications by a nursing mother: the older the child, the lower the level of possible risk for his body, the lower the therapeutic dose per 1 kg of baby’s body weight that reaches him through breast milk.
3. No, it's not necessary.
The drug is practically eliminated from the systemic bloodstream and breast milk as soon as the numbness of the anesthetized area begins to disappear. But while the drug is working, its concentration in the blood plasma and in milk is the same, so expressing milk will not change anything.
What anesthetics compatible with breastfeeding does the dentist use?
: Each type of pain relief corresponds to a specific drug.
✔Short-acting drugs:
Novocaine.
Synonyms: allocaine, gerocaine, kerocaine, meracaine, neocaine, planocaine, polocaine, procaine, paracaine, sevrocaine, sincaine, ethocaine.
Low risk, moderately safe during lactation. It is recommended to monitor the reaction. Anesthetic for topical use in dentistry and dermatology, has virtually zero absorption when used appropriately. It is not recommended for use in the area of the nipple and areola; in case of emergency, use immediately after feeding, rinse thoroughly with water before the next feeding.
✔Medications with an average duration of action (as the degree of risk increases):
Lidocaine.
Synonyms: xycaine, xylodont, xylocaine, lignocaine, lidocaine, luan, octocaine.
Very low risk. Compatible with breastfeeding, regardless of the method of its use: analgesic, antiarrhythmic (duration of action 10-20 minutes), or anti-epileptic. Safe for the child. Passes into breast milk in small quantities, no side effects have been identified. The time to reach the maximum concentration of the drug in the blood plasma is 0.01 hours. As a local anesthetic (in dermatological, dental, ophthalmic and otological preparations) it has almost zero systemic absorption. It is not recommended to use it on the nipples, but if necessary, it is better to do it after breastfeeding, and rinse with water before the next feeding. When used as anesthesia during childbirth, it can cause a delay in the flow of milk (impaired initiation of stage 2 of lactogenesis). It is the main drug included in sprays and gels.
Articaine.
Synonyms: alfacaine, brilocaine, septonest, ultracaine, ubistezin, cytokartin.
Very low risk. Compatible with breastfeeding, safe for the baby. It has a chemical structure similar to lidocaine and passes into breast milk in minimal quantities. Anesthetic for local use in dermatology and dentistry. Has virtually zero absorption when used appropriately. The time to reach the maximum concentration of the drug in the blood plasma is 0.25 hours. Indicated for patients suffering from high blood pressure. Contains the smallest amount of vasoconstrictor components, its duration of action reaches 4 hours.
Mepivacaine.
Synonyms: isocaine, scandicaine, scandonest, mepivastezin, mepidont.
Low risk, moderately safe during lactation. It is recommended to monitor the reaction. The time to reach the maximum concentration of the drug in the blood plasma is 0.5 hours. Mepivacaine is less toxic than lidocaine. It acts for about 20 minutes on the hard tissues of the tooth and about 2 hours on the surrounding soft tissues.
In dentistry, the most common uses are lidocaine and mepivacaine.
✔Long-acting drugs:
Bupivacaine.
Synonyms: anecaine, marcaine.
Very low risk. Compatible with breastfeeding, safe for the baby. A local anesthetic that is used for conduction (infiltration) anesthesia, including epidural anesthesia. Passes into breast milk in small quantities. No side effects were observed in infants whose mothers used bupivacaine. There is a risk to the newborn's ability to breastfeed and a risk of delayed milk supply (impaired initiation of stage 2 lactogenesis) in the mother when bupivacaine is used as an epidural. The time to reach the maximum concentration of the drug in the blood plasma is 0.2-0.5 hours.
(Current data on the compatibility of medications with breastfeeding is provided from the reference book of the Spanish hospital Marina Alta).
Ask us your question about the compatibility of medications (prescribed by a doctor) with breastfeeding, we will try to find an answer. Don't forget to include the baby's age as this information is very important.
The article was prepared especially for MILKMOMSTORY by Veronika Makarova, lactation consultant, Moscow
Source: https://milkmomstory.livejournal.com/58569.html
Side effects
Lidocaine during breastfeeding, when used correctly, has virtually no side effects. However, the likelihood of their occurrence increases if there are contraindications or in case of overdose.
In this case, negative reactions from certain body systems are possible:
- immune: allergy, anaphylactic shock (with repeated administration of the drug);
- nervous: nervousness, increased excitability or drowsiness, tremors, convulsions, loss of control over facial muscles;
- cardiovascular: increased blood pressure, bradycardia, tachycardia, arrhythmia. In severe cases – cardiac arrest;
- respiratory: breathing disorders, bronchospasm, shortness of breath, apnea;
- digestive: nausea, vomiting;
- organs of vision: a feeling of “fog” in the eyes, double vision, sometimes temporary loss of vision, redness of the eyelids, a burning sensation in the eyes;
- hearing organs: extraneous noise in the ears, feeling of discomfort;
- skin: irritation, redness, rash, itching and burning.
Why is lidocaine safe?
It is worth noting that the drug Lidocaine is most common in dentistry. It is the safest. This is because lidocaine:
- is a short-acting local anesthetic;
- has antiepileptic and antiarrhythmic effects;
- characterized by almost zero absorption;
- it enters mother's milk in negligibly small quantities, which will not harm the baby in any way;
- in dentistry it is used in low concentration;
- very rarely has side effects.
An important factor is the absence of an allergy to this drug. In case of individual intolerance, it is important to inform your doctor about this. It is worth concluding that it makes no sense to refuse to use this local anesthesia, due to at least two advantages: Lidocaine will relieve you of the worries associated with tooth pain and will help you quietly cope with the treatment of the problem. Clinics have the opportunity to use the drug in the following ways:
- injection method (infiltration method); - conductive method; - terminal or application method for fear of injections.
The potential harm from the use of Lidocaine during breastfeeding is not comparable to the possible negative consequences of toothache and concomitant diseases.
Drug interactions
External use of lidocaine does not impose restrictions on the use of other drugs.
For intramuscular and intravenous administration, combinations with the following drugs are undesirable:
- Cimetidine and Propranolol, reducing the liver's ability to metabolize lidocaine, lead to an increase in its concentration in the blood. When used together, reduce the dose of lidocaine;
- drugs that slow down the development of HIV infection (antiretroviral) act similarly;
- diuretics, reducing the concentration of potassium in the blood, weaken the effect of lidocaine;
- local anesthetics or antiarrhythmic drugs with a similar mechanism of action, when used together with lidocaine, giving an additive effect, increase its toxicity;
- some antipsychotics taken at the same time as lidocaine increase the risk of developing ventricular arrhythmia;
- Quinupristin and Dalfopristin are antibiotics whose action is based on slowing down the synthesis of proteins necessary for the life of bacteria. They increase the concentration of lidocaine in the tissues of the heart, and also contribute to the appearance of this type of arrhythmia;
- muscle relaxants taken simultaneously with lidocaine will increase the blockade of muscles and nerves, making the loss of tissue sensitivity more pronounced and prolonged;
- Verapamil and Timolol when used with lidocaine can cause cardiovascular failure;
- Dopamine increases the risk of seizures after lidocaine injection;
- antieliptic drugs require, on the one hand, an increase in the dose of lidocaine as an anesthetic, and, on the other hand, they make its antiarrhythmic properties more pronounced;
- the complex effect of sedatives and lidocaine enhances the effect of the anesthetic on the nervous system;
- vasoconstrictors lengthen the time it takes for lidocaine to leave the body;
To feed or not to feed a child after breast anesthesia?
Among inexperienced doctors, there is an opinion that if a woman has been subjected to anesthesia, then after completion of the operation the baby should not be breastfed for a long time, since the anesthetic will be completely eliminated from the body only after a few days.
However, this opinion is wrong, and you can feed the baby as soon as the numbness subsides.
If the numbness has completely passed, the lidocaine is considered cleared from the blood.
If your mother still has doubts, you should pay attention to several more factors:
- The drug is very quickly eliminated from the body through the kidneys.
- If a woman notifies the doctor about her situation, he will select a low concentration of lidocaine for use.
- Often the effect of the anesthetic wears off when you return home from the hospital.
Only a few pain medications pass into breast milk, and then in very small quantities; an even smaller proportion of these drugs can be absorbed in the baby’s intestines. Therefore, most anesthesia drugs are absolutely harmless in terms of the possibility of combining their use and breastfeeding. Including lidocaine.
Analogs
Lidocaine during breastfeeding can be replaced with analogues only after prior consultation with a doctor.
Complete analogues containing lidocaine hydrochloride as the active component are:
| A drug | Description |
| Versatis | The drug is available in the form of plates with a sticky surface. The package contains from 1 to 30 plates. The drug is intended for local anesthesia and is used to alleviate the patient’s condition with neuralgia and muscle pain of unknown etiology. Packaging price for 30 pcs. – from 300 rub. |
| Helikain | Lidocaine-based gel, local anesthetic. The drug is available in tubes with a capacity of 100 or 30 g, packed in cardboard boxes. Used to perform all types of superficial anesthesia in:
urology.
|
| Dinexan | Gel with local anesthetic properties. In addition to lidocaine it contains:
Intended for pain relief of the oral mucosa and can be used:
The drug is sold in tubes of:
|
| Lycaine | A product based on lidocaine hydrochloride is intended for performing all types of local anesthesia for pain of low and moderate intensity. Widely used:
The drug is available in the form:
|
| Luan | Gel, local anesthetic, used mainly when performing endoscopic diagnostic and therapeutic procedures requiring anesthesia, by applying to the mucosa. The drug is available in 2 types, differing in the concentration of the active substance:
|
Lidocaine, when used correctly, is a harmless drug for a nursing mother and her baby. It is not worth refusing anesthesia performed with its help, given that the period of breastfeeding sometimes lasts more than a year. The disease will not wait for its end, causing much more harm than 1 injection of painkiller.
Lidocaine during lactation
According to the instructions, Lidocaine can be used during breastfeeding, but is not recommended. If you experience, for example, toothache, contact your dentist. Lidocaine is often used to treat or remove a diseased tooth. How else can you relieve tooth pain during breastfeeding, see the link https://vskormi.ru/mama/obezbolivayschie-pri-laktacii/.
According to doctors, this anesthetic is relatively safe for lactating women and newborns. This is explained by the fact that the drug acts locally and its duration of action is short. The concentration of the active substance in the blood and breast milk is minimal, and therefore the medication will not harm the baby. The drug should not be used only in case of hypersensitivity to its components.
Feeding can be done almost immediately after the feeling of numbness disappears. This is safe, since the doctor selects the minimum dose of the medicine, which is quickly eliminated from the body. The main thing is to notify the doctor in time that you are feeding your child.
Thus, Lidocaine is allowed to be used during lactation as prescribed by a doctor. A nursing mother should monitor the condition of the newborn after using an anesthetic, as there is a risk of side effects. This is possible in case of individual intolerance to the components of the drug in the infant.
For every mother, the period of breastfeeding is especially exciting. Indeed, at this time, more than ever, it is important to carefully monitor your diet, well-being and medication intake.
Nowadays, not a single mother is immune from diseases. And the range of medications allowed during lactation is small - the baby’s health is also at stake. But enduring pain is also not an option. What to do if a young mother is surprised by a toothache while breastfeeding? Are there medications that are taken during lactation? Should I endure it, gritting my teeth, or go to the dentist and get treatment without the use of anesthetic anesthesia?
Lidocaine is an approved painkiller for breastfeeding for minor surgical procedures.