2686
Edentia or absence of teeth in both jaws is a fairly common situation that can occur not only in elderly patients, but also in fairly young people.
This pathology requires immediate elimination, both due to the lack of aesthetics of the oral cavity and due to the possibility of developing a large number of complications.
However, to choose the right treatment tactics, a specialist needs to correctly study the structural features of the patient’s jaw with missing teeth, which is greatly simplified when using the classifications of toothless jaws available in dental practice.
Schroeder separation
Classification of toothless upper jaws is made according to the degree of atrophy (reduction) of the alveolar processes (parts of the jaw that bear teeth). The scientist identified three types.
The first is characterized by pronounced areas of anatomical retention (the structure of the bed that ensures the retention of the prosthesis). In Schroeder’s classification of toothless jaws, in particular, the first type of atrophy includes:
- The presence of a high palatine vault.
- Pronounced jaw cusps and alveolar process.
- Highly located areas of fixation of folds of mucous membrane and muscle fibers.
These manifestations do not create obstacles to the installation of a prosthesis. Moreover, in Schroeder’s classification of toothless jaws, this type is considered the most favorable for prosthetics.
With a moderate degree of atrophy of the process, they speak of the second type of jaws. The cusps of the upper jaw are preserved, and the arch of the palate is clearly defined. The transitional fold is located slightly closer to the apex of the process than in the first type. A sharp contraction of the facial muscles can lead to disruption of the fixation of the prosthesis.
The third type of jaw is characterized by significant atrophy. The palate is flat, and the tubercles and alveolar processes are absent. The transitional fold is in the same plane as the hard palate.
Prosthetics of such a jaw is accompanied by significant difficulties. Fixation of the prosthesis is almost impossible.
Types and features
There is still no single comprehensive classification of toothless jaws. This is due to the fact that in addition to the marginal forms of jaws named in the known groups, there are many transitional types that have certain structural features.
Currently, the most popular are five groups of toothless jaws, named after the developers.
What is the purpose of relining a removable denture and the material used.
Let's calculate here how much dentures with suction cups cost.
According to Schroeder
According to Schroeder's classification, the upper jaw rows with missing teeth can be divided into three types, which is due to different levels of bone depletion in the alveolar area:
- I jaw involves insignificant thinning of the tooth-bearing area. In this situation, the cusps of the jaw and the areas of the upper row, designed to hold the teeth, are clearly visible, and the palatine vault is deep.
The folds of the mucosa and the areas of muscle attachment are located quite high. According to experts, this type of jaw row is the most desirable for installing a prosthetic structure, because its elements do not interfere with the attachment of artificial teeth. Type II is recognized when there is an average level of thinning of the alveolar process and its not very clear expression. The patient has moderate depth of the palatal plane.
The transitional fold is shifted towards the alveolar ridge. When attaching a prosthesis for this type of jaw, there are risks of reducing the quality of its fixation as a result of spasms of facial muscles. Type III is indicated by an excessive level of atrophy of the bony base of the jaw. Alveolar ridges and tubercles are completely smoothed. The palate takes on a flat shape.
The mucosal fold is located low in the same plane as the palate. When placing dentures, this jaw shape causes the most difficulties, which is associated with high mobility of the structure as a result of the anatomical features of the elements of the dentition.
According to Keller
According to experts, the lower jaw causes more difficulties in prosthetics than the upper jaw. This is due to its anatomical and physiological characteristics.
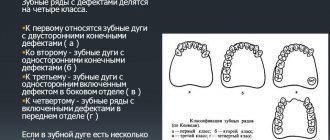
To simplify the process of restoring elements of the lower jaw row, the Keller classification was developed, which assumes that the patient may have one of four types of jaw:
- The first type of lower dentition involves slight atrophy and uniform smoothing of the alveolar parts.
This creates an ideal basis for fixing the prosthetic structure and prevents it from moving forward and in different directions.
The attachment of the folds of the mucous membrane and muscles is located in the base of the alveolar region.
Dentists note that this option occurs quite rarely in patients, mainly with the simultaneous extraction of teeth and a slow process of thinning of bone tissue. The second form of the jaw is characterized by a uniform and clearly defined atrophic process occurring in the alveolar area.
The ridge stands out slightly against the background of the floor of the oral cavity, but has a rather sharp surface, which complicates the procedure for fixing the prosthesis.
The muscles in this case are attached in the area where the alveolar ridge is located. Due to the anatomical structure of the jaw, the use of a prosthesis often causes pain and discomfort due to the possibility of its displacement. Dentists identify the third type of jaw It is characterized by thinning of the alveolar process in the area of premolars and molars, while maintaining the volume of bone tissue in the central sections.
Prosthetics with this classification option is considered acceptable, since in the lateral sections of the dentition there are smooth surfaces suitable for fixing artificial molars.
In addition, maintaining the alveolar cusp in the central section prevents artificial teeth from sliding forward under load during chewing. The fourth form of jaws without teeth according to Keller’s classification involves severe atrophy of the alveolar area in the area of the frontal incisors.
At the same time, in the lateral areas of the dentition, bone tissue is preserved much better. Fixation of the prosthesis in this case is not very reliable, since the structure may lose stability and shift.
According to dentists, fixing the prosthesis on the lower jaw is acceptable for each of the Keller classification options, however, for the second and fourth types of dentition, it causes many difficulties associated with the structure of the oral cavity.
Lower jaw
Its anatomical and physiological characteristics differ significantly from the characteristics of the upper jaw. As experts note, the conditions for the manufacture and subsequent use of removable dentures are less favorable.
The classification of edentulous lower jaws is characterized by 4 types. It was proposed by L. Keller.
With the first type of jaw, the alveolar processes atrophy slightly and evenly. Due to the evenly rounded ridge, placement of the prosthesis is not accompanied by difficulties. Shift of the product to the sides and forward is practically excluded.
At the base of the alveolar processes there are areas of attachment of folds of mucous membrane and muscles.
This type, in accordance with Keller’s classification of classes of toothless jaws, occurs with simultaneous removal of teeth and slow atrophy of the alveolar part. It is considered the most convenient for prosthetics.
The second type in Keller’s classification of edentulous jaws is characterized by pronounced, but uniform atrophy of the alveolar processes. This part rises above the floor of the mouth. In the anterior section, the alveolar part appears as a narrow, in some cases sharp, formation. It is of little use for installing a prosthesis.
The areas of muscle attachment practically coincide with the level of the apex of the alveolar part.
On this type of jaw, prosthetics are difficult, as there are no conditions for anatomical retention. In addition, due to the high location of muscle attachment sites and the absence of a transitional fold, the prosthesis moves when the masticatory muscles contract. Using the product is often accompanied by pain. Successful prosthetics in some cases can be achieved after smoothing the sharp edge of the mylohyoid line.
The third type is characterized by pronounced atrophy of the alveolar processes of the lateral part with a relatively normal state in the anterior part. This situation occurs in the case of early removal of chewing teeth.
The third type of jaw is considered relatively favorable for prosthetics. Between the mylohyoid and oblique lines in the lateral sections there are flat, almost concave surfaces. They are free from muscle attachment sites. The alveolar part of the anterior section prevents displacement of the prosthesis.
The fourth type of jaws is characterized by pronounced atrophy of the anterior part of the alveolar processes with their relative preservation in the lateral sections. Because of this, the prosthesis slides forward, losing support.
Changes in the mucosa
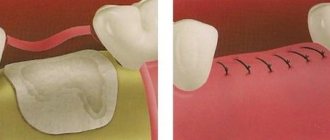
The emerging changes that develop in the oral cavity after teeth have been removed begin to involve not only the alveolar processes, but also spread to the mucous membrane that covers them and the hard palate.
These changes can be expressed in the form of atrophy, and folds may also form. In this case, the location of the transitional fold relative to the crest of the alveolar process changes. The essence and stage of these modifications can be explained not only by the loss of teeth, but also by the reasons that became the basis for their removal.
Division of jaws by I. M. Oksman
This scientist characterized both the upper and lower jaws. The unified classification of toothless jaws according to Oxman involves division into 4 types.
Upper jaws:
- The first type is established for jaws with a high alveolar process, high maxillary cusps and the location of the attachment areas of the buccal cords, frenulum and transitional fold, a pronounced palatal vault.
- The second type is diagnosed with moderate atrophy of the maxillary tuberosities and alveolar processes, a shallower palate, and lower attachment of the mobile mucosa.
- With the third type, there is a sharp and at the same time uniform atrophy and flattening of the arch. The mucosa is attached at the level of the apex of the process.
- The fourth type is diagnosed with uneven atrophy. It combines the characteristics of all other species.
The lower jaws are also divided into 4 types. According to Oxman’s classification of toothless jaws, they have the following characteristics:
- Type 1 – high alveolar process, low location of the transitional fold and areas of fixation of the buccal folds and frenulum.
- Type 2 – uniform, moderate atrophy.
- Type 3 – the alveolar process is weakly expressed or completely absent. In this case, atrophy can spread to the body of the jaw.
- Type 4 – uneven atrophy. It occurs when teeth are removed at different times.
Kurlyandsky classification (for edentulous upper jaw) (1955)
Type 1: high, pronounced alveolar ridge and pronounced tubercles of the upper jaw, evenly covered with a dense mucous membrane. Deep palate, unexpressed or absent torus, the presence of a large mucoglandular cushion over the aponeurosis of the muscles of the soft palate.
Type 2: average degree of atrophy of the alveolar ridge, mildly expressed tubercles, average depth of the palate, pronounced torus, average pliability of the mucous membrane and mucoglandular cushion under the aponeurosis of the muscles of the soft palate.
Type 3: sharp atrophy of the alveolar ridge, sharply reduced size of the body of the upper jaw, unpronounced tubercles, shortened anteroposterior size of the hard palate, wide torus, narrow strip of the neutral zone along line “A”.
Kurlyandsky classification (for edentulous lower jaws) (1995) The first type - the alveolar process protrudes above the level of the attachment points of the muscles of the internal and external sides.
The second type - the alveolar process and the body of the jaw are atrophied to the level of the muscle attachment points on the inner and outer sides.
The third type - atrophy of the jaw body has passed below the level of muscle attachments on the inner and outer sides.
The fourth type is large atrophy in the area of the chewing teeth.
The fifth type is large atrophy in the area of the front teeth.
If we compare the classifications of Keller and Kurlyandsky, then the third type of atrophy according to Kurlyandsky can be placed between types 2 and 3 according to Keller: atrophy occurred below the level of muscle attachments on the inside and outside. 69. The doctrine of fixation of the prosthesis and stabilization on toothless jaws, their determining factors. The concept of adhesion and functional suction.
Fixation
- this is keeping the prosthesis on the jaw at rest, and
stabilizing it
during operation. The strength of fixation of the prosthesis depends on the anatomical conditions present in the patient’s oral cavity, the type of mucous membrane and the method of obtaining an impression.
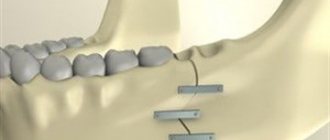
Boyanov proposed to distinguish mechanical, biomechanical, physical and biophysical methods of fixation. Mechanical methods were developed at the beginning of the last century by Fauchard and consisted of the use of various springs. Biomechanical methods involve fixation of prostheses using subperiosteal and intraosseous implants, as well as surgical plastic surgery of the alveolar processes in order to create conditions for anatomical retention. When applying physical methods, physical phenomena were used as a means of strengthening dentures on toothless jaws. This method was based on the use of magnets, rarefied space and weighting of the lower prosthesis. A physical and biological method for fixing dentures on toothless jaws was proposed by Kantorovich. The essence of this method lies in the design of the boundaries of the prosthesis, taking into account the functional state of the adjacent mobile soft tissues (biological prerequisites), as well as in the use of physical phenomena that occur in the oral cavity, in particular the phenomena of adhesion and capillarity. These phenomena ensure functional suction of the prosthesis.
The functional suction of the prosthesis is achieved due to the formation of a continuous circular valve around its edges within the transitional fold. The mucous membrane of the transitional fold, due to its mobility, is able to follow the shifts of the prosthesis during chewing and speech, which maintains the continuity of the circular valve and prevents air from penetrating under the prosthesis.
.Adhesion
- a force that causes two substances to stick together and is the result of intermolecular interaction. In the case of accurate display of the macro- and microrelief of the mucous membrane on the basis of the prosthesis, a condition is created in which molecular adhesion forces arise between two congruent surfaces, separated by a thin layer of saliva, helping to keep the prosthesis on the jaw. The quality of saliva and the size of its layer play an important role in the manifestation of adhesion.
The adhesion of the prosthesis is also based on the universal physical phenomenon of wettability, which occurs when the molecular adhesion forces are less than those that exist between the molecules of a liquid and a solid. The prosthesis and mucous membrane are well moistened with saliva, resulting in a concave meniscus. The force with which he tries to straighten is directed outward and acts like a suction pump, pressing the prosthesis against the mucous membrane of the hard palate.
Functional suction is based on the difference in atmospheric pressure outside the prosthesis and under the prosthesis. To explain this, the concept of the valve zone was introduced.
Valve zone
- this is the zone of tight contact of the mucous transitional fold, line "A", the bottom of the mouth with the edge of the prosthesis, which exactly follows the contours of the vault of the oral cavity during all functional movements of the lower jaw, lips, tongue and cheeks. To form a circular valve, the prosthesis must overlap the valve zone by 1 -2 mm. In this case, a space with rarefied air will form between the prosthesis and the underlying mucous membrane, and the prosthesis will be well fixed due to the difference in atmospheric pressure. In the clinic this is achieved:
— precision manufacturing of the length of the edges of the rotes;
- volume of edges;
- some pressure of the edge of the prosthesis on the underlying tissue.
The conditions for fixing the prosthesis on the upper toothless jaw are more favorable than on the lower jaw. The prosthetic bed of the upper jaw has a large area, and the valve zone passes close to the organs with a relatively small subvexity. In contrast, in the lower jaw the area of the prosthetic field is smaller than in the upper jaw, which reduces the width of the valve zone. A tongue with loss of teeth loses support, changes shape and occupies part of the prosthetic field, pushing the prosthesis. With significant atrophy of the alveolar part, the muscle attachment points approach the zone of the closing valve, which, during the movement of the tongue and lower jaw, leads to displacement of the prosthesis from its bed.
The boundaries of the valve zone are determined and formed on an individual impression tray directly in the patient’s mouth, taking into account the topography and function of the masticatory and facial muscles surrounding the prosthetic field. An individual impression tray is made according to the jaw of the prosthetic patient and allows for a more accurate representation of all anatomical landmarks that are important for high-quality production of prostheses
70. Individual spoons. Manufacturing methods.
Individual trays are made in a dental laboratory as directed by a doctor from wax, plastic, sheet polystyrene or plexiglass on a plaster model obtained from an anatomical cast (impression). The quality of impression materials can be gypsum, elastic impression (impression) and thermoplastic materials.
Individual wax spoon . The boundaries of the future tray are outlined on the plaster model, a plate of dental wax is heated, folded in half and pressed tightly onto the model, giving it the shape of an impression tray. excess wax is cut off with a heated spatula along the marked border, the spoon is removed and its edges are melted on an alcohol lamp or gas burner. To increase the strength of the spoon and ease of use in the mouth, bend a handle from aluminum wire 1 mm thick in the shape of the letter P, no more than 1 cm, spread the ends of the wire in different directions according to the shape of the spoon, heat the ends of the wire over a flame and insert the handle according to the center of the alveolar process at an angle of 90. A custom wax tray can be made with a backing that provides space for the impression material. To do this, crimp the model along the outlined boundaries with one layer of softened wax, cut off the edges, grease the outer surface with Vaseline and make an individual wax spoon on this layer using the method described above. To obtain an impression, the first layer is removed from the tray and an impression mass is applied in its place. Using a custom wax tray, you cannot make an impression under pressure. For this purpose, you need a rigid (plastic) custom-made impression tray.
Individual spoon made of plastic . Using a plaster model, a spoon is made from wax, a small (up to 1 cm) handle is modeled from wax in the area of the front teeth, a model with a wax spoon is plastered into a cuvette, the wax is melted, replaced with plastic, polymerized, processed, but not polished. You can make a spoon from self-hardening plastics (protacryl, carbondent, redont) by free molding and polymerization under pressure in water at room temperature. Plastic dough is prepared according to the previously described method, which is rolled out on a polyethylene plate with a glass rod to a thickness of 4 mm. A shape corresponding to the shape of the upper or lower toothless jaw is cut out from the resulting plate with a spatula. The resulting plate is placed on a model with an insulating layer of “Isokol” applied and molded. Hardening of the plastic is accompanied by an exothermic reaction, which causes small deviations of the plastic dough from the plaster model along the peripheral edge of the spoon. At this point, you need to re-crimp the edges of the spoon. To avoid deformation of the spoon, it is recommended to carry out polymerization in water at room temperature under pressure. An individual spoon can be obtained from a standard AKR-P plate, which is softened in hot water and crimped according to the model. In the case of premature hardening, the unformed section of the plate is again softened and re-crimped according to the model. Excess I/J strips are cut with scissors along the marked boundaries. A handle is made from the remains of the plate using a very heated spatula. From a polystyrene or plexiglass plate up to 3 mm thick, you can make an individual impression tray directly on a plaster model in a pneumatic press with a heater (PPS-l) and a dry-air polymerizer (PS-l).
After fitting the spoon, the doctor, depending on the pliability and mobility of the mucous membrane of the prosthetic bed, takes a functional impression using elastic materials (thiodent, sielast), hardening materials (dentol, repin, gypsum) or thermoplastic masses (MST-02, etc.).
After receiving a solid functional cast, it is edged with plaster. The edging is necessary to maintain the volume of the edge of the prosthesis to ensure closure of the valve during function. Edging is carried out as follows. Using a chemical pencil, at a distance of 2-3 mm from the outer edge of the cast, mark a line along which a pre-prepared edging roller made of wax 2-3 mm thick is attached with molten wax.
When the model is received, the trace from the edging will preserve the outer boundaries of the neutral zone, necessary for the formation of the valve zone. The edging helps protect the dental technician from violating the neutral zone boundary when opening a plaster model cast from a functional cast, which the doctor obtained using functional tests.
Alternative division
There is also a classification of toothless jaws according to Kurlyandsky. He divided jaws into types not only according to the degree of loss of bone tissue in the alveolar part, but also according to changes in the topography of the fixation of muscle tendons.
In accordance with the classification of toothless jaws proposed by Kurlyandsky, there are 5 types. The third type can be considered intermediate between types 2 and 3 described by Keller.
It was already mentioned above that not a single classification allows us to provide for the entire variety of atrophy options. For the quality use of dentures, the relief and shape of the alveolar ridge are also important. The maximum stabilization effect can be achieved with uniform atrophy.
In Courlandic
In 1955, V. Yu. Kurlyandsky formulated a classification of jaws without teeth, which takes into account the degree of atrophic changes in bone structures in relation to the topical features of muscle attachment. He identified 5 maxillary types:
- I. The upper part of the alveolar process protrudes above the site of attachment of muscles from the vestibular and palatal surfaces.
- II. The ridge and the jaw itself are reduced in volume, reaching the site of attachment of muscles from the vestibular and palatal surfaces.
- III. Atrophic jaw changes below the points of muscle attachment.
- IV. Significant atrophic process in the area of molars and premolars.
- V. Significant atrophic process in the area of incisors and canines.
Classification of impressions of edentulous jaws
It can be carried out according to two criteria: the height of the edges and the degree of squeezing of the mucous membrane.
According to the first criterion, anatomical and functional impressions are classified. A subtype of the latter are functional suction impressions.
Depending on the degree of squeezing of the mucous membrane, loading (compression) and unloading types of impressions are distinguished. Let's look briefly at each of them.
Pros and cons of prints
Some experts are against the use of unloading impressions. This position is based on the fact that all chewing pressure falls on the alveolar process. In this regard, its atrophy begins.
Dentures made using compression impressions rest on the tissues of the buffer areas, like cushions. In this case, the alveolar process remains unloaded. When chewing under pressure, the vessels of the buffer area are emptied of blood. The prosthesis puts pressure on both the buffer zones and the process. As a result, the latter does not atrophy.
Types of impressions
An impression is usually understood as a negative (reverse) imprint of the tissues of the area of future prosthetics. Impressions are necessary for the production of prosthetic elements based on them. There are two types of prints according to the height of the edges:
- Anatomical – an impression with high edges, which is taken with standard impression trays without holes and large volumes of plaster. This option does not take into account the condition of the tissues located next to the prosthetic bed (a complex of structures in direct contact with the prosthesis).
- Functional – an impression with low edges, formed using a custom tray and moderate volumes of dental plaster. During its production, specially designed functional tests are carried out, reflecting the mobility of integumentary tissues. The mucosal overlap of the finished prosthetic structure is less than 2 mm.
A type of functional impression is the functional suction subtype. It can also be removed with a functional spoon, but has a higher edge and covers the area outside the prosthetic bed by a couple of millimeters.
Based on the degree of pressure on the integumentary tissue, functional impressions are in turn divided into subtypes:
- Unloading - imprinted with plaster with virtually no pressure, which is achieved using a special structure of the spoon: excess plaster comes out of the holes on the palatal side under pressure. This allows you to minimize the pressure of the future prosthesis on the mucous membrane;
- Compression – used for mobility of integumentary tissues. This impression is taken using alginate, thermoplastic, and silicone masses; gypsum is rarely used. It is removed under pressure with a spoon without holes.
- Combined - relevant for varying degrees of mucosal compliance in different areas. In certain areas, the impression is taken under pressure, in others - practically without.
At first glance, unloading impressions seem to be more physiological and comfortable for the patient, but many specialists do not recommend their use. This is due to the fact that when chewing, the alveolar process takes on the entire load, which gradually atrophies against this background. When using a prosthesis created on the basis of compression impressions, chewing puts a relatively uniform load on the buffer areas, which are emptied of blood at this time, and on the process, so atrophy does not occur.
Doynikov classification
It is based on the unevenness of atrophy. Doynikov identified 5 of its degrees:
- 1 – on the lower and upper jaws, the alveolar ridges are well defined; they are covered with slightly pliable mucous membrane. Its natural folds are somewhat distant from the apex of the process and the alveolar part. The mucous membrane evenly covers the palate. Jaws of this type are considered convenient for prosthetics, including when using products with a metal base.
- 2 – average degree. The maxillary cusps are moderately pronounced, the depth of the palate is average. The palatine torus (bone elevation, thickening of the palatine suture) is well defined.
- 3 – the alveolar part and process are completely absent, the body of the jaw and the maxillary tubercle are sharply reduced, the torus is wide, the palate is flat.
- 4 – the alveolar ridge is expressed in the anterior section. Significant atrophy is noted in the lateral areas.
- 5 – in the lateral sections the alveolar ridge is pronounced, in the anterior section there is significant atrophy.
This classification is considered the most convenient in the practice of an orthopedic surgeon, since it covers the maximum number of cases and characterizes the picture of not only the degree, but also the localization of atrophy. Meanwhile, practicing specialists use all known classifications in their work. This allows you to select prosthetics tactics as accurately as possible.
Mucous membrane of the prosthetic bed
It is characterized by the degree of pliability, sensitivity and mobility. There are three types of mucosa:
- Normal. It is characterized by moderate pliability and good moisture. The mucous membrane has a pale pink color. It is considered the most favorable for installing a prosthesis.
- Hypertrophied. When palpated, the mucous membrane is loose, with a high content of intermediate substance. Features good hydration. With this type of mucosa, it is not difficult to create a valve, but the prosthesis will be mobile due to the pliability of the membrane.
- Atrophied. This mucous membrane is distinguished by its high density and whitish color. The shell is dry. It is considered the most unfavorable for the installation of a prosthesis. The mucous membrane covering the maxillary alveolar process is immovably connected to the periosteum. Almost along its entire length it consists of its own layer and flat multilayered epithelium. On the latter, in the area of the process, there is a stratum corneum.